Reasons for decreasing and increasing aggregation
Increased aggregation level or hyperaggregation is a condition in which blood flows slowly through the vessels and quickly clots. Provocateurs of such deviation can be:
- diabetes;
- hypertonic disease;
- cancer of the kidneys, gastrointestinal tract or blood;
- vascular atherosclerosis;
- leukemia;
- sepsis;
- lymphogranulomatosis;
- surgical excision of the spleen;
- menstruation in women.
Moderate platelet hyperaggregation during pregnancy is normal. This deviation occurs due to the need to nourish the placenta with blood. The value reaches its peak in the 3rd trimester of gestation.
A decrease in platelet aggregation occurs due to the following pathologies:
- thrombocytopathy;
- diseases of the hematopoietic system;
- use of antiplatelet agents;
- renal failure;
- dysfunction of the thyroid gland;
- anemia;
- alcohol abuse.
Platelet aggregation
Platelet aggregation
To assess platelet function, CIR Laboratories LLC performs an analysis for induced platelet aggregation. This is a high-quality analysis performed on an automatic aggregometer.
To assess platelet function, the CIR Laboratory performs an analysis for induced platelet aggregation. This is a high-quality analysis performed on an automatic aggregometer. Since this test changes dramatically when taking drugs that affect blood clotting (antiplatelet agents, for example, aspirin, thromboass, anticoagulants, for example, heparin), it is advisable to take it before starting to take these drugs. For each aggregogram, the laboratory doctor issues a conclusion.
A platelet aggregation test is recommended in the following cases: miscarriage, unsuccessful IVF attempts, a history of severe pregnancy complications, infertility of unknown origin, as well as increased bleeding: easy bruising, menorrhagia, nosebleeds.
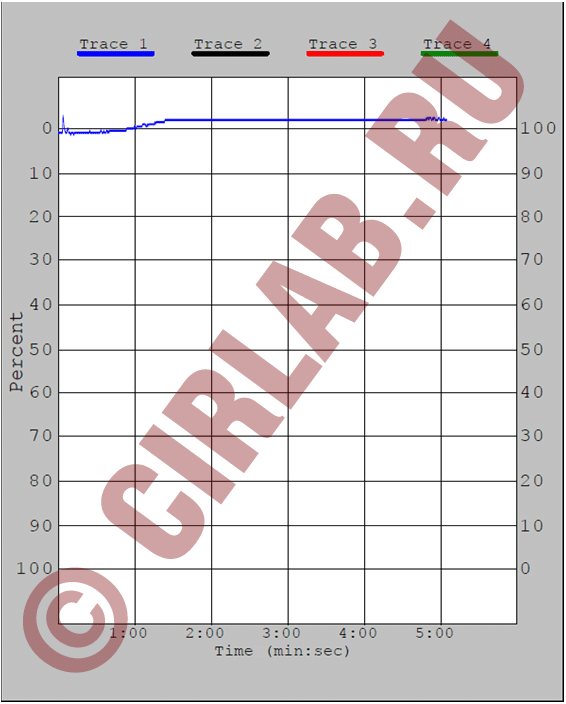
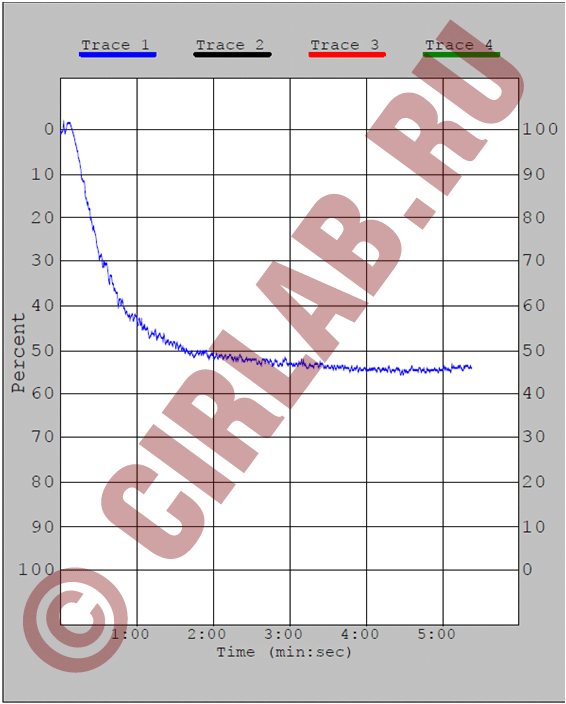
The aggregation curve evaluates the amplitude of aggregation, the shape of the curve, the presence of one or two waves, and the presence of disaggregation.
