| Complex. Ultrasound SCREENING (abdomen, kidneys, adrenal glands) | 2800 |
| Complex. ULTRASOUND SCREENING FOR MEN (abdomen, kidneys, adrenal glands, prostate gland, bladder with determination of residual urine, thyroid gland) | 5000 |
| Complex. ULTRASOUND SCREENING FOR WOMEN (abdomen, kidneys, adrenal glands, bladder, pelvic organs, mammary glands, thyroid gland) | 5000 |
| Obstetrics and gynecology | |
| Ultrasound of the pelvic organs (transabdominal) | 1500 |
| Ultrasound of the pelvic organs (transvaginal) | 1750 |
| Ultrasound of the mammary glands | 1500 |
| Ultrasound of the mammary glands with Doppler | 1850 |
| Ultrasound 1st trimester (up to 10 weeks) | 1800 |
| Ultrasound 2nd trimester (from 11 to 20 weeks) | 2000 |
| Ultrasound 3rd trimester (after 21 weeks) | 2200 |
| Fetal ultrasound 1st trimester to 12th week (SCREENING) | 2000 |
| Fetal ultrasound 2nd trimester after 12 weeks (SCREENING) | 2200 |
| Ultrasound determination of fetal sex | 1200 |
| Ultrasound of the fetus up to 21 weeks (multiple pregnancy) | 2200 |
| Ultrasound of the fetus from 21 weeks (multiple pregnancy) | 3500 |
| 3D-4D fetal examination | 3500 |
| 3D-4D fetal examination (multiple pregnancy) | 5000 |
| Vascular Doppler | 1200 |
| Ultrasound monitoring of a growing follicle (folliculometry) | 900 |
| Ultrasound of fallopian tube patency (Echohysterosalpingography (EchoHSG) | 7000 |
| Abdomen | |
| Ultrasound of the abdominal organs (without kidneys) with Doppler if necessary | 2000 |
| Ultrasound of the gallbladder | 1500 |
| Ultrasound of the gallbladder with determination of function | 1700 |
| Ultrasound of the spleen | 1200 |
| Ultrasound of the liver | 1200 |
| Ultrasound of the pancreas | 1000 |
| Cardiology | |
| Echocardiography (ECHO-CG / ultrasound of the heart) | 3000 |
| Vessels | |
| Ultrasound Dopplerography of the BCA (ultrasound Dopplerography of the brachiocephalic arteries) | 2500 |
| Ultrasound of the arteries of the upper extremities | 2200 |
| Ultrasound of the arteries of the lower extremities | 2700 |
| Ultrasound of the veins of the lower extremities | 2500 |
| Ultrasound of arteries and veins of the lower extremities | 4000 |
| SMALL ORGANS | |
| Ultrasound of the thyroid gland | 1500 |
| Ultrasound of the salivary glands | 1200 |
| Ultrasound of lymph nodes | 1200 |
| Ultrasound of soft tissues | 1500 |
| UROLOGY | |
| Ultrasound of the kidneys and adrenals | 1500 |
| Ultrasound of the bladder | 1100 |
| Ultrasound of the prostate and bladder with determination of residual urine (transabnominal) | 1800 |
| Ultrasound of the prostate gland (transrectal) | 1800 |
| Ultrasound of the adrenal glands | 1100 |
| Ultrasound of the penis | 1100 |
| Ultrasound of the scrotum | 1800 |
| ORTHOPEDICS | |
| Ultrasound of the joint | 1500 |
| Ultrasound of the cervical spine | 2000 |
| Ultrasound of the lumbar spine | 2000 |
Typically, the spleen is checked when an abdominal ultrasound is performed. The examination is mandatory for people with chronic cirrhosis or hepatitis and diseases of the lymphatic system.
Doctors recommend checking the spleen separately if there is a suspicion of leukemia, neoplasms (tumors and cysts), an increase in size and other abnormalities in the development and position of the organ. The spleen is checked for infectious diseases such as tuberculosis, syphilis, typhoid fever, mononucleosis, sepsis and abdominal injuries.
In what cases does a doctor prescribe an ultrasound of the spleen?
Ultrasound examination has no contraindications and restrictions on the number of sessions performed.
Using ultrasound, you can monitor the dynamics of treatment as often as you like. Normally, the spleen is located in the left hypochondrium, its outline does not extend beyond the edge of the rib line. With the disease, the spleen increases in size and protrudes from under the chest, which is noticeable upon palpation. To clarify the cause of the changes, the doctor prescribes an ultrasound.
The study is carried out by:
- if a spleen injury is suspected;
- inflammation;
- developmental anomalies - wandering spleen, development of the accessory lobe;
- malignant or benign neoplasms;
- disorders of hematopoietic function;
- infectious diseases - syphilis, sepsis;
- chronic diseases of the gastrointestinal tract;
- portal hypertension;
- preventive examinations after surgery.
The method allows you to quickly detect abscesses, traumatic necrosis, hemorrhages or tissue ruptures, and cysts.
The disadvantage of spleen ultrasound is considered to be the insufficient accuracy of the method for a single examination of the organ. But with a comprehensive ultrasound of the abdominal organs, the information is as accurate as possible.
Indications for spleen examination
The main indication for ultrasound of the spleen is pain, which many diseases make themselves felt. If after an initial examination by a doctor the situation does not clear up and the tests do not produce results, in most cases an ultrasound of the spleen is prescribed.
