Caries and pulpitis are two common dental diseases that have similar symptoms. Moreover, the second disease can act as a complication of the first. However, the treatment methods for these pathologies are slightly different. In this article we will tell you how to distinguish caries from pulpitis. Can I do this myself?
In this article
- How to distinguish deep caries from pulpitis
- Diagnosis of caries and pulpitis
- How to treat deep caries and pulpitis
- Prevention of caries and pulpitis
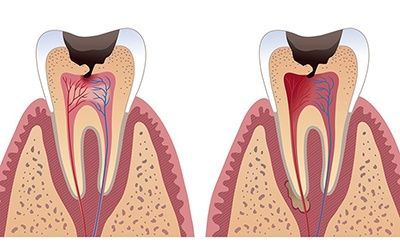
To understand the differences between caries and pulpitis, you should consider the features of both pathologies. Carious lesion is a slowly developing process of destruction of hard tooth tissues, resulting from the proliferation of cariogenic microbes. Bacteria produce acids that corrode enamel and dentin. This process develops slowly, but is constantly progressing.
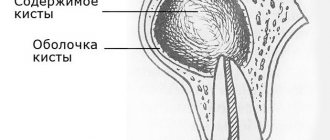
Pulpitis is an inflammatory disease of the pulp - the soft tissue located inside the tooth. As a rule, it occurs due to infection of the pulp by bacteria, which spread as caries progresses. If a carious lesion is left untreated, it penetrates into the dentin and affects the soft tissue.
Pulpitis can develop for other reasons, for example, after mechanical trauma and chipping of part of the tooth. But in most cases it is diagnosed in people with advanced caries. The etiology and mechanism of development of these pathologies have similar features. They also have common symptoms, so pulpitis and caries are often confused. Let us describe the signs of both pathologies.
How to distinguish deep caries from pulpitis
The main symptom of pulpitis is sharp pain in the tooth. With caries, they do not occur immediately, but only at the third or fourth stage of the disease. First, the carious lesion affects the enamel. At this stage, the pathology is asymptomatic. Only with the development of the second degree does discomfort appear when eating sweet foods.
Pulpitis and caries have a common symptom - pain. However, the nature of the pain is different. Let's describe the main differences:
- With pulpitis, pain occurs randomly. Its appearance can be triggered by any external factor, for example, cold wind.
- With caries there is no spontaneous pain. They appear when the tooth is exposed to sweet or sour foods, hot and cold temperatures, or when brushing the teeth. Usually the pain goes away immediately after the irritant is removed.
- Pain with pulpitis is prolonged. The tooth aches for a long time. Moreover, even strong analgesics do not help. Often the pain radiates to the temple or ear area.
You can distinguish deep caries from pulpitis by external signs. A darkened tooth indicates nerve death. Also in favor of pulp inflammation is the scale of destruction. If a tooth is destroyed by ⅓, most likely the pulp is also affected.
Diagnosis of pulpitis
Correct diagnosis of pulpitis is a primary task for any dentist, since this disease can be confused with caries, trigeminal neuralgia and exacerbation of chronic periodontitis. Each of these diseases is characterized by pain symptoms, so in order for the diagnosis to be correct, it is necessary:
- identify the causes of pain;
- determine the frequency of pain;
- determine the intensity of attacks;
- conduct a visual inspection;
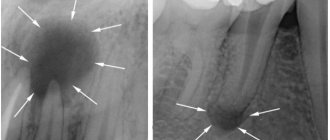
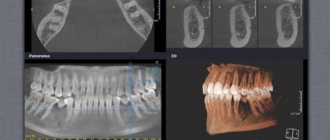
- carry out x-ray diagnostics.
Diagnosis of caries and pulpitis
Actually, there is no need to diagnose at home and try to find the differences between these diseases on your own. If you have a toothache, you need to go to the dentist, regardless of whether the cause is caries or pulpitis. The doctor will make a diagnosis based on an external examination of the tooth. He can also prescribe laboratory and instrumental diagnostic methods.

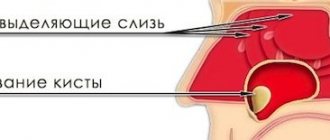
If a carious process is suspected, a special dye test is used. A pigment composition is applied to the enamel, which colors the carious lesion blue. If caries is not confirmed, the doctor will check the pulp for sensitivity. If necessary, radiography is prescribed. X-rays can reveal hidden carious cavities in the interdental spaces or under the gum.
Why does inflammation develop?
The main reason for the development of inflammatory processes in the pulp is infection due to advanced caries. Usually (in 90% of cases) the infection enters the pulp through a carious cavity. But sometimes a retrograde route is possible (the penetration of bacteria through a hole in the root or periodontal pockets). It is extremely rare (with osteomyelitis, acute respiratory infections, rubella, chickenpox, sinusitis) the infection is introduced through the blood - the hematogenous route.