The sample shown shows: 1—zeroing of the device, 2—before adding the inductor, 3—peak associated with dilution of the sample by the inductor, 4—reference point, first wave, 5—second wave, 6—disaggregation.
Important information: the combination of taking foods, herbal medicines and nutritional supplements containing components from this list with taking antiplatelet agents (thromboASS) and anticoagulants (heparin) is a dangerous combination due to the risk of bleeding (category D according to the FDA classification). The risk of bleeding in most cases outweighs the potential benefit.
More details At CJSC Laboratories CIR, platelet aggregation is performed with the following inducers:
- Aggregation with ADP
- Aggregation with arachidonic acid
- Aggregation with adrenaline (epinephrine)
- Aggregation with ristocetin. The first three inducers make it possible to evaluate the function of platelets from different sides; they complement each other. Aggregation with ristocetin allows one to suspect a dangerous bleeding condition - von Willebrand disease (von Willebrand factor deficiency). When planning a pregnancy, this analysis is important to eliminate the risk of bleeding during childbirth.
Aggregation with ADP (blue line) and arachidonic acid.
The aggregation response is sharply reduced. There is virtually no disaggregation.
Aggregation with ADP.
The aggregation response is reduced. There is virtually no disaggregation.
(aspirin has the maximum effect)
Aggregation with arachidonic acid. There is no aggregation response. A common situation when taking non-steroidal anti-inflammatory drugs
Also, platelet aggregation with ADP and adrenaline may decrease.
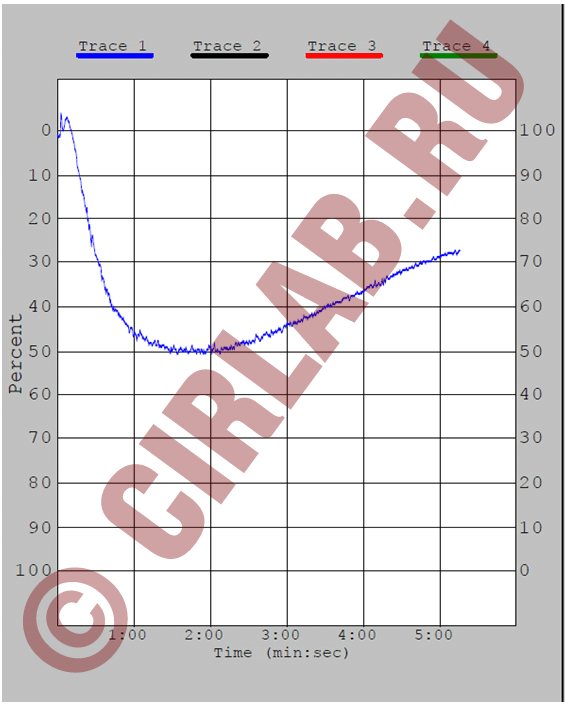
Aggregation with ADP, response reduced. Partial disaggregation.
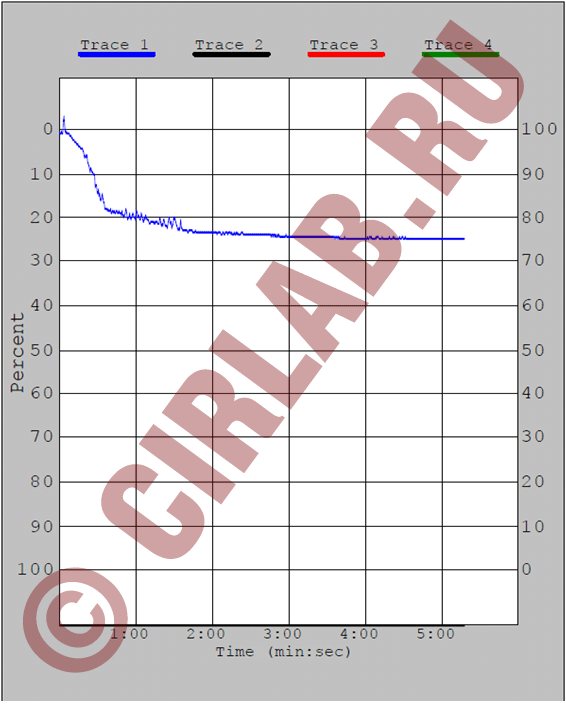
Aggregation with ristocetin, the aggregation response is sharply reduced.
