Advantages and features of CT
In terms of information content, CT is not inferior to MRI. Moreover, computed tomography is preferable for assessing the condition of bone tissue. Also, CT becomes the method of choice if the patient has such contraindications to MRI, such as the presence of metal foreign bodies, implants, etc. in the body.
X-ray and ultrasound compared to computed tomography are less accurate and not always reliable. In addition, the radiation dose from a CT scan is significantly lower than from a traditional X-ray examination.
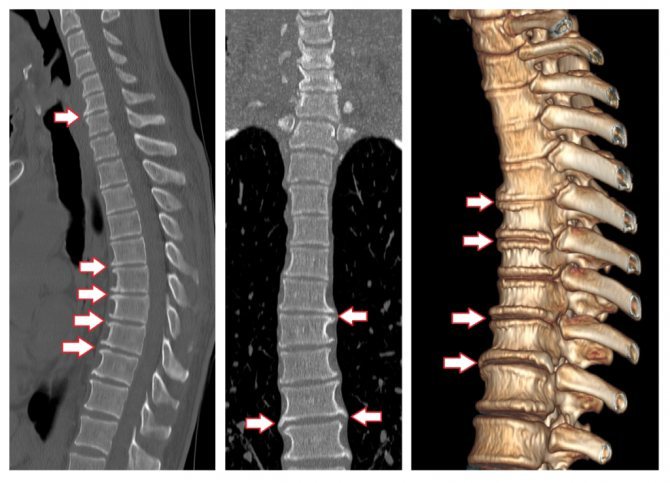
Spinal osteomyelitis
Osteomyelitis is a relatively rare and difficult to diagnose inflammatory disease of the vertebral bone tissue. It begins with damage to the bone marrow and then spreads to other components of the bone tissue. Leads to destruction of the vertebra with subsequent deformation of the entire spinal column.
Osteomyelitis develops against the background of other diseases. In this regard, the following varieties are distinguished:
- Tuberculous osteomyelitis;
- Luetic spondylitis (complication of syphilis);
- Typhoid osteomyelitis;
- Rheumatic osteomyelitis, etc.
This disease is characterized by local back pain - from such a symptom it is impossible to suspect an inflammatory process and distinguish it from other degenerative-dystrophic diseases of the spine. On tomograms, doctors see a set of symptoms indicating a specific clinical picture of osteomyelitis: foci and abscesses of infection that spreads through the intervertebral disc, erosion (thinning) of the intervertebral disc, destruction of the vertebral bone body with a change in its height.
CT scans also help diagnose other inflammatory diseases of the spine, such as spondylitis and discitis.
Indications for CT scan of the lumbosacral region
Even the slightest damage to the lumbar and tailbone area, as a rule, negatively affects physical activity and well-being. The most common symptom accompanying most spinal diseases is pain. Painful symptoms can be caused by:
- spinal injuries;
- protrusion, herniated intervertebral discs;
- lumbosacral osteochondrosis;
- pinched nerve;
- spondylosis;
- congenital anatomical pathologies;
- hemorrhage in the spinal cord;
- tumor neoplasms.
Computed tomography allows you to clearly visualize ligaments and intervertebral discs, shows the condition of the spinal cord and spinal canal, and identifies almost all diseases associated with pain in the lower back and sacrum.
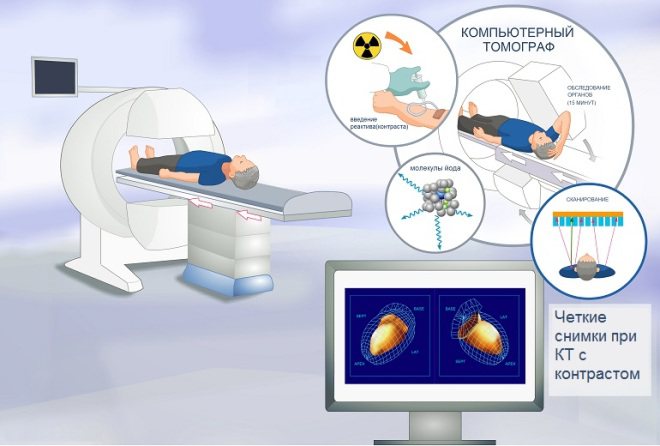
To improve the quality of the images, a CT scan with contrast may be prescribed. Iodine-containing preparations can enhance the absorption of x-rays by tissues. This improves the clarity of pictures.
Degenerative diseases of the spine
Common causes of chronic back pain include a large group of degenerative diseases of the musculoskeletal system. Those detected on CT include:
- Osteochondrosis;
- Osteophytes;
- Osteomyleitis;
- Spondyloarthrosis;
- Osteoporosis;
- Degenerative spondylolisthesis.
Osteochondrosis
Osteochondrosis is the collective name for degenerative diseases that lead to the destruction of intervertebral discs and chronic back pain. Presumably, osteochondrosis occurs due to infections, inflammation, heredity, hormonal disorders, a sedentary lifestyle, and improper physical activity. Osteochondrosis can lead to intervertebral disc herniation, sequestration, and even disability of the patient. On CT scans of the spine, the doctor will see which intervertebral discs are damaged. They can be located at any level: from C1 to L5 , where:
C is the cervical spine;
Th— thoracic spine;
L - lumbosacral spine.