An ultrasound of the spleen is prescribed for suspected enlargement of the organ to confirm or refute this, as well as to find out the cause if the answer is positive. In addition, absolute indications for ultrasound of the spleen are diseases such as liver cirrhosis, leukemia, and infectious diseases. Ultrasound of the spleen may be prescribed to determine the location of metastases of a malignant tumor and in case of traumatic injuries to the abdominal cavity.
What does an ultrasound of the spleen show?
Ultrasound examination of the spleen can reveal:
- liver pathology;
- tumor process;
- development of infection: toxoplasmosis, scarlet fever, malaria, mononucleosis, endocarditis;
- damage due to trauma;
- inflammatory process;
- autoimmune diseases;
- dysfunction of hematopoiesis;
- hereditary diseases caused by gene deformation;
- disruption of the structure as a result of a heart attack, hematoma, abscess, cyst.
In children, an enlarged spleen may indicate a violation of hemoglobin synthesis due to anemia and sideropenia, leukemia, congenital pathology of the heart muscle, tuberculosis, and typhoid fever.
How to prepare for research
In emergency cases, the doctor will perform an ultrasound examination without prior preparation of the patient. This is how victims of accidents, beatings, or severe bruises are examined. If you quickly identify rupture of organs in the abdominal cavity, internal bleeding, precious time for providing assistance will not be missed.
For planned events, patient preparation begins three days before the study.
Recommended:
- Eliminate cabbage, baked goods and sweets, milk, legumes, coffee, carbonated drinks and other foods that contribute to gas formation from your diet. Gas-filled intestinal loops make it difficult to assess the shape and position of the spleen.
- Do not eat anything for 9 hours before the test.
- Take sorbents, carminatives and enzyme preparations for digestion 12 hours before the test.
- For patients who suffer from constipation, take a mild herbal laxative or do a cleansing enema.
If gas formation is increased the day before the examination, you should take activated carbon at the rate of one tablet per kilogram of the patient’s weight.
During the day before the procedure, you should not smoke or drink alcohol. Otherwise, the stomach spasm will affect the condition of the spleen and the examination result will lose its informative value. You should not chew chewing gum.
If an ultrasound of the spleen is necessary for a child, you can limit yourself to 3-6 hours of fasting. The older the child, the longer the food break should be. You can only drink clean, non-carbonated water, but it is prohibited to drink water an hour before the test.
The child should be prepared psychologically for the study, persuaded, and offered the upcoming study as the basis for a new game. It is necessary that the baby can relax and lie quietly on the couch so that the doctor has enough time to examine.
Echography of the spleen in children and adolescents

Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Clinical and echographic semiotics
The spleen is rarely affected primarily, but almost always changes in hematological, oncological, immune, vascular, infectious, and systemic diseases. However, detecting these changes is not easy. The situation with the detection of spleen pathology and the possibility of dynamic monitoring has radically changed with ultrasound examinations.
The spleen is a unique organ even in its genesis. All unpaired organs of our body are formed along the midline. The spleen is an exception. It appears in the 4th week of intrauterine development from a mesenchymal protrusion on the left side of the dorsal mesogastrium from cells of both superficial and deep mesenchyme. At the 20th week of gestation, foci of hematopoiesis appear in the spleen. The spleen is a lymphatic organ included in the circulatory system. This is the only lymphatic organ where there are close connections between lymphatic tissue, blood vessels and cells of the reticuloendothelial system [1]. Blood circulation in the spleen is no less unique; there are two types of blood flow through the spleen - open and closed. In a closed type of circulation, the central artery supplies blood to the white pulp, the blood passes directly through the marginal zone of the sinuses and drains into the venous sinuses. With an open type of circulation, the central artery supplies the red pulp with blood and breaks up into capillaries that drain into the parenchyma. Only from there does the blood enter the venous sinuses, which collect in the trabecular veins and flow into the common vein of the spleen in the hilum area. 10% of the incoming blood passes through the closed circuit, 90% through the open circuit. The mixed type of circulation determines the phase nature of the image of the spleen in computed tomography or magnetic resonance vascular tomography. Initially, in the early arterial phase, the spleen appears inhomogeneous, later, in the late arterial or venous stage, it appears homogeneous.
Functionally and anatomically, the spleen is fully formed only by adolescence. Thus, the white pulp in children makes up 30% of the mass of the spleen, in adults - 15-20%, after 50 years - even less. In adults, the spleen weighs about 150 g, in old people - 100 g. About 300 liters of blood passes through the spleen per day. The red pulp (trabecular mass) performs the function of depositing blood, the white pulp is a lymphatic organ.
The development of a child into an adult and then the involution of a strong adult into an old man is characterized by physiological discordance, that is, different organs at different age periods develop or involute at different rates. When recalculated by body weight, a 10-year-old child has 2 times (!) more lymphoid tissue than a 20-year-old strong young man [2]. The spleen is an extremely variable organ. 0.1% of people have no spleen (asplenia). In most of these individuals this anomaly does not manifest itself in any way. Apparently, in some cases there is not true asplenia, but heterotopia of the spleen. Echography sometimes gives false negative conclusions in asplenia, since the displaced left lobe of the liver can be mistaken for a non-existent spleen. The best method for detecting splenic atopy is technetium-99m scintigraphy. True asplenia can be combined with a central position of the liver, three-lobe lungs, and malposition of the small intestine.
