What is TORCH complex
The word TORCH means:
- T – toxoplasma (toxoplasma gondii);
- O – other infections (others);
- R – rubella (rubella);
- C – cytomegalovirus;
- H – herpes simplex.
The group usually includes the 4 above infections, but may include hepatitis C, chlamydia, syphilis, etc.
For more detailed information, you should make an appointment with an infectious disease specialist or gynecologist at the clinic.
What are ToRCH infections?
The abbreviation ToRCH comes from the first letters of the most dangerous infections for the fetus - Toxoplasma (toxoplasma infection) - Rubella (rubella) - Cytomegalovirus (cytomegalovirus) - Herpes (herpes). These are classic infections. In addition to them, they also talk about infections such as parvovirus (infection caused by parvovirus B19), listeriosis, hepatitis B and C and some others. All of them can affect people of any gender and age, but the term itself is used in relation to women who are preparing for pregnancy, pregnant women, as well as the fetus and newborn. Rubella, toxoplasmosis, cytomegalovirus and herpes infections are common infections. In most cases, the first encounter with them occurs in childhood and adolescence - this is called primary infection, after which immune protection remains. If the body encounters an infection again, it is called a secondary infection or reinfection.
Purpose of the survey
TORCH infections are often harmless to adults and occur with virtually no symptoms. Herpes and cytomegalovirus, once entering the body, remain there forever in latent form. If a person has had toxoplasmosis and rubella, then antibodies to these pathogens remain in his blood.
The main purpose of the examination is to identify seronegative pregnant women who do not have IgG antibodies, which indicate a long-standing infection. Only primary infection with TORCH infections is dangerous, since there is no developed immunity. In this case, there is a high risk of intrauterine infection, which can lead to fetal pathologies, miscarriage and stillbirth.
It is important to examine a woman before she plans to conceive. If IgG type immunoglobulins are diagnosed in the blood, then she can easily become pregnant. Otherwise, the doctor will advise you on how to avoid infection. Sometimes vaccination is recommended, for example, in the absence of antibodies to the rubella virus.
Why are TORCH infections dangerous?
Today, the TORCH complex includes diseases of a viral and parasitic nature that are especially dangerous during pregnancy. They are often asymptomatic or have mild symptoms, which makes their diagnosis difficult.
TORCH infections are a condition that includes the following diseases:
| Disease | Description |
| T – toxopla-smosis (toxoplasmosis) | According to WHO, about a third of the world's population is infected with toxoplasmosis. The causative agent of the disease is the parasite Toxoplasma. The most likely source of infection is domestic cats. Infection is possible through household means or by eating meat products that have not undergone full heat treatment.
The consequences of toxoplasmosis will be termination of pregnancy or severe damage to the organs of vision, liver, and central nervous system of the unborn child. The disease is most dangerous in the first 8 weeks of pregnancy. |
| R – rubella (rubella) | A viral disease, the causative agent of which is transmitted by airborne droplets. An infected person is able to infect others even before the first signs of the disease are detected and within a week from the moment they appear. Symptoms (rash, malaise, mild fever) are mild. Women who have been ill several months before conception develop strong immunity, which will protect the unborn child. However, primary infection at the very beginning of pregnancy is so dangerous that doctors raise the question of terminating it. The consequences of infection for a period of more than 12 weeks will be a lag in the physical and mental development of the born baby, as well as numerous pathologies. Timely treatment will help reduce the risk of their development. |
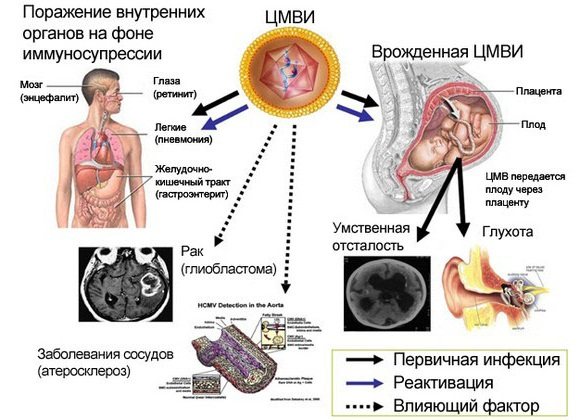
| C – cytomeg-alovirus (cytomeg-alovirus) | The causative agent of the disease is the CMV virus, which is transmitted through sexual contact with a carrier, through shared utensils, and also during pregnancy. The disease is asymptomatic; upon recovery, stable antibodies are formed in the blood that last for life. The virus, having entered the latent phase, remains in the body and can be activated when the immune system is weakened for one reason or another, in particular due to pregnancy. During primary infection of the expectant mother, the risk of infection of the fetus is especially high. The infection can also be caused by the father if his semen contains cytomegalovirus. During a short period of pregnancy, the disease often leads to the death of the embryo or to the birth of a child with congenital CMV infection. It can manifest itself as a list of incurable diseases, including cerebral palsy, cerebral edema, and muscle weakness.