It is important to understand exactly which segment is damaged or causing pain. To restore damaged vertebrae, injection techniques are used, for example, therapeutic blockades and plasma lifting. The attending physician must determine the exact site of administration of the drug.
Osteoporosis
Osteoporosis is a disease associated with bone decalcification. As a result, the vertebrae become very fragile, and CT scans can determine that their structure has become porous. A diagnosis of osteoporosis is associated with a poor prognosis—an increased risk of fractures and injuries. Osteoporosis is most often diagnosed in older people and women after menopause due to hormonal changes.
Osteophytes and spondylosis
Osteophytes are pathological growths of bone tissue that cause painful compression of nerve fibers, blood vessels, and soft tissues. Osteophytes cause discomfort and impede movement, and they arise due to a disturbance in calcium metabolism in the marginal area of the bone, thereby deforming the skeleton.
Osteophytes may not cause severe discomfort, but medical practice shows that the detection rate of this pathology in men and women over the age of 50 with concomitant spinal diseases (intervertebral hernia, osteomyelitis, spondylosis) is approximately 80% and 60%, respectively. Before spine surgery, neurosurgeons often refer patients for a CT scan to check the vertebral bodies for osteophytes and their location, since this will determine surgical tactics.
Facet syndrome
Spondyloarthrosis (facet syndrome) is an inflammation of the intervertebral joints of the spine, which is preceded by disc degeneration. The detection rate of pathology in patients with pain in the lower back, neck and thoracic spine is up to 40%. The pain syndrome also spreads to other parts of the body: face, ribs, hips - depending on the location of the inflammation.
Spondylolisthesis (spinal segment instability)
Degenerative spondylolisthesis is a pathological displacement or slipping of the upper vertebra onto the underlying one. Using computed tomography, the angle of displacement is determined and the degree of trauma is assessed (described in detail in the conclusion). Facet syndrome occurs due to injuries, bone defects, unsuccessful operations, and congenital structural features of the skeleton. Displacement of the vertebrae is best visualized on CT, but the attending physician may recommend that the patient undergo an MRI of the spine.
Contraindications
Computed tomography is contraindicated in pregnant women, patients weighing more than 150 kg, and people with severe mental disorders. For children, the procedure is prescribed in emergency cases strictly according to indications. CT with contrast is not allowed for people with an allergy to iodine, impaired liver and kidney function, or severe diabetes mellitus. Lactation is not included in the list of contraindications, however, after the examination, the woman will have to skip breastfeeding twice, since contrast agents penetrate into the milk.
What affects CT?
The following may prevent you from getting a CT scan or change the test results:
- Pregnancy. CT scans are not usually performed during pregnancy.
- Barium was used for another test. Barium is detected on CT scan. If a CT scan of the lower back is required, this should be done before any procedures that use barium.
- Metal objects in the body. These objects, such as surgical clamps or metal prosthetic joints, can interfere with a clear view of an area of the body.
- The patient cannot lie still during the examination.
How the research works
During the scan, the patient is placed in the tomograph tunnel. Before doing this, he needs to remove all metal objects. When the tomograph ring rotates around the extendable table, numerous layer-by-layer images are created. To ensure that the images are not distorted, you must remain still during the procedure. The procedure is absolutely painless and lasts from 5–10 minutes to half an hour (for examination with contrast).
After the scanning is completed, the resulting images are processed on a computer, deciphered by specialists and given to the patient along with a medical report.
Preparation and conduct of the survey
CT scans are sometimes performed using a contrast agent, an iodine-based solution. It is injected into the bloodstream through a vein or into the spinal canal before the scan begins to clearly see the area being examined. Before such a study, the patient must abstain from food and drink for 5 hours. It is advisable to find out in advance how the scan is done.
CT scan without contrast agent does not require preliminary preparation. They take with them the results of previous research, remove jewelry and other metal objects, since their image is superimposed on the photographs. If foreign objects are installed in the body (implants, staples, pacemakers), be sure to inform the doctor about this.
The patient is placed on a special movable table, which slides into the annular part of the tomograph during scanning. To prevent a person from moving, their arms and legs are secured with belts. The patient is advised to take a comfortable position so that he can lie on the couch without unnecessary movements. A patient with severe back pain is given analgesics to help him lie still and not move during the examination. People with increased nervous excitability are given sedatives.
When contrast is used, a special injector injects a solution into the patient's circulatory system. At the time of injection, a person feels nausea, a salty taste in the mouth and a spreading warmth throughout the body. There is nothing wrong with this: after 10–15 seconds everything returns to normal. In rare cases, the patient develops an unpredictable allergic reaction in the form of itchy skin or difficulty breathing. Medical personnel are ready for this and will provide the necessary assistance in a timely manner.
The doctor sits in the next room and operates the scanner. The patient is under constant supervision of a specialist, since there is a window between the rooms. During the scan, staff may ask you to hold your breath. Any signs of discomfort should be reported to the radiation technologist immediately. If the examination is performed on a child, parents can be next to him in special protective aprons.