Possible polysplenia. The presence of additional spleens can be combined with bilobar lungs, tracheoesophageal fistula, absence or hypoplasia of the gallbladder, duodenal atresia, small intestinal malposition, and anal atresia. Combinations of asplenia with Dandy-Walker syndrome, cleft palate and maxilla, myelomeningocele, absence of the left adrenal gland, and hypospadias are very rare. Almost one in four have accessory splenic tissue. Most often it is found in the area of the hilum of the spleen, tail of the pancreas, mesentery, lig. Colicolienalis, on the appendages and in the scrotum. An additional spleen extending toward the kidney simulates a kidney tumor.
Ectopic spleen can be either congenital (the presence of additional spleens or displacement of the anlage of the only spleen) or acquired. In the latter case, ectopia can occur when the diaphragm is ruptured and the spleen is displaced into the chest cavity or the spleen is displaced into the chest cavity due to Bochdalek's hernia. Even an infarction of the spleen has been described when it is strangulated in the hernial opening [3].
The spleen is quite well fixed by the lienogastric and lienorenal ligaments. In the absence of the lienorenal ligament, the phenomenon of the so-called mobile spleen appears. Volvulus of the spleen (sometimes self-resolving) cannot be ruled out. In children, splenic volvulus most often occurs before the age of 1 year; among adults, it is typical for women 20-40 years old. Provocateurs can be trauma, pregnancy, splenomegaly. Volvulus of the spleen leads to impaired blood outflow, an increase in the size of the spleen, hypersplenism and its infarction. During Doppler examination, blood flow in the area of the splenic hilum is not detected. Very rarely, splenic volvulus leads to torsion of the tail of the pancreas. Among other anomalies of the spleen, the splenogonasal association is known. The anomaly is only left-sided and occurs in the 5-6th week of intrauterine life. It is caused either by minimal inflammatory adhesions between the anlage of the gonad and the spleen, followed by translocation of part of the splenic tissue into the scrotum, or by close contact of the anlage cells of the spleen and gonad. In most cases, the spleen and testicle in the scrotum or the spleen and ovary are discrete and connected only by a delicate connective tissue flagellum (discrete type of splenogonasal association). In the continuous type of association, the gonad and spleen are connected by splenic tissue or a fibrous cord with additional spleens included in it. Usually the orthotopically located spleen is not changed. In rare cases, a splenogonasal continuous association is combined with anomalies of the limbs, jaws, additional lobes of the lungs and liver, and anal atresia. 50% of all diagnosed cases of splenogonasal association occur in boys under 10 years of age. Clinically, the anomaly manifests itself as a painless enlargement of the left testicle without signs of scrotal edema and is initially interpreted as a hernial protrusion. Echographically, an additional small (1-2 cm in diameter) formation is detected, located in close proximity to the testicle and differing from it in echotexture. Differential diagnostic difficulties arise when excluding polyorchid, extragonadal tumor, and epididymitis. Scintigraphy with technetium-99m accumulating in the spleen helps to suspect ectopic splenic tissue. However, a final diagnosis can only be made based on the results of the operation. It is important that echographic findings allow orchiectomy to be avoided. In girls, the anomaly is discovered by chance during ultrasound examinations.
The abundance of anatomical and topographical features and the conjugation of many functions in a relatively small volume explain changes in the spleen in response to a wide range of factors: infectious, immune, hemodynamic, etc. But all of them lead to changes in the size of the spleen and its density.
The term "splenomegaly" is widely used to refer to varying degrees of enlargement of the spleen. With splenomegaly of various etiologies, various structural changes occur in the spleen. Thus, in case of disturbances in the outflow of blood from the spleen (portal hypertension, compression of v. lienalis), the total length of the sinuses as a result of their new formation increases sharply, and the diameter turns out to be smaller than normal. The number of cells in the sinus walls decreases (per unit area of the sinus wall, or cm²), the total number of phagocytoactive cells increases sharply. With splenomegaly, in response to increased intrasplenic breakdown of erythrocytes, the pulp cords increase in size, expand with an increase in phagocytic cells and hyperplasia of sinus cells.
Splenomegaly is typical for: hyperdibasic aminoaciduria type I; amyloidosis; Budda - Chiari syndrome; Byler's disease; homozygous beta thalassemia; cholesterol and triglyceride accumulation diseases; trimethylaminuria; vinyl chloride disease; Wolman's disease; Felty's syndrome and Still's disease; G1M gangliosidosis type I; Gaucher, Niemann-Pick and Letterer-Zieve diseases; glycogen storage disease (especially type 4); iminodipeptiduria; progressive lipodystrophy; alpha-mannisidosis; mevalonacidemia; mucolipidosis types II and III; mucopolysaccharidosis types IH, II, VI and VII; neutropenia; POEMS complex; sialidosis; spherocytosis; Simpson-Golabi-Bemel syndrome; Tangier disease; Zimmerman - Labanda syndrome; Stauffer's symptom complex; infectious, rheumatic diseases, hemolytic conditions and portal hypertension.
Ultrasound examinations are the first, and often the final, when excluding spleen pathology.
