Each of us has encountered infectious diseases at least once throughout our lives. All of them are caused by a large number of pathogenic agents: bacteria, viruses, protozoa and fungi. Microbiology includes millions of microorganisms that can lead to the development of infection in humans.
Some of them are opportunistic, others are obligate pathogens. In medicine, there are a huge number of laboratory methods to identify a pathogen. Each of them has its own disadvantages and advantages. The sensitivity and accuracy of the method are of great importance.
The most commonly used methods are genetic molecular and serological studies. Patients, receiving a referral for molecular and serological tests, wonder what it is and believe that this is a very complex examination. In fact, the process of passing the analysis does not exceed 5 minutes, and the information content ranges from 95-100%.
What is serological analysis
Serological tests are an important tool for identifying the cause of an infectious disease. Serodiagnosis is a specific blood test that is based on the interaction of antigens and antibodies in the serum.
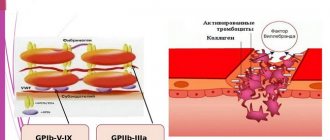
Antibodies are protein molecules formed in the human body a few days after contact with a pathogen. They are strictly specific for each infection and are produced to destroy the pathogen. Recognition of these protein fractions allows one to quickly identify the microorganism to which they were formed. Antigens are foreign proteins found in bacteria. The synthesized antibody finds an antigen in the blood and binds firmly to it, preventing it from having a detrimental effect on the body.
The binding reaction of these two proteins to form a single complex underlies the use of all serological reactions. To search for antibodies, special standard solutions with pathogen antigens (diagnosticums) are used, which are added to the blood being tested. Serodiagnosis determines all protein markers of infections, and subsequent interpretation of the results also provides information about the duration of the disease. This feature is characteristic only of serological analysis, which makes it the method of choice in many clinical situations.
Pros and cons of serological studies
With the help of serodiagnosis, geographic screening and mass diagnostics are carried out for preventive purposes to prevent epidemics. Other advantages:
- high reliability;
- quick interpretation of results – within 1 day;
- a large list of detected diseases;
- safety of analysis;
- the ability to monitor the effectiveness of treatment by the titer of Ag, At.
The disadvantage of the method is that when carrying out it is necessary to take into account the incubation period of the disease. Some infectious diseases have a “serological window” period - the virus is in the body, but antibodies have not yet entered the blood. The herpes virus can be detected after 2 weeks, HIV - after 1, 3, 6 months after infection.
Important! According to statistics, erroneous results account for 4% of the total number of tests performed. More often this is due to non-compliance with the rules of preparation for analysis, violation of the rules of diagnostics.
Advantages and disadvantages
The serological method of laboratory diagnosis has a large number of advantages, which has deeply introduced it into practical use in all branches of medicine: gynecology, urology, infectology and venereology.
Serodiagnosis is a publicly available test that provides rapid, accurate results. It does not require lengthy preparation for collecting material and is easily tolerated by all patients. To collect venous blood, the patient is required to follow a diet for only 48 hours. Serological tests also have high specificity (100%), sensitivity (95%) and accuracy (90-95%).
But this venous blood test requires a lot of expensive diagnostic tools, which also affects its cost. Some pathogens have weak immunogenicity, that is, the body produces few antibodies to them, so serodiagnosis is impossible. In addition, the method is much less often used for viral infectious pathologies, being inferior in efficiency to PCR analysis.
In what cases is it prescribed
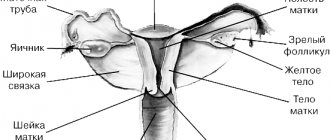
Serological laboratory blood tests are prescribed for the diagnosis of infectious diseases: bacterial, viral, protozoal, parasitic and mixed infections. Antibody detection is most widely used in obstetrics, gynecology and urology. In urology, this laboratory test is used for urethritis of unknown etiology, balanitis and balanoposthitis. In gynecology, they are referred for examination for any inflammatory process of the reproductive system (vulvovaginitis, colpitis, cervicitis and endometritis).
In obstetrics, every pregnant woman is prescribed a venous blood test to exclude diseases dangerous to the fetus. These infections are called the “TORCH complex” and are determined using serological tests. TORCH infections cause developmental defects in the developing fetus, often incompatible with life. That is why early and accurate diagnosis of these infections is the main goal of the obstetrician-gynecologist. Serology is also performed if male or female infertility is suspected due to infectious pathology.
If a doctor suspects a patient has a sexually transmitted infection, then a comprehensive examination is required, including serodiagnosis. If one of the partners is found to have a disease from the STI group, then the second partner must undergo testing, even if he does not have clinical symptoms.
Diagnostic methods
Serological reactions include several varieties.