The analysis is given in Maryino on weekdays and Saturdays from 9.00 to 11.00, on Tretyakovskaya and Voykovskaya on weekdays from 8.00 to 10.00.
What medications affect platelet aggregation?
| Pathogenetic mechanism | The way to realize the impact | Drugs |
| Inhibitors of thromboxane A2 formation | ||
| Phospholipase inhibitors | Prevents the formation of arachidonic acid, inhibits collagen, ADP and adrenaline aggregation | Quinacarpine, high-dose corticosteroids |
| COX inhibitors | Acythelate platelet and COX membranes, block the formation of prostacyclin in the endothelium, inhibiting aggregation and release reactions. Against the background of drugs that block COX, arachidonic acid levels are sharply reduced. | PVP (aspirin, indomethacin, butadione, ibuprofen, sulpirazone), indocid, fenoprofen |
| Thromboxane synthetase inhibitors | They block the synthesis of thromboxane A2 without affecting the synthesis of prostacyclin. Inhibits aggregation under the influence of arachidonic acid | Prostacyclin and its synthetic analogues, imidazole and its derivatives (individual sensitivity) |
| Competitive antagonists of thromboxane A2 | Block thromboxane receptors and inhibit aggregation. Inhibits aggregation under the influence of arachidonic acid | 1,3-Azoprostanoic acid and its derivatives |
| Drugs that increase cAMP levels in platelets | ||
| Adenylate cyclase stimulators | They block the synthesis of thromboxane A2 without affecting the synthesis of prostacyclin. Inhibits aggregation under the influence of arachidonic acid. | Prostacyclin, PGE, diterpene foscolin |
| Phosphodiesterase inhibitors | Prevents cAMP degradation. Inhibit platelet adhesion to the subendothelium, the second wave of aggregation, disrupt the release reaction | Dipyridamole, papaverine, aminophylline, intensain |
| Stimulators of prostacyclin synthesis | They enhance the synthesis of prostacyclin, its release from the endothelium, and weaken its degradation | Anabolic steroids, nicotinic acid, vasopressin |
| Drugs that interfere with calcium transport | ||
| Suppress the second wave of aggregation | Isoptin, nifedipine | |
| Impairs the adhesive-aggregation function of platelets | Furosemide in high concentrations | |
| Disrupts the initial and second wave of ADP-collagen- and adrenaline-platelet aggregation | Nitrofurantoin, aminazine, imipramine, amitriptyline, antihistamines, α- and β-blockers, high (over 20 million units/day) doses of penicillin, carbenicillin | |
| Drugs of different groups | ||
| Anticoagulants | In high concentrations they reduce aggregation | Pelentan, warfarin |
| Dextrans | Reduce platelet aggregation | Reopoliglyukin |
| Anesthetics | Reduce ADP aggregation | Nitrous oxide, cyclopropane, phenobarbital |
| Alcohol | Reduces collagen and ADP aggregation | |
| Antiplatelet agents | Reduce all types of aggregation, significantly enhance the effect of prostacyclin, disrupt the connection between platelets and fibrinogen | Tiklid |
Presentation “Platelet aggregation”
- what is platelet aggregation
- What are platelet granules and what do they contain?
- what platelet activators are there in a living organism and what does the laboratory use?
- requirements for conducting research
- factors affecting platelet aggregation
- interpretation of aggregograms
Assessment of platelet aggregation and pregnancy planning What are you taking?
Effect of drugs on platelet aggregation The use of four inducers in the analysis of platelet aggregation, APS, gene polymorphism Reduced aggregation, polymorphism of hemostasis genes, coagulogram Why take platelet aggregation before pregnancy? Aggregation cost Tags:
Aggregation, ADP, platelets, von Willebrand disease, aspirin
Back to section
Indications for analysis
Platelet aggregation is studied when:
- hemorrhagic disorders (increased bleeding);
- thrombophilia (coagulation disorder with an increased risk of thrombosis);
- severe atherosclerosis;
- diabetes mellitus;
- before performing surgical interventions;
- during pregnancy;
- when monitoring the effectiveness of anticoagulant and antiplatelet therapy.
Also, this study is important in the diagnosis of hereditary hemorrhagic thrombocytopathies.