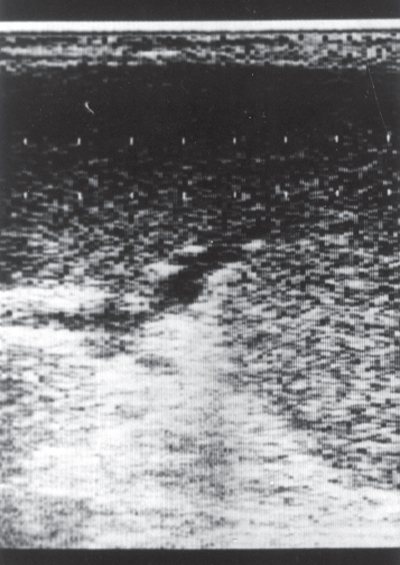
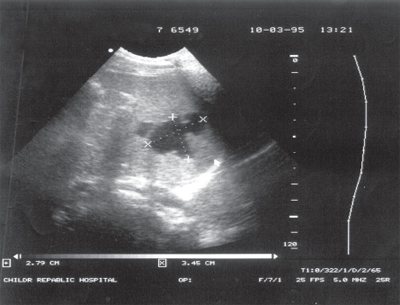
The splenic capsule is extremely thin and therefore cannot be visualized. But thanks to the capsule, the image of the edge of the spleen appears very clear, although it can be difficult, especially in obese patients, to delimit the lateral edge of the spleen from the abdominal wall. The thinnest connective tissue layers extend from the spleen capsule into the parenchyma, which mark division into lobules, although there is no completely lobular structure, so the organ is very fragile, especially with splenomegaly, when the ratio of parenchyma and connective tissue changes sharply in favor of the first component. Normally, the echographic image of the spleen is homogeneous. The echogenicity of the spleen in newborns, infants and young children is lower than in adults, which is explained by the weak development of trabecular tissue and completely repeats the age-related dynamics of the echostructure of the lymph nodes. The echogenicity of the splenic hilum is higher than that of its parenchyma. In the spleen itself, when using sensors with a radiation frequency of 3-5 MHz, a large number of small linear or point signals are recorded. The use of high frequency sensors (13 MHz) made it possible to prove that these signals are a reflection of ultrasound from lymphoid follicles (white pulp). The correlation coefficient with histological findings turns out to be very high (r=0.71; p=0.03) [4]. Constructing images in various modes opens up new perspectives in assessing the structure of the spleen. Ultrasound imaging of the spleen in MRI mode makes it possible to better visualize the parenchyma and remove extraneous signals (Fig. 1).
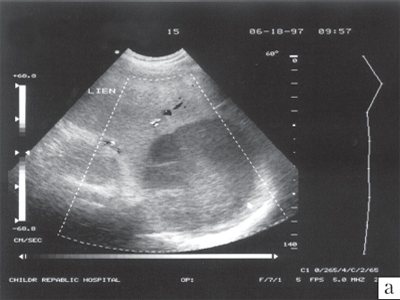
Rice. 1.
Image of the spleen in normal mode and MRI mode.

A)
Image of the spleen during ultrasound scanning in normal mode. Many additional echo signals are detected in the parenchyma.
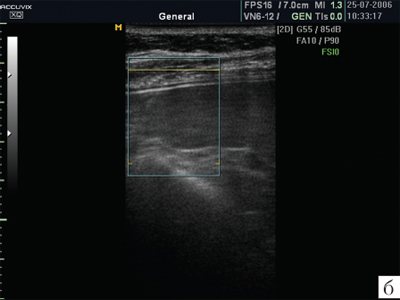
b)
Ultrasound image of the spleen in MRI mode. This type of imaging allows for better visualization of the parenchyma.
Often, in the area of the hilum of the spleen, a round formation with a diameter of 1-2 cm is found, completely repeating the structure of the image of the spleen. This formation is interpreted as an accessory spleen. An accessory spleen, according to morphological studies, is found in approximately 20-25% of cases. Since some additional lobules of the spleen are located far from it, in the abdominal cavity and even in the scrotum, they are not always detected sonographically. After the spleen is removed, the accessory spleen hypertrophies and takes the form of a normal spleen. It is the presence of an accessory spleen that leads to the fact that refunctioning of the spleen after embolization is observed in 5-10% of cases. This percentage is significantly higher in hemolytic anemias. According to our data, after the first embolization, refunctioning of the spleen develops in 40-50% of children and adolescents, which requires repeated interventions.
The clarity of the contours of the spleen allows one to reliably determine its size. In practical work, the size of the spleen is estimated by its length. A. Doria et al. [5] presented in their work the standards adopted abroad. For precise control of the size of the spleen, detection of hidden splenomegaly and scientific research, determination of the volume of the spleen by its size in three planes is used. Variations in these sizes when performed by different specialists are minimal, and the correlation with computed tomography data is excellent [6, 7].
Changes in the echographic picture of the spleen, along with changes in its size and topic, can be represented as a homogeneous or focal change in its structure.
Private problems
Diffuse changes in the spleen
. A homogeneous change in the structure of the spleen (increased echogenicity) is characteristic primarily of portal hypertension. This is the most common change in the spleen known in the clinic of internal medicine. The echogenicity of the parenchyma with portal hypertension increases moderately. With pathology of erythropoiesis, hyperplasia of the reticuloendothelial system or heart failure with blood stagnation in the periphery, the echogenicity of the spleen does not change, although its size increases. The pathology of granulopoiesis, lymphopoiesis and multiple myeloma are accompanied by a decrease in the echogenicity of the parenchyma of the enlarged spleen. The spleen reaches extremely large sizes, descending into the small pelvis, in chronic myeloid leukemia. However, its echogenicity, as a rule, does not change, the parenchyma remains homogeneous. Systemic inflammatory diseases leading to splenomegaly in the first stages occur with a decrease in the echogenicity of the spleen, which reflects inflammatory edema of the organ, but this stage is quickly replaced by an increase in the echogenicity of the spleen.
Rice. 2.
Echogram of the spleen of a child with amyloidosis. The spleen is sharply enlarged in size, dense, the vessels in the hilum area are dilated.