|
| N – herpes (herpes) | This is a group of viral infections that affect the mucous membranes of the nose, eyes, mouth (herpes type 1) or the reproductive system (herpes type 2). Over time, patients develop antibodies, and the herpes virus enters an inactive phase. Thanks to this, symptoms of the disease appear only when the immune system is weakened. Infection of a pregnant woman who has not previously been ill with herpes can lead to a frozen pregnancy or miscarriage. The list of other negative consequences includes external deformities, the birth of a child with eye pathology, microcephaly, and severe diseases of the cardiovascular system. |
| О – others (other infections) | Various diseases of viral and parasitic etiology, which pose a serious danger not only to the unborn child, but also to the pregnant woman herself. These include hepatitis B and C, chlamydia, syphilis, gonorrhea, listeriosis, AIDS, chicken pox, enterovirus infection. |
Indications for examination
When should a woman be tested for the TORCH complex:
- 2-3 months before planned conception;
- in the early stages of pregnancy (if necessary over time).
Newborns are also examined if there are suspicious symptoms.
The examination must be carried out regardless of how you feel, since the disease often occurs without pronounced symptoms. As a rule, a referral for analysis of the Torch complex is issued when a pregnant woman first visits a gynecologist.
Why is the examination carried out?
It is before pregnancy (or in the early stages) that we need to find out whether there was an infection or not. If there was, you don’t have to worry, this infection is not dangerous for a pregnant woman. If not, then the doctor will tell you about a set of preventive measures (for example, if we are talking about rubella, then you can get vaccinated, if we are talking about toxoplasma, you can follow certain rules to reduce the risk of infection, etc.). In addition, for those infections for which there are no protective antibodies, it is important to conduct regular monitoring so as not to miss an infection during pregnancy.
Description of the examination
To detect pathogens in blood serum, 2 methods are used:
- ELISA – enzyme immunoassay;
- PCR – polymerase chain reaction.
The price of the second method is much higher. The turnaround time for analysis is about 1 week.
Titers for immunoglobulins IgM and IgG are of diagnostic interest. IgM antibodies rise immediately after infection and indicate an acute stage. While IgG titers may indicate a chronic disease or carriage.
The cost of the TORCH panel consists of the price of a study on titers of immunoglobulins such as IgM and IgG for each infection. The herpes virus is tested for the first and second types (HSV 1 and HSV 2).
ToRCH infections and pregnancy
- Introduction
- What are ToRCH infections?
- Why are ToRCH infections dangerous?
- Why is the examination carried out?
- How is the diagnosis made and how is the examination carried out?
- Pre-pregnancy examination
- Examination during pregnancy
- Complementary and confirmatory studies: IgG antibody avidity
- Additional and confirmatory studies: immunoblot
- Read more about 6 dangerous infections
- How to get tested in the CIR laboratory?
- Dictionary
- Cost of tests
The process of deciphering the results
A positive or negative result is determined depending on the reference values of IgM and IgG immunoglobulins.
Table. Interpretation of the results of the TORCH complex and recommendations.
| Outcome options | Antibody type | Decoding | Recommendations | ||
| IgM | IgG | For pregnant women | When planning to conceive | ||
| 1 | — | — | No immunity to infection | Take precautions to avoid infection, undergo follow-up examinations | |
| 2 | + | — | Primary contact with the infection occurred 1.5-2 months ago | Urgently contact a gynecologist for treatment | Do not plan pregnancy in the next six months until immunity is formed |
| 3 | + | + | The infection occurred 1.5-4 months ago, immunity is developing | Conduct additional research | You can plan to conceive in the near future |
| 4 | — | + | Presence of immunity to infection, remission stage | Not dangerous for the fetus | |
A final diagnosis can only be made by a qualified doctor.
The essence of the analysis
Blood is taken from a vein of the pregnant woman, which contains antibodies to infections (immunoglobulins Ig). There are five classes of antibodies, but in this case only two should be determined - IgM and IgG. Many laboratories do only a comprehensive examination. But it is quite possible to find out whether the immunoglobulins you are interested in are available, which will cost less. The analysis can reveal not only the presence of antibodies, but also their quantity. The latter option is more preferable, as it gives the doctor maximum information. If necessary, it is possible to find out the time of infection by determining at what point immunoglobulin began to be produced.
