Mucus in a smear is one of the indicators that help assess the condition of the patient’s urogenital tract.
Everyone knows that this indicator is present both normally and with deviations. The characteristics of the discharge, its abundance and other indicators that need to be understood are of significant importance.
Patients often ask what tests are recommended to be taken when abnormalities are detected, and which doctor can help in identifying abnormalities.
What does the appearance of discharge in men mean, and is an infectious process always to blame?
Features of mucus secretion in women
Mucus in a smear in women frightens a significant number of representatives of the fair sex who see this indicator in the results of their research. In fact, as doctors note, there is no reason to be afraid. The presence of mucous discharge is not a reason to make terrible diagnoses or begin active treatment.
It rather acts as an indicative indicator by which the condition of the lower parts of the genitourinary system is judged.
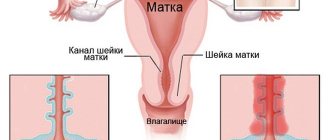
Normally, the indicator can be determined as follows:
- urethral canal
- in the vagina
- in the cervix
Normally, most women do not have mucus in the urethra. In the analysis, this is designated as a minus.
In the vaginal area, the amount of discharge may be scanty, which will be indicated by a single plus.
The area of the cervix may be largely filled with mucus, which is indicated by a pair of pluses or a three. Three pluses are a reason to be wary, but not to make any diagnosis and begin treatment.
To draw any conclusions about the state of women's health, it is necessary to evaluate not just the presence of mucus, but its combination with other indicators. Otherwise, it is impossible to talk about the objectivity of the conclusions.
Combination of mucus with leukocytes
Often patients, having seen the results of their studies, are interested in what indicators should be used to evaluate the presence of a mucous component in the smear.
After all, if this indicator is not assessed separately, then there is an indicator that gives it greater significance.
First of all, it is recommended to evaluate leukocytes and mucus in the smear. Leukocytes are the first immune cells that respond to infection entering the genital tract.
Moreover, their highest concentration is observed directly in the inflammation zone. As you move away from it, their number gradually decreases.
The presence of leukocytes in excess indicates that there is an inflammatory process in the body. The nature of which is most likely infectious. In some cases, opaque mucus is detected in the smear, which is combined with leukocytes. Such a deviation most often indicates that the patient has developed an infectious process.
It is important to understand that it can be both specific and non-specific. As doctors note, much depends not only on the presence of leukocytes, but also on their number. Normally, women have the most of them in the cervical canal. There you can count up to 30 cells of the immune system. The smallest is in the urethra area, usually no more than 5 pieces.
If the indicators exceed the specified values, this is a reason to be wary. Depending on where exactly the excess of leukocytes is diagnosed, the final diagnosis is made. For example, if the urethra is affected, urethritis may be diagnosed.
With prostatitis, an excess of leukocytes will be detected in the prostate secretion, which is also important for making such a diagnosis.

Reasons why mucus can combine with white blood cells
If there is a lot of mucus in the smear, and this is combined with leukocytosis, then the doctor will diagnose inflammation regardless of the patient’s gender.
Read also: Characteristics of the main sexually transmitted diseases
The symptom can be detected in both men and women. Moreover, as doctors note, inflammation is just a symptom, and not a full-fledged diagnosis.
When determining it, it is imperative to establish what the specific cause of the pathology is. Most often, the cause of the inflammatory process is microorganisms. They are classified by doctors as pathogenic and opportunistic. The differences between them are quite significant.
Pathogenic microorganisms always lead to the development of some disease. Normally, they are completely absent in the human body, even in minimal concentrations. Examples of such microorganisms are gonococci, chlamydia, and trichomonas.
Opportunistic microorganisms can live in the human body for a long time. However, they do not cause discomfort to the patient until there are only a few of them. If active reproduction begins, unpleasant symptoms of the disease appear, complicating a person’s life. Examples of opportunistic microorganisms are mycoplasma, ureaplasma, and candida.
To establish the cause of the disease, it is not enough to simply evaluate a smear using a microscope.
The use of additional techniques is often required.

For example, a smear can be sown on nutrient media for further evaluation, or subjected to PCR diagnostics.
The doctor selects any methods for correcting the condition only when the origin of the disease is clear. Until the source of the inflammatory process is diagnosed, no therapy is prescribed to the patient. Since it is likely to do more harm than good.