Many storage diseases occur with changes in the echogenicity of the spleen. A diffuse increase in the echogenicity of the spleen is typical of glycogenosis, Wilson-Konovalov disease, iron overload diseases, and amyloidosis. In amyloidosis, the spleen capsule thickens. Initial condensation of echo signals is observed in the hilum region, close to the vessels, which is consistent with the known tendency of amyloid to accumulate in the walls of blood vessels and the paravasal space. Then a mass of additional echo signals of varying densities and sizes appears in the parenchyma. Subsequently, they completely replace the parenchyma of the organ and the echographic picture resembles the “greasy” or “clay” spleen described by pathologists (Fig. 2).
In Gaucher disease, when focal deposition of glucocerebrosides is possible, hyper-, hypoechoic or mixed foci are found against the background of increased general echogenicity of the spleen.
Local (focal) changes in the spleen
. Small hyperechoic foci are characteristic of splenic calcifications. In pediatric practice, they are usually the result of an intrauterine infection, are discovered accidentally and do not affect the prognosis and quality of life. Large calcifications form after injuries.
Focal changes in the spleen are observed with tumors. Hyperechoic round formations are typical of non-Hodgkin's lymphomas. Lymphomas are one of the few types of tumors that metastasize to the spleen. Hypoechoic formations (“target-shaped spleen”, “shot spleen”) are typical for Hodgkin lymphoma (Fig. 3).
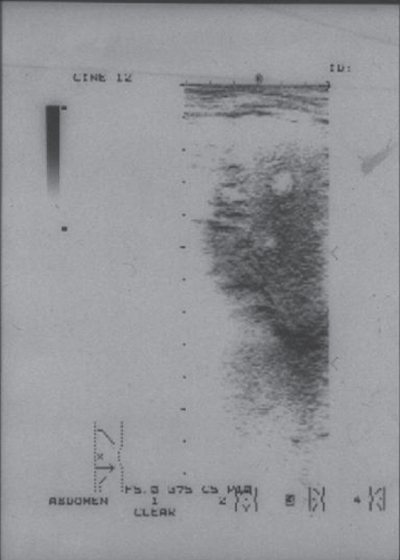
Rice. 3.
Echogram of the spleen in Hodgkin's lymphoma. Echo-negative formations are visualized in the parenchyma.
There are three possible degrees of spleen damage in lymphomas, reflecting three degrees of risk [8]:
- the lesions are located separately, do not merge, the edges of the organ are not changed;
- the foci merge with each other;
- the foci merge with each other and deform the edge of the organ.
Hypoechoic foci, forming the same picture of a “target-shaped spleen,” are observed in a variant of immunodeficiency such as incomplete phagocytosis, and are essentially small abscesses. In contrast to tumor foci, foci in immunodeficiencies are numerous and less homogeneous (Fig. 4).
Melanoma metastases can be either hyper- or hypoechoic [9].
Greater differential diagnostic difficulties arise in the presence of inflammatory pseudotumor of the spleen. Inflammatory pseudotumor can be discovered accidentally, looks like a clearly defined mass, sometimes with calcifications, resembles a hamartoma, lymphoma [10]. Histologically, myofibroblasts and inflammatory cells are detected in it. According to immunohistochemistry and in situ hybridization, the Ebstein-Barr virus is detected [11, 12]. Despite the high sensitivity of imaging methods, the results are nonspecific and the final diagnosis is made on the basis of histological studies [13].
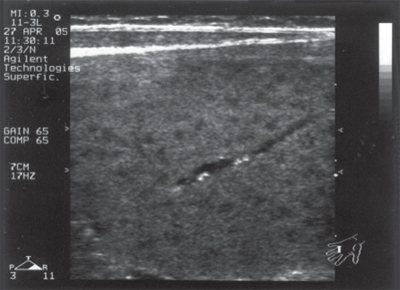
Rice. 4.
Multiple echo-negative formations in the spleen in a child with primary immunodeficiency syndrome. Small, high-intensity echo signals (calcified thrombi) are detected in the lumen of the vessel.
Benign tumors of the spleen include hamartomas, lymphangiomas and hemangiomas. All these tumors begin at birth, but usually manifest themselves in the 4th to 6th decade of life. Hemangiomas are the most common primary tumors of the spleen. Small hemangiomas do not manifest themselves in any way. Large hemangiomas appear as a space-occupying formation in the left hypochondrium, painful when thrombosed. Thrombosis of a giant hemangioma is manifested by anemia, thrombocytopenia and consumption coagulopathy (Kasabach-Merritt syndrome). Echographically, hemangioma looks like a polycystic formation, in which calcifications are possible. Large hemangiomas of the spleen are usually combined with hemangiomas of other organs, which facilitates the interpretation of the echographic picture.
Small multiple calcifications in the spleen are usually discovered by chance and may indicate a past infection, in small children - intrauterine.
Splenic abscesses often occur with sepsis. In most cases, abscesses are small, multiple, clinically “silent”, and are detected at autopsy. Clinically significant splenic abscesses are usually solitary and result from:
- systemic bacteremia;
- blind or penetrating trauma with superinfection of hematoma, infarction (with hemoglobinopathies, malaria, hydatid cysts);
- introduction of infection from another source, for example from a subdiaphragmatic abscess.
Rice. 5.
Sonographic and angiographic image of a primary splenic cyst.