All of them are based on the search for antibodies (immunoglobulins) and antigens, but are carried out in different ways and have different diagnostic criteria for diagnosis. Serological methods of laboratory research, depending on the methodology, are divided into simple and complex. The classification is based on how many proteins need to be found: simple reactions detect only antibodies or antigens, and complex reactions detect antigen + immunoglobulin complexes. A complex research method is more preferable because the sensitivity of the analysis is much higher. Most often in laboratories, serological diagnostics are represented by the following immunochemical seroreactions:
- immunofluorescence reaction (RIF);
- enzyme immunoassay (ELISA);
- indirect hemagglutination reaction (IRHA);
- complement fixation reaction (CFR).
These types of studies relate to complex seroreactions and have significant advantages over others. They are carried out extremely quickly, have high accuracy in diagnosing diseases and do not require lengthy preparation: the patient is only required to take a venous blood test.
Immunofluorescent reaction RIF
The immunofluorescence reaction (RIF), or Koons analysis, is a method for the rapid detection of antigens of a pathogenic agent in a patient’s biomaterial. To carry out RIF, a special dye is used - a fluorochrome, which can glow under a fluorescent microbiological microscope. Fluorochrome is added to the diagnostic serum with strict adherence to the concentration, otherwise the reaction may show false results. There are two types of immunofluorescence reaction: direct and indirect.
The direct Koons reaction detects only pathogen antigens. To determine them, a diagnostic serum consisting of antibodies and fluorochrome is added to the biomaterial. Antigens located on the cell wall of the pathogen bind to colored antibodies. The lab technician looks at the slide under a microscope and sees a bright green glow. A typical example of such a reaction is the detection of chlamydia contrasted with Evans blue.
Indirect RIF (IRIF) detects antigen-antibody complexes. To do this, the doctor sequentially adds unlabeled immunoglobulins to the sample first so that they bind to antigens. Then new serum is added to the formed immune complexes, containing antibodies already labeled with dye to the newly formed complexes. Most often, direct reaction is used to diagnose viral diseases.
The only drawback of these reactions is a certain degree of subjectivity when taking into account the results: the same glow intensity is sometimes assessed by doctors differently, which ultimately leads to false laboratory examination data.
Indirect hemagglutination reaction RNHA
RNGA is an analysis aimed at identifying immunoglobulins or antigens in various biological fluids.
The indirect hemagglutination reaction is one of the most accurate methods for determining the titer of immunoglobulins, which allows us to judge the stage of the infectious process. A 4-fold increase in immunoglobulin titer in two blood tests taken several weeks apart indicates an acute infectious process of bacterial or viral etiology. RNGA allows the attending physician to prescribe the correct drug therapy, taking into account the stage of the disease. The test is widely used to detect STIs, meningococcal infections, botulinum toxin (botulinum toxin) and most viral infections. To conduct the study, red blood cells are used - erythrocytes, on the surface of which antigens or antibodies are located. The serum is called antigenic or antibody erythrocyte diagnosticum. Diagnosticum is added to the blood being tested, then the reaction is observed. When these red blood cells attach to antigens or immunoglobulins in the blood, complexes are formed, and red blood cells begin to precipitate. If the test is negative, the red blood cells accumulate in a small button-shaped spot. If a sediment with scalloped edges in the form of an umbrella has formed at the bottom of the test tube or tablet, then the reaction is considered positive.
The difficulty in performing this serological test lies in the need for precise preparation of the erythrocyte diagnostic fluid and strict adherence to the concentrations of the components used.
Enzyme immunoassay ELISA
The enzyme immunoassay method is considered the most accurate, specific and sensitive seroreaction. The recording of ELISA results is automated, and the human factor and subjective assessment of data are excluded. The accuracy of the result reaches 98%, and with repeated testing – 100%. ELISA is used to diagnose sexually transmitted infections, HIV, viral hepatitis A, B, C, D, E, TORCH infections and many other diseases.
There are more than ten modifications of this analysis (direct, indirect, non-competitive, solid-phase, etc.), but they all have special, characteristic diagnostic features, but a similar principle. The phases of enzyme immunoassay serological reactions include the creation of an antigen-antibody complex, to which enzymes are added that act as a label. Then the material under study is placed on a special plate, placed in an automated system, and the search for complexes labeled with radionuclides begins. The analyzer identifies glowing marks, measures the optical density and degree of luminescence of immune cells, and then displays the analysis result.
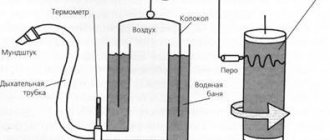
Immunofluorescence method.
"Glow" in a dark-field microscope
This method is based on the use of Abs labeled with a fluorescent substance. Most often, fluorescein isothiocyanate, which has a green glow in ultraviolet rays, is used as a label. The result of the analysis is assessed by the degree of brightness of the glow. A manual method of determination using a fluorescence microscope, an optical microscope with a fluorescent attachment, as well as an automatic method using a microchip cytometer, flow cytometer, or robotic fluorescence microscope can be used.
RIF is carried out by direct and indirect methods. The direct method means the direct binding of sorbed Ag to labeled Ab. The indirect method involves using unlabeled Ab to bind to Ag, and then adding labeled Ab, which avoids nonspecific reactions.