Carrying out analysis and deciphering it
The study of platelet aggregation makes it possible to detect deviations from the norm and diagnose pathologies of the cardiovascular or hematopoietic systems. The procedure is necessary to monitor the dynamics of the course of certain diseases and control the treatment.
After collecting the biological material, special substances are added to the blood - inducers, which are similar in structure to the cells of the body that promote thrombus formation.
The inductor can be:
- adenosine diphosphate or ADP - platelet aggregation with ADP is considered the most common test method;
- adrenalin;
- ristomycin;
- arachidonic acid;
- collagen;
- serotonin.
The method for establishing aggregation is based on the passage of light waves through the blood plasma both before and after clotting. The following properties of the light wave are taken into account:
- What does it mean that platelet aggregation with ADF is reduced in the analysis?
- character;
- form;
- speed.
All this happens in a machine called a platelet aggregation analyzer. The equipment is available in every Helix laboratory service.
The analysis is deciphered by a hematologist, and the indicator depends on the substance that was added to the test liquid and its concentration.
| Inductor | Aggregation rate (%) |
| AT with ADF | from 30.7 to 77.7 |
| Platelet aggregation with adrenaline | from 35 to 92.5 |
| AT with collagen | 46,4–93,1 |
| AT with ristomycin | 30–60 |
What is “platelet aggregation”
Platelets are colorless blood cells whose function is to protect the body from blood loss. When body tissues are damaged, platelets immediately rush to the site of injury and block it, preventing excessive blood loss. This blocking occurs due to the fact that platelets instantly stick together and form a block that closes the wound. This blocking process is called platelet aggregation. The process occurs in two stages:
- Blood cells stick together
- Later they adhere to the walls of the vessel, forming a blood clot or thrombus.
When the body is healthy, this function is protective. But if pathological changes occur in the body, the formation of blood clots can disrupt nutrition in vital organs and tissues.
Platelet aggregation is normal
As noted above, when setting the degree of platelet aggregation, several types of inducers of this process can be used. This is why platelet aggregation rates may differ depending on the nature of the reagent used. Imitation of blood platelet gluing is performed on glass with the addition of an inductor. These substances normally trigger blood clotting reactions in the human body. Of those used, only ristomycin (ristocein) has no biological analogues in the human body. Each inductor has its own norm.
Platelet aggregation with ADP
It is worth noting that to obtain a complete picture and for the purpose of accurate diagnosis, an analysis to determine platelet aggregation can be performed alternately with four inducers. ADP-induced platelet aggregation is often the first to occur. Normally, this indicator is within the limits 30,8–77,8%
. When platelet aggregation does not fit into the above values, doctors exclude the presence of the following types of diseases:
- myocardial infarction;
- ischemia;
- diabetes;
- arterial hypertension;
- thrombopathy of hereditary origin;
- cerebrovascular accident;
- thrombocytopathy in hemoblastosis.
Platelet aggregation with adrenaline
The study of platelet aggregation using adrenaline as an inducer is an informative diagnostic method. This method fully reflects the internal mechanism of activation of the blood vessel restoration process. The value taken as the norm is 35,0–92,5%
. An excess of the indicator indicates hyperaggregation, a decrease indicates hypoaggregation. Increased platelet aggregation is associated with a high concentration of platelets in the blood, pathology, stress, and taking a number of medications.
Platelet aggregation with ristomycin
When assessing how platelet aggregation occurs in the body, ristomycin helps to simultaneously identify von Willebrand syndrome. This disease is hereditary. The spontaneous aggregation of platelets that accompanies the disease is characterized by the appearance of periodic bleeding, which is similar to that occurring in hemophilia.
However, with this pathology, bleeding lasts longer, since the patient experiences a violation of all three parts of hemostasis at once. Doctors can also use an analysis with ristomycin when assessing the effectiveness of antiplatelet therapy and selecting the correct dosage of the drug. Normally, the values should be in the range 56–167%
.
Platelet aggregation with collagen
Often, doctors cannot determine exactly which stage of blood coagulation is impaired: platelet adhesion or aggregation - a collagen test helps determine this. If, with this type of study, doctors record an excess of the established standards, this indicates a failure of the adhesion process. Platelets cannot attach normally to the endothelium of damaged blood vessels, so bleeding does not stop for a long time.