Urethral smear in the diagnosis of STIs
The procedure for preparing the drug involves applying the discharge obtained from the surface of the urethral mucosa onto a glass slide. For a more detailed examination under a microscope, the smear can be stained with special dyes.
- 1As a rule, the collection of material for a smear is carried out in a standing position, with underwear lowered.
- 2Using a napkin, mucus is removed from the external opening of the urethra; a special brush and probe are inserted into the opening to scrape off the mucous membrane.
- 3If there is no discharge, the patient is asked to massage the urethra from the base of the penis to the glans.
- 4The brush is inserted 2 cm deep into the urethra. You should not perform rotating movements with the probe, as this manipulation is accompanied by severe pain.
- 5The resulting material is applied to glass slides and labeled.
- 6To identify motile trichomonas, a native preparation is prepared: saline solution (37°C) is added to the material applied to the glass slide. This method is applicable if a man has copious discharge from the urethra.
- 7For subsequent microscopy in the laboratory, slides must be air dried and labeled. During a delayed study, the obtained biomaterial can be fixed on glass.
| Pathogens |
| Chlamydia trachomatis |
| Mycoplasma hominis |
| Mycoplasma genitalium |
| Ureaplasma urealyticum, Ureaplasma parvum |
| Neisseria gonorrhoae |
| Trichomonas vaginalis |
| Gardnerella vaginalis |
| Candida albicans |
| Human herpes virus types 1 and 2 |
| Human papillomaviruses, highly oncogenic (16,18, etc.) and low-oncogenic (6,11, etc.) |
7.1. Gonorrhea
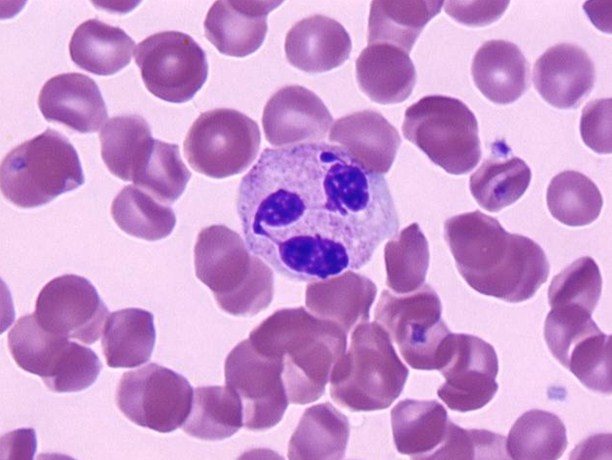
The causative agents of gonorrhea are Neisseria gonorrhoeae (Neisser's gonococci), bean-shaped cocci, located in pairs, with concave sides facing each other.
Gonococci are detected when:
- Microscopy of a stained specimen (Gram stain, methylene blue stain). The result can be positive (detected) or negative (not detected).
- PCR. The PCR result can be positive or negative.
- Bakposeve (sowing on chocolate agar). The method is used to make a diagnosis in children, regardless of microscopy results, when gram-negative diplococci are detected in a smear and there are no clinical manifestations.
Gonococcal urethritis is confirmed by the following results:
- 1 Absence/decrease in the level of normal microflora.
- 2Increased number of polymorphonuclear, not destroyed leukocytes (more than 4-5).
- 3Identification of intracellular diplococci (located inside phagocytes).
- 4Identification of extracellular diplococci.
7.2. Trichomoniasis
The causative agent is Trichomonas vaginalis, a protozoan. To detect trichomonas, it is necessary to examine freshly collected material from the urethra.
To confirm trichomoniasis in men, the following are used:
- 1Microscopy (method of “crushed” or “hanging” drop, staining of the preparation according to Leffler, Gram, Romanovsky-Giemsa). In the pathological material, living, mobile Trichomonas are determined (pear-shaped, oval shape, jerky, rotational movements of the microorganism).
- 2PCR – diagnostics.
- 3Cultural method (seeding on a nutrient medium). In men, due to the small number of trichomonas in the discharge, it is advisable to use the cultural method.
7.3. Chlamydia
Chlamydia trachomatis is difficult to see with a regular microscope, so the material obtained by scraping from the urethra is examined by PCR. The information content and reliability of such an analysis with proper preparation (see above) is very high.