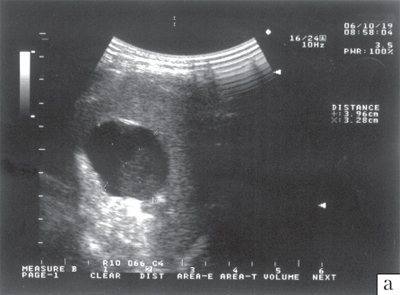
A)
Sonographic picture of a primary splenic cyst. The contents of the cyst are homogeneous, the contours are clear and smooth.
b)
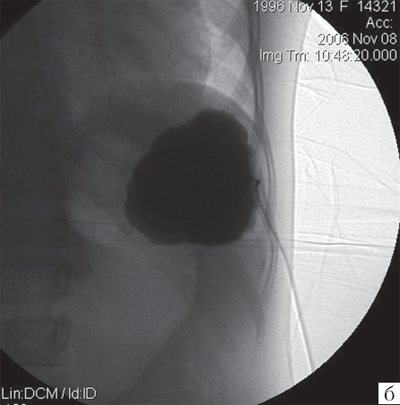
Angiographic image of a primary splenic cyst. The contours of the cyst are smooth. The filling of the cyst with contrast agent is uniform.
The most common pathogens are staphylo- and streptococci, anaerobes, aerobic gram-negative bacilli, including salmonella. Fungi can cause splenic abscesses in immunocompromised patients. Spleen abscesses in immunocompromised patients are usually accompanied by abscesses in other organs. This pathology of the spleen most often debuts subacutely with fever, pain in the left hypochondrium, often pleuritic, in the side, upper abdomen, radiating to the left arm. The muscles of the left upper quadrant of the abdomen are tense. Splenomegaly is typical. Rarely, a friction rub is heard over the spleen. Leukocytosis is characteristic. Sometimes it is possible to obtain a culture from blood. On plain radiography, the left dome of the diaphragm is elevated, and effusion is detected in the left pleural cavity. The kidney, colon, and stomach are displaced. With gas-forming flora, extraintestinal gas is detected in the abscess. An echographic examination reveals splenic abscesses with a diameter of more than 1 cm, but reliably - 2-3 cm or more. The most informative are CT and MRI.

Rice. 6.
Three-dimensional reconstruction of the surface of a primary splenic cyst. It is clearly visible that the surface of the cyst is smooth. The technique allows you to determine the volume of the cyst, its surface area, and the topic of formation.
Congenital splenic cysts (true) are rare. They look like echo-negative formations with homogeneous content and clear contours (Fig. 5). Modern ultrasound diagnostic devices allow you to construct a three-dimensional image of an object. When constructing a three-dimensional image, the surface of the congenital cyst is smooth (Fig. 6). Infection of a primary cyst is rare. A cyst, even a relatively small one, can manifest itself as hypersplenism. Hypersplenism necessarily accompanies giant cysts (Fig. 7). Accidental injuries with cyst rupture and bleeding pose a great danger. We (Yu.A. Polyaev) strive to preserve the organ as much as possible and introduce a sclerosing agent, which allows us to avoid removal of the spleen. In recent years, in no case has the spleen been removed due to the presence of primary cysts. Long-term results of organ-preserving operations are good.
Secondary cysts (echinococcal, post-traumatic = hemorrhagic, epidermoid) have heterogeneous contents and rough walls. The post-traumatic cyst is usually irregular in shape (Fig. 8). With echinococcosis of the spleen, along with the main large cyst, visualization of several daughter cysts is possible.
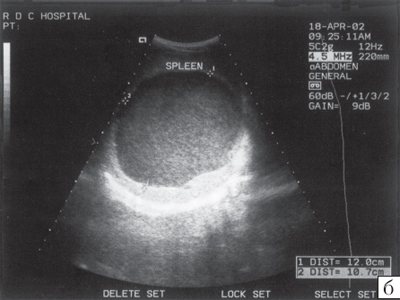
Rice. 7.
Image of a giant splenic cyst..
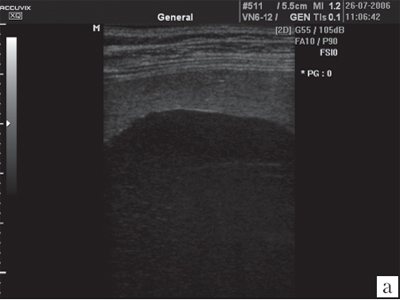
A)
Ultrasound MRI image of a giant primary splenic cyst. It is clearly visible that the parenchyma layer is small.
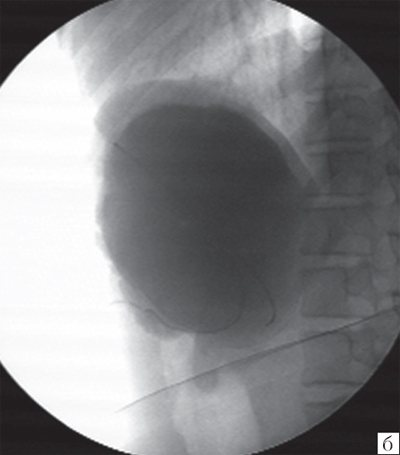
b)
Contrast angiogram of the same cyst.
Spleen hematomas resemble a cyst. Splenic hematomas are the result of blunt trauma to the abdomen. Splenic hematoma and rupture of this organ in older children are the result of blunt trauma to the abdomen. In 10-20% of cases, hematoma and even rupture of the spleen are not very obvious clinically. Diagnosis is complicated by multiple injuries and head injuries, therefore, each injured child taken to a specialized hospital must undergo a complete echographic examination.
Rice. 8.
Sonographic image of a post-traumatic splenic cyst. The shape of the cyst is irregular; septa are visible inside.