The presence of pathology is judged by the discrepancy between the parameter values and the established norm. For the collagen test, platelet aggregation should be 46,5–93,2%
. Exceeding these values or decreasing the parameter indicates:
- Reasons for the decrease in the number and average volume of platelets in the blood
- thrombopathy;
- hemoblastosis;
- disorders of the cardiovascular system.
Platelet aggregation with ADP
Platelet aggregation with ADP
— diagnostic assessment of activation of the platelet adhesion (aggregation) reaction using a special aggregation inducer - adenosine diphosphate (ADP).
ADP promotes platelet sticking (aggregation). The platelet aggregation test with ADP allows you to assess platelet function by studying their aggregation under the influence of an aggregation inducer. The analysis helps diagnose diseases of the blood coagulation system. T platelets
are blood cells that are responsible for clotting. Conditions associated with decreased platelet aggregation include inherited and acquired disorders of cell function. Platelet aggregation testing is performed to identify and diagnose platelet dysfunction in patients with excessive bleeding.
When vessels are damaged, platelets accumulate at the site of damage, are activated and stick to each other, forming a platelet thrombus, and a primary hemostatic plug is formed, which helps stop bleeding and heal the wound. When platelets are activated, a reaction occurs that culminates in the activation of phospholipase. As a result, the cell membrane changes properties and can come into contact with neighboring cells. As a result, platelets can aggregate with each other and form a platelet thrombus.
Aggregation
- the property of platelets to connect with each other. Adhesion is the ability of platelets to adhere to damaged vessel intima. Thus, adhesion and aggregation are processes necessary for the formation of a so-called “plug” to close the lesion in the vascular wall. Increased activation of platelets in pathology can lead to excessive thrombus formation and, conversely, when aggregation slows down, hemorrhages (bleeding) can occur.
Platelet activation
- a necessary element for normal hemostasis. Under normal conditions, circulating platelets do not interact with the inner surface and endothelial cells of blood vessels. But when the vessel wall is damaged, collagen comes out into the lumen of the vessel and platelets, with the participation of von Willebrand factor, adhere (adhesion) to the damaged area of the vessel. Increased platelet aggregation is accompanied by coronary heart disease and the development of myocardial infarction.
Indications:
- diagnostic evaluation of excessive bleeding or increased bleeding;
- assessment of platelet function in pregnant women;
- monitoring platelet function before complex surgical operations.
Assessment of platelet aggregation is useful during antiplatelet drug therapy.
Low doses of aspirin are prescribed to prevent blood clots in patients suffering from atherosclerosis and diseases of the cardiovascular system. Platelet aggregation analysis allows us to predict the body's response to antiplatelet drugs. Several other drugs may affect platelet aggregation, including antibiotics, antihistamines, clopidogrel, dipyridamole, nonsteroidal anti-inflammatory drugs, theophylline, ticlopidine, and tricyclic antidepressants. Preparation
No special preparation required. It is recommended to take blood samples no earlier than 6–8 hours after your last meal. On the eve of the study, alcohol consumption, smoking, physical and emotional stress should be avoided.
If the patient is taking medications, you should consult with your doctor about the advisability of conducting a study while taking medications or the possibility of discontinuing it before the study; the duration of withdrawal is determined by the period of removal of the drug from the blood.
Interpretation of results
The interpretation of the test is based on an analysis of the nature of aggregation (one- or two-wave, complete or incomplete, reversible or irreversible), as well as some other indicators.
Units of measurement: % As a percentage, the norm corresponds to 25–75%.
Factors that increase results:
- heparin;
- blood sample hemolysis;
- lipemia;
- nicotine.
Factors that reduce the result:
- excessive consumption of garlic (inhibits platelet aggregation);
- aspirin (acetylsalicylic acid inhibits platelet aggregation by blocking the synthesis of thromboxane A2);
- azlocidine, captopril, carbamate, carbencillin, chloroquine, chlorpromazine, clofibrate, cyproheptadine, dextran, dipyridamole, diuretics, flumenic acid, hydroxychlorin, isosorbide dinitrate, mezlocillin, moxalactam, nifedipine, nitrofurantoin, penicillin, phentolamine, piperacillin , promethazine, propranolol, prostaglandin E1 , pyrindole, sulfinpyrazone, ticarcillin, tricyclic antidepressants;
- thrombocytopenia.