With chlamydia and chlamydial urethritis, the following results are possible:
- 1When examining a simple smear through a microscope, an increase in the number of leukocytes is revealed (4 or more in the field of view).
- 2The number of epithelial cells may be increased or within normal limits.
- 3PCR revealed chlamydia trachomatis DNA.
Testing for genital herpes is carried out in a specialized laboratory. Microscopy using conventional staining methods is not applicable due to low sensitivity and specificity. The main diagnostic methods are immunoluminescence (RIF), molecular genetic (PCR) methods.
In laboratory diagnosis of HPV, exclusively molecular biological methods (PCR) are used. Microscopy of Papanicolaou-stained specimens is characterized by low sensitivity.
Characteristic cytological signs of HPV: the presence of koilocytes (cells with heterogeneous hyperchromatic nuclei, a lighter rim of cytoplasm is determined perinuclearly), loss of nuclei. The described morphological changes in cells must be confirmed by molecular biological methods (PCR).
Mucus in a smear: detection of bacteria
Mucus in a smear means that in the fair sex it is not always an infectious process or the norm. It can also be a symptom of dysbiosis. In the event that its excess is detected, but there is no inflammatory process, leukocytosis is not detected.
Normally, the genital tract is not a sterile area. They are inhabited by bacteria, most of which are lactobacilli. Under certain circumstances, the number of these bacilli may fall. This happens when immunity decreases or when antibiotics are used irrationally.
Other microorganisms take the place of lactobacilli. They may not provoke a strong immune reaction and may not accompany their reproduction with an inflammatory process. In this case, mucus will form in large quantities. There will be an unpleasant odor coming from the vagina. It can become a cause of complexes for the fair sex.

This condition is called vaginosis, since there is no inflammation in the organs. Normally, a large number of gram-positive rods will be detected in a vaginal smear. If there are fewer of them than required according to the norms, or they are absent altogether, the doctor concludes that the cleanliness of the vagina is impaired.
If a representative of the fair sex is diagnosed with vaginosis, then treatment is carried out under medical supervision, as is the case with STDs.
The means of therapy are selected individually in each case, and the treatment itself often takes place in two stages.
How to decipher the results?
3.1. Normal flora
Recently, special attention has been paid to the normal composition of the vaginal microflora, since it has been proven that it is this factor that determines a woman’s reproductive health, provides local immunity, protection from pathogenic bacteria, and the normal onset and course of pregnancy.
Normally, 95% of a woman’s flora consists of lactic acid bacteria (otherwise known as Doderlein bacilli, lactobacilli, lactobacilli).
During their life, lactobacilli process glycogen released from epithelial cells to form lactic acid. It is this that provides the acidic environment of the vaginal contents, which prevents the proliferation of facultative and pathogenic flora.
Each woman has 1-4 types of lactobacilli in her vagina, and their combination is purely individual.
When deciphering the results of the analysis, it is impossible to conduct a detailed analysis of the vaginal microflora; the laboratory assistant evaluates only the ratio of rods and cocci.
The absence of cocci and a large amount of gram-positive rod flora (++++) is equated to grade 1 vaginal cleanliness. This is observed quite rarely; this situation is more typical for control smears after vaginal sanitation or taking antibiotics.
A small number of cocci (+, ++) is considered normal and indicates 2 degrees of purity, but only if rod flora (++, +++) is also detected. This is a good stroke.
An increase in the number of cocci (+++, ++++) against the background of a decrease in the number of rods (+, ++) is considered pathological. This result is called grade 3 vaginal cleanliness. This situation requires a detailed examination .
A large number of cocci (++++) and the complete absence of gram-positive rods (Gram + rods) in the smear indicate 4 degrees of purity. In this case, the woman requires mandatory treatment.
You can read more about the degrees of vaginal cleanliness here (follow the internal link).