Other factors can cause pulpitis:
- poor-quality treatment of a carious cavity or accidental damage to the pulp chamber during the treatment of caries;
- improper filling of the canal;
- pulp burn when grinding a dental crown before prosthetics;
- gum diseases leading to the formation of periodontal pockets;
- tooth injury.
Depending on the etiology, there are 4 types of pulpitis:
- infectious
– develops due to the penetration of pathogenic bacteria into the pulp;
- traumatic
– the cause is a violation of the sterility of the pulp due to traumatic damage to the tooth, due to which opportunistic bacteria are directed into the pulp chamber and provoke inflammation;
- iatrogenic, or medical
– occurs due to the fault of the dentist due to improper treatment of the carious cavity;
- calculiform
– the result of a metabolic disorder in the neurovascular bundle, accompanied by the formation of stones or denticles (replacement dentin).
How to treat deep caries and pulpitis
At the initial stage of caries, remineralizing therapy is prescribed. Solutions containing calcium, fluoride and other minerals are applied to tooth enamel. If hard tissues are damaged, filling is performed. First, the dentist cleans the tooth of necrotic tissue, then applies a filling and polishes it. Deep caries, which has led to nerve damage, is treated by removing the pulp.
Treatment of pulpitis is no different from treatment of advanced caries. The doctor prepares the carious cavity, opens the mouth of the canal, removes the dead nerve, treats the tooth with an antiseptic solution and applies a filling. The procedure is performed under local anesthesia.
Pulpitis does not always lead to the need to remove the nerve. If the patient seeks help from a doctor immediately after the onset of acute tooth pain, the doctor uses a biological treatment method. It removes inflammation while preserving the nerve. However, even after a successful procedure, there is a risk of recurrence of the disease. Periodically, you will have to undergo radiography in order to detect the onset of the inflammatory process in time.
Classification of tooth pulpitis: forms and types
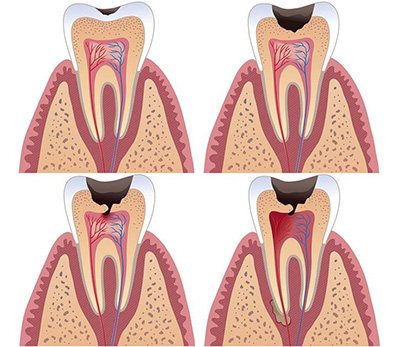
The disease is classified as acute, chronic or acute. All forms require careful examination and differ significantly from each other in treatment methods.
Chronic form
This is the most common form of this disease, occurring in fibrous, hypertrophic, and gangrenous forms. However, it is the most difficult to diagnose because the symptoms appear over a long period of time. Sometimes exacerbations follow one after another, then the pain subsides for a long time. Doctors often mistake painful outbreaks in a chronic disease for one of the forms of acute pulpitis. Therefore, a careful history taking is necessary.
- Fibrous pulpitis
is more common and is quite insidious, since in some cases symptoms may be absent for a long time. The patient is not bothered by painful attacks, there are no obvious signs of inflammation in the dental tissues, but irritants can cause a painful reaction. When visiting the dental office, deep pulpitis with extensive caries is discovered. - Hypertrophic
pulpitis looks like a polyp growing from a carious cavity. It gradually grows, bleeds and causes pain during meals. With this type of pulpitis, the tooth crown is destroyed, and the bone tissue of the root apex decreases. This is clearly visible on x-rays. - Gangrenous pulpitis
occurs with pronounced symptoms. The bone tissue of the tooth can be visually intact or affected by caries. Harmful bacteria irritate the pulp, it becomes painful, bleeds, and an unpleasant odor appears from the mouth. The tooth reacts sharply to high temperature. In some patients, pain appears in the first stages, and then gradually disappears. In such cases, with pulpitis, the entire nerve (pulp) is removed.
Acute form and stages of development
In this form, pathology often develops in a closed cavity of the tooth, that is, visually it looks intact and there are no obvious signs of caries. Pulpitis is accompanied by sudden pain, which quickly increases and gradually disappears. Its appearance is provoked by irritants in the form of hot and cold food. The following types of disease are distinguished.