Deviations from the norm Abnormal platelet aggregation is combined with the following conditions:
- platelet disorders caused by deficiency of membrane glycoprotein receptors, deficiency of storage sites, deficiency of ADP release;
- lack of plasma proteins that ensure the interaction of platelets with the walls of blood vessels, including von Willebrand factor, fibrinogen, fibronectin;
- the presence of abnormal metabolites and plasma components in uremia, dysproteinemia, disseminated intravascular coagulation syndrome;
- collagen-vascular disorders (Marfan syndrome, osteogenesis imperfecta);
- myeloproliferative disorders (essential thrombocythemia, polycythemia vera, chronic myeloid leukemia);
- Glanzmann's thrombasthenia (Glanzmann): deficiency of glycoprotein IIb/IIIa; absence of aggregation under the action of ADP, collagen, adrenaline, thrombin, but normal aggregation under the action of ristomycin;
- Bernard-Soulier syndrome (Bernard-Soulier): deficiency of Ib, normal aggregation under the influence of ADP, collagen, adrenaline, insufficient agglutination under the influence of ristocetin. Unlike von Willebrand's disease, agglutination due to the action of ristomycin is not corrected by the addition of normal plasma;
- deficiency of storage spaces/pools (Chediak-Higashi syndrome, glycogenosis type I, gray platelet syndrome, Hermansky-Pudlak syndrome, TAR thrombocytopenia syndrome/pathia with Aplasia of the Radius. This syndrome belongs to the group of congenital pathologies of the megakaryocyte-platelet apparatus, combined with abnormalities of the bone apparatus - bilateral absence of the radius with shortening of the forearms, sometimes with deformation of the spine, scapula, hip dysplasia, cleft palate, muscle defects, strabismus, pulmonary hypoplasia, congenital heart defects), Wiskot-Aldrich syndrome: platelet aggregation may be abnormal , often due to the absence or reduction of secondary ADP release;
- cyclooxygenase deficiency: abnormal platelet aggregation due to failure to activate the prostaglandin pathway; aspirin-like defect;
- von Willebrand disease: normal aggregation under the influence of ADP, collagen, adrenaline; absence or reduction of agglutination under the influence of ristocetin (with the exception of type IIB, where agglutination occurs at subnormal concentrations of ristocetin).
Decreased platelet aggregation
- taking acetylsalicylic acid, indomethacin, large doses of furosemide.
Normal platelet count in blood
To know the state of platelet levels, you need to have an idea of their normal level.
| Age | Indicator, x 10^9/l |
| Newborn | 100-420 |
| up to 1 year | 160-320 |
| from 1 year to 4 years | 150-300 |
| from 15 to 18 years old | 180-340 |
| Men over 18 years old | 180-400 |
| Women over 18 years old | 150-380 |
If we talk about the aggregation rate, then it is 25-75%. In this case, the process of platelet gluing occurs well and does not pose any health hazard.
What does platelet aggregation say in a blood test?
To study the ability of platelets to aggregate, the laboratory creates an imitation of natural conditions - the circulation of blood cells in the bloodstream.
This study is carried out on glass with the addition of inductor substances that normally participate in similar reactions in the human body:
- Adrenalin;
- Collagen;
- ADF;
- Thrombin.
Ristomycin (ristocein), which has no analogues in the human body, is additionally used as an inducer. Each platelet aggregation inducer has its own normal range, which differs slightly in different laboratory conditions.
Norm of platelet aggregation depending on the reaction inducer
| Method for determining platelet aggregation | Norm,% |
| Blood test with ADP | 30,8 – 77,8 |
| Blood test with adrenaline | 35,0 – 92,5 |
| Blood test with collagen | 46,5 – 93,2 |
| Blood test with ristomycin | 58 – 167 |
For the diagnosis of cardiovascular pathologies, the determination of spontaneous platelet aggregation, when plates of blood cells stuck together circulate through the circulatory system, is of great importance.
Disturbances in the microcirculation zone:
- Changes in vascular walls in the microcirculation zone;
- The formation of aggregates from platelets, which increases the risk of developing pathology of the heart and blood vessels and serious complications.
Methods for determining CAT parameters:
- Change in the optical density of a suspension of blood platelets;
- Visual assessment of platelet aggregation.
In laboratory conditions, to diagnose pathological platelet aggregation, the following is used:
- Optical aggregometers – record platelet aggregation in plasma;
- Conductometric aggregometers – measure the level of aggregation in whole blood.
The obtained data is displayed as a curve on the aggregogram. The method of laboratory diagnosis of the level of platelet aggregation is reliable, but requires high labor intensity and a large volume of blood plasma.