The procedure is painless and takes 10–15 minutes, with contrast – up to ½ hour.
CT diagnostics in Moscow
At the Central Clinical Hospital of the Russian Academy of Sciences, all examinations are carried out under the supervision of experienced, highly qualified doctors. Modern equipment meets all international standards. Patients are offered diagnostic procedures in comfortable conditions at one of the most affordable prices in Moscow. If pathological processes are detected, treatment in the clinic’s hospital is possible.
To register for an examination at the Central Clinical Hospital of the Russian Academy of Sciences and clarify the cost of the lumbosacral CT service in Moscow, you can call or use a special form on the website.
CT or MRI of the lumbar spine
MSCT is based on the action of x-rays; they are absorbed by body tissues. The intensity of this process depends on the density of the structure of the studied area. Magnetic resonance imaging is carried out based on the operation of the magnetic field, which affects the location of water dipoles in tissues.
With any type of tomography, many layer-by-layer images are obtained in three mutually perpendicular projections. The technique helps to obtain photographs of thin sections of the tissues being studied, which gives an idea of any changes in the shape and structure of the object being studied.
If you need to check the condition of the hard elements of the spinal column, it is more advisable to use a lumbar CT scan. As a result of the study, MSCT will show inflammatory processes, cracks, fractures, displacements, and neoplasms of dense tissue. An MRI will show the condition of the ligaments, muscles and other soft elements of the area being examined.
CT and MRI of the lumbosacral spine, performed with the use of a contrast agent, will help assess the quality of blood supply to tissues in this area, identify the presence of tumors and morphological changes.
Magnetic resonance imaging is safe for the patient. But the prices for MRI are much higher than the cost of computed tomography, so the choice of diagnostic method in each case is individual, depending on the presence of contraindications and indications for the study.
Decoding the results obtained
In order to make a diagnosis using computed tomography data, it is necessary to describe the pathological changes that are present in the obtained images. A radiologist or radiation diagnostics doctor is engaged in decoding. Any information about previous examinations and treatment that the patient can provide can help the doctor. After decoding, the patient receives photographs on digital media or printed on film, as well as a doctor’s report certified by signature and seal.
What is the difference between a CT scan and a CT scan of the spine?
This is not to say that the general CT procedure is significantly different from a CT scan of the spine. The only difference may be if the procedure is performed on the lower parts of the spinal column. Bowel preparation may be required to ensure optimal visibility. Before the study, you need to exclude foods that affect gas formation from your diet. If the problem persists, you need to take Espumisan. To reduce intestinal motility during the study, the patient is prescribed No-shpa.
What does it show?
- development of degenerative processes;
- foci of inflammation;
- primary and secondary malignant tumors;
- abnormal neoplasms of a benign nature;
- foreign objects;
- compression and trauma-induced fractures, dislocations, ligament ruptures;
- internal bleeding;
- spinal cord compression;
- destruction of the vertebrae due to infections or cancer;
- disturbances in the stability of the structural elements of the musculoskeletal system;
- hernias;
- spondylosis and spondyloarthritis;
- blockage of the spinal canal.
CT and MRI: which is better?
Along with CT scanning, MRI (magnetic resonance imaging) is often recommended. This procedure is based on the use of a magnetic field that affects hydrogen atoms located in the human body.
As a result, electromagnetic pulses are generated, which are captured by the tomograph antennas and sent to a computer for subsequent processing.
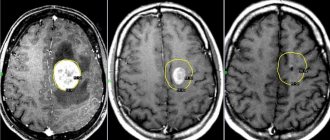
The techniques scan different types of tissue. For example, organs with a high concentration of fluid (spinal cord, brain) are better shown by MRI; hard tissues - bones, vertebrae - are scanned more thoroughly by CT.
Which procedure to perform in a particular case is determined by the attending doctor, based on the patient’s health condition.
Despite the relatively high safety for the human body, each procedure has contraindications. In the case of CT, they are as follows:
- individual iodine intolerance;
- pregnancy and breastfeeding;
- severe kidney disease;
- patient weight more than 200 kg;
- diabetes mellitus type 2;
- increased level of creatinine in the blood;
- serious health condition.
MRI is prohibited in the following cases:
- the person’s body weight exceeds the permissible load on the table;
- the body has electronic implants, such as a pacemaker;
- allergy to iodine;
- serious condition.
There is no significant difference in cost between the procedures. In any case, the price of the study depends on the clinic where it is carried out and the characteristics of the equipment.
Preparing for the study
If a CT scan without contrast is planned, no special preparation is required on the part of the patient. If you need contrast, you need:
- Limit food intake four hours before the examination.
- Take a biochemical blood test to exclude possible contraindications.
The patient should know before the diagnostic procedure:
- Why is it being held?
- What sensations may accompany the administration of a contrast agent?
- How to behave in a tomograph (complete immobility and compliance with all the doctor’s requests).
- That you need to remove all metal jewelry.
Patients with fear of confined spaces may be prescribed sedatives. This will help relieve tension and conduct the examination with minimal stress.