- Focal pulpitis
affects only the upper part of the tooth. Irritants cause paroxysmal pain in the pulp, lasting 10 - 20 minutes with fairly long breaks. The affected tooth is easily identified by the unpleasant sensations when pressing on it. - Diffuse pulpitis
develops from focal pulpitis after 1 - 2 days, if treatment measures are not taken in a timely manner. The inflammatory process has already affected the coronal part of the pulp, and root pulpitis develops (inflammation affects the roots). The pain occurs without external irritants and does not subside for a long time, sometimes for 3–5 hours. Most often, attacks occur at night. Several teeth hurt at once; the source of inflammation is almost impossible to determine. Pulpitis of the upper tooth radiates to the ear, temple, back of the head, and of the lower tooth - to the neck. Attacks can torment the patient for up to 2 weeks. - Purulent pulpitis
is the next stage with an increase in the inflammatory area, sudden and prolonged acute pain. It may subside if cold is applied to the cheek, and intensify when exposed to heat. Pus accumulates in the pulp, which can cause intoxication of the body with elevated body temperature.
Other types
- Retrograde pulpitis.
It is difficult to visually determine the presence of this pathology, since the surface of the tooth remains unchanged. The infection enters the pulp through the apical foramen. This process occurs against the background of chronic osteitis, osteomyelitis, and actinomycosis. Signs of the disease do not appear for a long time, and it can only be diagnosed through x-rays. In later stages, symptoms resemble a purulent form. - Traumatic pulpitis.
A rare pathology, the cause of which is not an infection, but a tooth injury due to an impact, poor-quality treatment, toxic effects, or taking medications that negatively affect the condition of the teeth. However, the manifestations of the pathology are similar to the symptoms of pulpitis in an acute infectious form. The tooth is treated by removing the pulp, but in some cases it can be saved. - Three-channel pulpitis.
Permanent teeth with three canals (chewing) also have three pulps. Accordingly, the dentist faces a much more difficult task of removing them and cleaning the canals. In modern clinics, such cases are treated using a microscope, since the work is painstaking and time-consuming.
Prevention of caries and pulpitis
To reduce the risk of developing these pathologies, the following rules should be followed:
- brush your teeth twice a day;
- Rinse your mouth after every meal;
- do not pick your teeth with sharp objects;
- come to the dentist for examination twice a year;
- stop smoking;
- limit your consumption of sweets.
If you experience pain or discomfort in your teeth, consult your doctor immediately. In some cases, caries and pulpitis develop rapidly. You can lose a tooth in just a few months. The incisors and canines that fall into the smile zone are especially vulnerable. After their removal, implants will have to be installed. Lack of treatment can lead to other complications, for example, periodontitis - inflammation of the ligamentous apparatus of dental tissues. This pathology leads to tooth loss and can cause bone infection.
Possible consequences of treating pulpitis
No matter how well the therapy procedure is carried out, there is a chance of developing complications of pulpitis. After treatment, there is a risk of tooth fracture. To avoid this, the patient is given a crown, and if the tooth walls are adequately preserved, restoration is carried out with a photopolymer.
As a complication, in the absence of timely treatment, periodontitis may develop. The disease is accompanied by an acute inflammatory reaction in the tooth and adjacent tissues. The complication has several stages. In the first case, the inflammatory process can be stopped and the tooth can be saved; in the second case, it is removed.

Although x-rays are not able to unambiguously determine the presence of pulpitis, the study remains a key point in diagnosing the pathology. Thanks to an x-ray, the dentist identifies indirect signs of pathology, begins timely treatment and saves the tooth.
Causes
Pulpitis is inflammation that is caused by infection. The most common causes are lactobacilli, staphylococci, and streptococci.
When these microorganisms get inside the carious cavity, microcracks in the enamel, which leads to destruction of the surface. Their goal is to get to the nerve. Therefore, it is often important to treat the entire body to prevent the infection from spreading further. But treatment of tooth pulpitis should only be prescribed by a doctor.
The list of treatments for dental pulpitis includes:
| — Mechanical and medicinal treatment of 1 channel |
| — Pulpitis (simple) root canal filling with three-dimensional obturation system E&Q Plus (1k/k) |
| — Pulpitis (simple) root canal filling with three-dimensional obturation system E&Q Plus (2k/k) |
| — Pulpitis (simple) root canal filling with three-dimensional obturation system E&Q Plus (3k/k) |
| — Pulpitis (complex) filling of root canals with the E&Q Plus three-dimensional obturation system (1k/k) |
| — Pulpitis (complex) filling of root canals with the E&Q Plus three-dimensional obturation system (2k/k) |
| — Pulpitis (complex) filling of root canals with the E&Q Plus three-dimensional obturation system (3k/k) |
Complications of pulpitis
Failure to see a dentist in a timely manner will lead to inflammation spreading to bone tissue and to the development of periodontitis. This will make the treatment more complicated, and the most likely outcome will be tooth extraction. This complication can also occur with improper treatment. If the doctor introduces an infection into the canals or the tightness of the fillings is insufficient, complications cannot be avoided. Experts recommend using treatment technologies with insulating curtains. Cleaning and processing of canals is carried out much better when using a visiograph, operating microscope, endomotor or binocular.