A survey X-ray of the abdominal cavity in the presence of a splenic hematoma and even more serious injuries may not reveal anything. Other signs of splenic injury may include splenomegaly, rib fractures, pneumothorax, high left dome of the diaphragm, fluid in the pleural cavity, free fluid (blood) in the abdominal cavity. Injury to the spleen is often combined with injury to the lower lungs and kidney injury. Ultrasound scanning can reliably and quickly detect splenic injury. In contrast to a true cyst, echo-positive inclusions of low and medium density (thrombi) quickly appear inside the hematoma. A so-called “chocolate cyst” is formed (Fig. 9). Echography, as opposed to scintigraphy and angiography, is the method of choice in diagnosing cysts. Scintigraphy and angiography do not allow distinguishing a cyst from an avascular tumor. A subcapsular hematoma looks like an echo-negative formation spreading along the contour of the spleen. The adjacent part of the parenchyma is compacted due to compression. Over time, as the hematoma organizes, linear adhesions appear inside it. Splenic rupture appears as the appearance of linear, broken hypoechoic stripes of uneven width within the spleen.
Rice. 9.
Splenic hematoma...
A)
Relatively recently appeared splenic hematoma. Its contents are heterogeneous.
b)
As the spilled blood coagulates and blood clots form, the density of the hematoma increases.
In newborns, splenic rupture is possible immediately after birth or on the 4-5th day of life. A splenic rupture can be suspected by the appearance of sudden pallor, wheezing breathing, or respiratory collapse. The reason is a combination of age-related vitamin K deficiency with hypocoagulation and minimal trauma when serving a child. In any case, if a splenic rupture is detected, the doctor should suspect child abuse.
Splenic infarction is the result of occlusion of the splenic artery or one of the terminal intrasplenic arteries. Splenic infarction is a typical pathology of the vessels of this organ and is considered in the section on local changes in the spleen only because of its external manifestations - segmental disturbances in echogenicity.
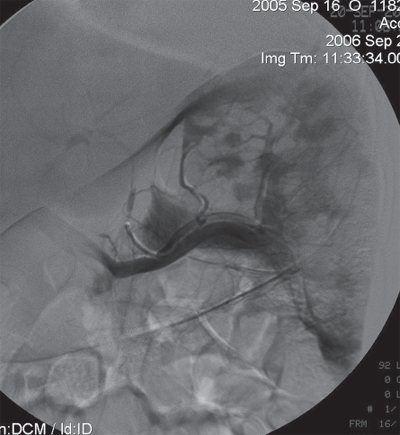
Rice. 10.
Angiogram of the spleen after its repeated occlusion in a patient with hemolytic anemia. Dark lesions indicate accumulation of contrast agent in the remaining parenchyma. In places of previous artificial infarctions, the contrast agent does not accumulate.
Splenic infarction is typical for torsion of this organ, sickle cell anemia, lymphomas, leukemia, myelofibrosis, Gaucher disease, embolism of various origins (including extrasystole), aneurysm of the splenic artery, vasculitis, antiphospholipoid syndrome, hypercoagulation, splenomegaly with circulatory disorders [14]. Small infarcts appear as hypoechoic formations in which blood flow is not detectable. If the infarction reaches the capsule, the contour of the organ is deformed. Small heart attacks are replaced by a connective tissue strip. Massive repeated infarctions lead to autosplenectomy, organ obliteration and reduction in size (Fig. 10).
Pathology of the vessels of the spleen
Splenic artery aneurysm is the most common type of visceral artery aneurysm. Detected depending on age in 0.07-10% of all autopsies. 85% of all cases of splenic artery aneurysms occur in women. The causes and/or predisposing factors for the appearance of splenic artery aneurysms are portal hypertension, pregnancy, multiple pregnancies, pancreatitis (erosion of the artery wall with the formation of a pseudoaneurysm or extension of the pseudocyst wall into the artery), penetrating gastric ulcer, fungal aneurysm, Ehlers-Danlos syndrome, periarteritis nodosa.
An aneurysm may be asymptomatic or clinically manifest by the presence of a pulsating formation or rupture (6-10% of all aneurysms). 95% of all ruptures occur during pregnancy. A ruptured aneurysm may extend into the intestine (intestinal hemorrhage), the abdominal cavity (hemoperitoneum), the pancreatic duct (hemosaccus pancreaticus), or the splenic vein.
Ultrasound examination reveals an anechoic formation with or without peripheral calcification, blood clots, a “cyst within a cyst” (pseudoaneurysm within a pancreatic pseudocyst), weak, unstable turbulent or pulsatile blood flow [15].
Aneurysm of the splenic vein can be congenital (idiopathic) with portal hypertension, pancreatitis, Osler-Rendu-Weber syndrome, after trauma or splenectomy. Splenic vein aneurysm is usually asymptomatic, but can be complicated by rupture, thrombosis, or embolism.
Ultrasound examination reveals a sac-like dilatation of the vein with slow blood flow.
An arteriovenous fistula develops with vascular malformations, iatrogenically after surgical interventions, after removal of the spleen, rupture of an arterial aneurysm, and with pancreatitis [16]. A predisposing factor is pregnancy, especially multiple pregnancy. An arteriovenous fistula immediately leads to portal hypertension with its characteristic clinical picture. Ultrasound examination reveals rapid massive blood flow through the splenic vein and artery.
Thus, modern visual diagnostic methods make it possible to reliably determine the size of the spleen and reliably characterize its structure.
Literature
- Ginsburg T. Hematology of Infancy and Childhood. 6th ed. Philadelphia: Harcourt Health Sciences. 2003. P. 280-365.