How to protect yourself from TORCH infections
If antibodies to these pathogens are not detected in the blood, then you need to adhere to certain tactics to avoid infection.
Recommendations for protection against TORCH infections:
- Toxoplasma: wash fruits and vegetables thoroughly, heat-treat meat, do not contact animals.
- Herpes: do not contact people who have symptoms of the disease.
- Rubella: strictly limit contact with children.
- Cytomegalovirus: Wash your hands thoroughly with soap, especially after touching baby diapers. Avoid contact with children under 5 years of age if possible. If there are children in the house, then you need to have separate dishes for them.
Methods for detecting TORCH infections
The diagnosis cannot be established solely on the basis of the patient’s complaints and the presence of her clinical manifestations. The fact is that many infectious diseases have similar clinical symptoms. The most accurate method is laboratory diagnostics using the TORCH complex. In medical practice, two studies are used to identify the pathogen: serodiagnosis and PCR analysis. Bacteriological testing is much less commonly prescribed. But it still remains relevant for bacterial invasions: mycoplasmosis, gonorrhea, candidomycosis.
The most accurate method is laboratory diagnostics using the TORCH complex
The most informative are serological reactions (RIF and ELISA), which allow for highly accurate screening of pathogens of TORCH infections. The method identifies specific protective proteins - immunoglobulins (IG), which are formed in the body in response to pathogen penetration. The study is carried out quickly, the analysis does not take much time to prepare and submit biological material, which makes it the method of choice. It allows one to judge not only the presence of a pathogenic agent in the body, but also determines the duration of infection. This is critical in obstetrics because the negative impact of infection on the fetus depends on the timing of the disease.
In difficult situations, to make a diagnosis, a serological study is supplemented by the method of immunoblotting - detection of antibodies to individual proteins of the pathogen. The sensitivity and accuracy of advanced diagnostics is more than 97%. But this is an expensive and time-consuming process, so the doctor prescribes it only after a screening examination.
The PCR method has a high accuracy of identifying the pathogen, but does not allow one to judge the timing of the disease, so it is used less often. The polymerase chain reaction finds fragments of the pathogen's genetic material even in minimal concentrations. It remains the method of choice in cases of acute infection, when it is necessary to quickly obtain results.
Bacterial culture can only be used for a group of other infections, which includes some bacteria. Sowing will determine the strain of the microorganism and its sensitivity to antibacterial therapy. It cannot be used to detect viruses or other groups of the TORCH complex.
Only through laboratory methods can you obtain complete information about your condition and not worry about the health of your unborn child . The study will not be difficult, because the only thing that is required from the patient is to donate blood for urogenital and TORCH infections.
What is TORCH and how does this word stand for?
The first letters of the names of infections that are included in the TORCH group are included in this abbreviation. The decryption looks like this:
- T - toxoplasmosis;
- O - other infections (syphilis, chickenpox, parvovirus, listeriosis);
- R - rubella;
- C - cytomegalovirus;
- H - herpes.
Let's take a closer look at each of the diseases.
Toxoplasmosis (T)
This is a well-known infection that affects about 30% of the world's population. Its causative agent is Toxoplasma. The primary host of this microorganism, in whose body it lives and reproduces, is domestic cats, which, as a rule, are the cause of infection. In addition, infection with toxoplasmosis can occur through unwashed hands (this is how children usually become infected in kindergartens), as well as a carnivorous raw food diet (raw meat diet).
Other infections (O)
This group involves infections that can affect the fetus: hepatitis B and C, syphilis, chlamydia, gonococci, listeriosis. Recently, HIV, chickenpox, and enterovirus infection were included in this list.
Rubella (R)
Rubella can be transmitted to a healthy person from an infected person, often through airborne droplets. Rubella is considered to be a completely harmless “childhood” disease. Infection in childhood does not lead to any serious consequences. The disease manifests itself as small rashes all over the body and an increase in temperature from 38 to 40°. The insidiousness of rubella lies in the fact that the infection goes through a long incubation period during which there are no symptoms.
Cytomegalovirus (C)
Cytomegalovirus became known only in the 20th century. It can be transmitted to an adult woman through sexual intercourse, blood, or breastfeeding.
Herpes (H)
Herpes simplex is a viral disease. Medicine knows two types of herpes - herpes type I and herpes type II.
Type I herpes most often manifests itself as the well-known “cold on the lips.” Type II manifests itself in the genital area. It is transmitted sexually, by airborne droplets and in utero. In the case of an advanced chronic course, it affects not only the places where it manifests itself, but also the central nervous system, eyes and internal organs.
After the initial infection, antibodies are produced, which largely make it possible to prevent the progression of the disease.