5.1.2. Platelets
Platelets are formed in the bone marrow by megakaryocytes - giant multinucleated cells, from whose cytoplasm they are detached. The platelet has the appearance of a round biconvex disk with a diameter of 2-4 microns. The normal lifespan of platelets is 7-10 days.
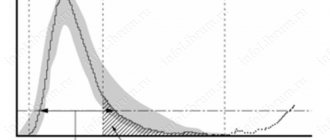
The number of platelets in the blood of a healthy person is 170-350x109/l. A decrease in the number of platelets is called thrombocytopenia, an increase is called thrombocytosis. Thrombocytopenia less than 80-100x109/l contributes to the appearance of bleeding, the risk of which increases sharply at levels below 20x109/l; thrombocytosis over 800x109/l creates a risk of developing thrombosis.
Along with the number of platelets, the functional usefulness of the cells (including those associated with the presence of their inhibitors in the blood), as well as the pathology of other components of the hemostatic system, are of great importance in the development of hemorrhagic syndrome. For example, with autoimmune thrombocytopenia, severe bleeding usually occurs when the number decreases to less than 20x109/l, while in disseminated intravascular coagulation syndrome, accompanied by complex disorders of hemostasis, a life-threatening hemorrhagic syndrome can develop at a platelet level of 80-100x109/l.
Normally, more than two-thirds of platelets are in the peripheral blood, the rest are deposited in the spleen, from where they enter the bloodstream as needed. In the absence of a spleen, the peripheral blood contains about 90% of the total number of platelets. In patients with splenomegaly or hypersplenism, the splenic pool increases sharply, and the platelet content in the portal vein is significantly higher than in the peripheral blood. The bone marrow is also a site of platelet deposition, but to a much lesser extent.
5.1.1. Endothelium
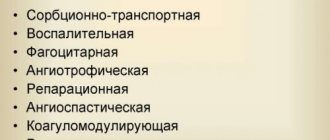
The vascular endothelium is the main barrier between the blood and other tissues of the body and at the same time it is the site of transport, synthesis and deposition of a large number of biologically active substances that are directly involved in hemostasis.
Endothelial cells directly or indirectly take part in all the main processes of hemostasis:
1) maintain the integrity of the vessel (by providing subendothelial connective tissue with collagen, elastin and fibronectin);
2) participate in the organization of laminar blood flow;
3) synthesize biologically active substances that cause constriction or expansion of blood vessels;
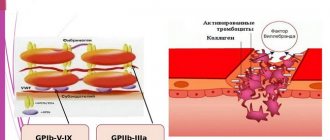
4) synthesize powerful inhibitors of platelet adhesion and aggregation; 5) participate in the activation and control of coagulation and fibrinolysis systems (by synthesizing and depositing individual factors, as well as providing a cell membrane for their interaction);
6) remove vasoactive substances, platelet aggregation agonists, and some factors of secondary hemostasis from the bloodstream.
Death or damage to endothelial cells, on the one hand, contributes to the development of bleeding, on the other hand, it triggers the hemostasis mechanism. The latter is due to the fact that contact with collagen, which is contained in large quantities in the subendothelium, exposed after the death of the endothelium, is a signal for the adhesion and activation of platelets, as well as the activation of secondary hemostasis systems (coagulation and fibrinolysis).