- Harris J. (Ed.) The measurement of man. Philadelphia. 1930. 534 p.
- Bakier B., Poyanhi A., Yekeler E. et al. Acute torsion of a wandering spleen: imaging findings // Diagnostic ultrasound. 2004. V. 29. R. 707-709.
- Rosenberg H., Markowitz R., Kolbeg H. et al. Normal splenic size in infants and children: sonographic measurements // American Journal of Radiology. 1991. V. 157. R. 119-121.
- Doria A., Daneman A., Moineddin R. et al. Highfrequency sonographic patterns of the spleen in children // Radiology. 2006. V. 240. R. 821-897.
- Lamb P., Lund A., Kangasabay R. et al. Spleen size: how well do linear ultrasound measurements correlate with three dimensional CT-volume assessment? // British Journal of Radiology. 2002. V. 75. R. 533-577.
- Picardi M., Martinelli V., Ciancia R. et al. Measurement of spleen volume by ultrasound scanning in patients with thrombocytosis: a prospective study // Blood. 2002. V. 99. R. 4228-4230.
- Nazarenko O.R. Comparative value of echography in assessing the condition of the abdominal organs in children with acute lymphoblastic leukemia / Abstract. dis.* cand. honey. Sci. M., 1997. 26 p.
- Bolondi L., Gandolfi L., Labo G. Diagnostic ultrasound in gastroenterology. Batterworths, Bologna. 2000. 540 rub.
- Franquet T., Montes M., Aizcorbi M. et al. Inflammatory pseudotumor of the spleen: ultrasound and computed tomographic findings // Abdominal Imaging. 2005. V. 14. R. 181-183.
- Puyan F., Bilgi S., Yalcin O. et al. Inflammatory pseudotumor of the spleen with EBV-positivity: report of the case // European Journal of Hematology. 2004. V. 72. R. 285-291.
- Akatsu T., Kamayama K., Tanabe M. et al. Ebstein-Barr virus-positive inflammatory pseudotumor of the spleen with the concomitant rectal cancer: a case report and review of literature // Digestive diseases and science. 2007. V. 52. P. 2806-2812.
- Shapiro A., Adams E. Inflammatory pseudotumor of the spleen managed laparoscopy. Can preoperative imaging establish the diagnosis? Case report and literature review // Surgical laparoscopy, endoscopy and percutaneous techniques. 2006. V. 16. P. 357-361.
- Guth A. Splenic infarct // eMedicine, last updated February 2006.
- Schepper A., Vanhoenacker F., Beck B. et al. Vascular pathology of spleen. Part I // Abdominal imaging. 2004. V. 30. P. 96-104.
- Schepper A., Vanhoenacker F., Beck B. et al. Vascular pathology of spleen. Part II // Abdominal imaging. 2005. V. 31. P. 228-238.
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Sequence of the procedure
The procedure is painless and takes no more than 20 minutes. Then the doctor deciphers and hands over the examination results.
The examination takes place in the following order:
- The patient enters the office and lies on his back on the couch.
- Frees the left hypochondrium area from clothing.
- The doctor applies a special gel to the patient’s skin that conducts ultrasound signals and promotes better gliding. The composition is safe and does not cause allergies.
- By moving the sensor of the device along the hypochondrium, the doctor records the parameters of the spleen, changes in its structure, and takes measurements. He pays attention to the condition of the blood vessels and lymph nodes of the spleen. An image of the organ is displayed on the monitor, the doctor records the required angles and prints out the images.
If the patient has congenital anomalies of the spleen, the doctor will ask him to lie on his right side and place his left hand behind his head. An ultrasound will be performed through the intercostal space.
To get a better look at the organ being examined, the doctor may ask the patient to take a deep breath and hold it for a few seconds.
Norm of indicators when decoding data

The results of the study are deciphered by the ultrasound doctor. It describes the state of the structure of the spleen tissue, the presence of congestion, injuries, tumors, the size of the splenic artery and vein. The patient submits the study protocol to the attending physician.
Normally the readings are:
- echogenicity: medium;
- diameter of the middle splenic vein: no more than 0.5 cm;
- sickle-shaped organ;
- a vascular network is acceptable in the portal area
- location: in the left hypochondrium between the diaphragm and the stomach;
- size: from 12 cm within the oblique cut (length), to 8 cm of the transverse cut (width), 4 cm thickness.
- estimated weight: 140–250 g.
- the structure is homogeneous, fine-grained, the contour is continuous.
Sizes of the spleen in children:
- under 3 years of age: 68 by 50 mm;
- from 3 to 7 years: 80 by 60 mm;
- from 8 to 12 years: 90 by 60 mm;
- from 12 to 15 years: 100 by 60 mm;
- over 16 years old: the size of an adult’s organ.
On average, women have a smaller spleen than men.
What does the doctor check?
An ultrasound examination involves assessing an organ according to standard parameters - position, shape, structure, size, tissue quality, blood vessels. Normally, the spleen of an adult should meet the following parameters:
- have a “crescent” shape, where the outer side is convex and the inner side is concave;
- the spleen is located on the left, between the stomach and the diaphragm, in close proximity to the left kidney and adrenal gland, pancreas, and colon;
- The standard dimensions of the organ are: 11–12 cm in length, 6–8 cm in width and 4–5 cm in thickness;
- standard vessel sizes are: the diameter of the splenic vein is 5 mm, the artery is 1–2 mm.
The size of the spleen in children depends on age and height.
Our clinic constantly hosts promotions