How to prepare for the test
The analysis does not require special preparation; all rules correspond to normal venous blood donation.
The patient is required to strictly follow a number of simple rules:
- 72 hours before the procedure, you should follow a diet: you should not eat fatty, fried, salty or spicy foods, alcoholic drinks are also prohibited;
- It is recommended to maintain optimal water balance in the body, and for this you need to drink at least two liters of clean drinking water;
- The venous blood test is carried out on an empty stomach, so at least 10 hours before the procedure you should not eat, drink tea, coffee or other drinks;
- Smoking is prohibited 4 hours before the procedure.
If for health reasons the patient is required to take any pills, it is necessary to notify the attending physician in advance. An hour before handing over the material, it is recommended to avoid physical activity, and before entering the treatment room, you should sit down and rest for 10-15 minutes.
Preparation
It is worthwhile to properly prepare for the study immediately in order to immediately obtain the most accurate results. What can cause unreliable test data:
- daily consumption of coffee, alcohol of any strength, foods high in fat and simple carbohydrates;
- prolonged exposure to the sun;
- taking medications with antimicrobial, antiviral or antibacterial properties;
- excessive physical activity, heavy physical activity during the day before the analysis;
- collection of biological material from patients who have only recently completed chemotherapy or antibiotic therapy.
A serological blood test from the ulnar vein usually needs to be taken in the morning. If the patient, for medical reasons, should not skip meals, then the analysis is carried out after five hours. It is necessary not to smoke at least 30 minutes before donating blood and agree on taking or stopping medications with your doctor. The study cannot be carried out if the patient is not feeling well - weakness, elevated body temperature, including due to an infection occurring in the body, or an exacerbation of any chronic pathology.
Analysis process
Venous blood is collected for serological testing in the first half of the day. The patient should arrive at the laboratory in advance, taking with him the necessary documents (passport and referral for analysis).
The patient is asked to go to the treatment room and sit comfortably on the chair. Blood is drawn from a vein located in the elbow area, so it is necessary to free the forearm and elbow area from things. A tourniquet is applied to the shoulder and a pillow is placed under the arm. The nurse puts on disposable sterile gloves and treats the puncture site with a cotton swab soaked in a disinfectant.
The algorithm for performing a venous injection includes pumping blood into a vein; for this, the patient is asked to clench and unclench his fist several times. In this case, the vessel is better visualized and palpated, which facilitates the collection of material. The nurse then inserts a syringe needle into the vein, draws 10 milliliters of blood, and applies a bactericidal patch to the injection site. To avoid the formation of a hematoma, after the manipulation you should bend your arm at the elbow for 15-20 minutes.
Decoding the results
For a correct diagnosis, serological reactions must be interpreted by a qualified specialist.
The detection of antibodies does not indicate the presence of the disease; in some cases, the circulation of immunoglobulins in the blood is the norm. Thus, IgM antibodies from measles, chickenpox, etc. are constantly present in our body. They are a marker of past infection and protect us from re-infection. Therefore, recording the results of a blood test and deciphering a serological study must be carried out individually for each patient. However, there are certain serological markers of infectious diseases:
- The detection of class A immunoglobulins to a virus or bacteria in the blood indicates an acute infectious process lasting no more than 14 days.
- If class M immunoglobulins are found in the blood, then advanced laboratory diagnostics are required, because these antibodies are a marker of both a previous illness and long-term infection.
- An increase in antibody titer by 4 or more times in two consecutive blood tests indicates the presence of an infectious disease.
- The detection of any pathogen antigens indicates that the pathogen is present in the body.
In case of an unclear diagnostic picture, repeated serological tests are carried out or the examination is supplemented with other research methods (PCR, bacterial culture, etc.)
What to do if sexually transmitted diseases are detected
If serological diagnostics confirms the presence of an STI, then it is necessary to immediately proceed to the treatment stage in order to avoid complications and chronicity of the process. The patient should make a second appointment with the attending physician. He will prescribe etiotropic complex treatment and will dynamically monitor the patient’s condition during drug therapy.
Title: Serological tests: what is it, a blood test to determine infections, how to take and decipher it, reaction methods to determine diseases
Description: What are serological tests and what diseases are they used to identify. How is a blood test done to determine infection? How to prepare, submit and decipher the result after receiving it. Methods of carrying out reactions to determine the disease.
What infections can a serological test help identify?
Serological markers are antigens or antibodies detected during the test. Serology is used to diagnose many infections:
- syphilis;
- HIV infection;
- viral hepatitis;
- herpetic;
- cytomegalovirus;
- chicken pox;
- measles;
- rubella;
- meningococcal;
- borreliosis;
- typhoid fever;
- yersiniosis;
- helicobacter pylori;
- mycoplasma;
- chlamydial;
- toxocariasis;
- toxoplasmosis;
- echinococcosis.
A blood test for parasites is informative if they are extraintestinal, that is, they live in the tissues. Such parasites cannot be detected using stool analysis.