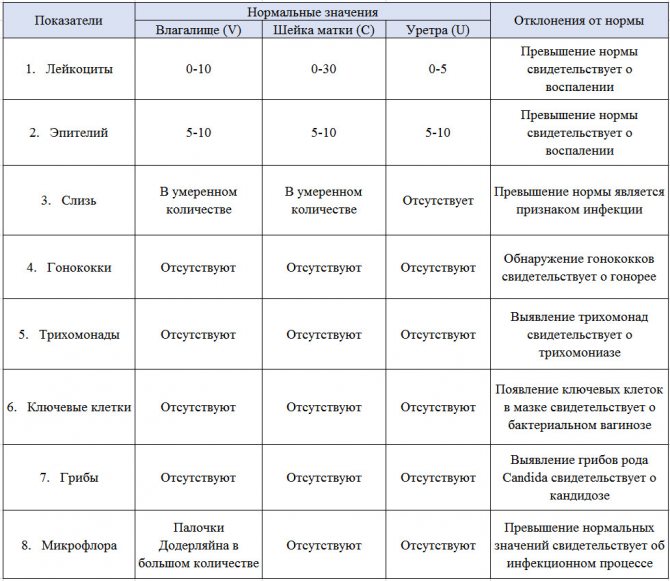
Table 1 - Normal indicators assessed when interpreting the results of smear microscopy for flora and GN. To view, click on the table
3.2. Gonococci and Trichomonas (Gn, Tr)
Gonococci are bean-shaped microorganisms that are the causative agents of gonorrhea. They are unstable in the external environment, but when they enter the human body they are surrounded by a special capsule.
The main reason for the referral of patients with gonorrhea is purulent, profuse discharge from the genital tract. Pain during urination and discomfort in the genitals occur in only 50% of women. A latent course of infection with a tendency to chronicity and the development of secondary infertility is often observed.
Normally, gonococci are absent in a smear for microflora and GN. They are detected when gonorrhea is 100% present, which requires immediate treatment not only for the woman, but also for all her sexual partners.
It is also necessary to additionally examine all family members, especially children, since infection can be transmitted through shared towels, bathrooms, and personal items.
Trichomonas vaginalis are unicellular (protozoan) microorganisms capable of movement due to flagella and independent life outside the macroorganism.
In vaginal contents, it is possible to detect Trichomonas vaginalis, which is the cause of urogenital trichomoniasis. The predominant mode of transmission of urogenital trichomoniasis is sexual.
Once on the vaginal mucosa, Trichomonas firmly attach to the surface of the epithelium and cause cell death.
In response to the influence of pathogens, inflammation develops on the mucous membrane: hyperemia (redness) and swelling, petechiae (pinpoint hemorrhages), local hyperthermia (increased temperature) appear.
Normally, there should be no trichomonas in the vaginal smear for purity. If they are detected, specific treatment of the woman and her partner is necessary, as well as additional examination of family members living in the same area (contact household transmission of the infection cannot be ruled out).
3.3. Leukocytes
Leukocytes are blood cells, the so-called white blood cells, the main function of which is specific and nonspecific defense of the body. Leukocytes are divided into several types depending on the function they perform in relation to foreign agents: some recognize them, others deliver them, and others destroy them.
When microscopying a vaginal smear, it is not the type of leukocytes that is taken into account, but their total number. An increase in the number of leukocytes in a smear indicates the presence of an inflammatory process.
The norm for leukocytes is considered to be up to 10 in the field of view in a non-pregnant woman for vaginal discharge.
During pregnancy, up to 20 leukocytes per field of view are considered normal, which is associated with the physiological state of immunosuppression and increased load on the excretory system.
In the discharge taken from the vaginal part of the cervix, a higher level of leukocytes is acceptable - up to 30 in the field of view. In a normal urethral smear, the number of leukocytes does not exceed 0-5 in the field of view.
Exceeding normal values (“bad smear”) may be a sign of:
- 1Inflammatory process at any level of the reproductive system: colpitis, cervicitis, endometritis, salpingoophoritis.
- 2Latent or chronic infection (ureaplasmosis, chlamydia, mycoplasmosis), the presence of STIs that need to be treated.
3.4. Epithelial cells
During the reproductive period of a woman, provided that normal hormonal levels are maintained, the surface cells of the vaginal mucosa are regularly exfoliated and rejected, thereby maintaining the healthy state of not only the mucous membrane itself, but also the constancy of the vaginal environment.
However, during microscopy of a gynecological smear, the number of epithelial cells in the field of view is always assessed. Normally, their number does not exceed 10 in the field of view of the laboratory technician.
A decrease in their number may indicate:
- 1About hormonal imbalance: decreased estrogen saturation of the body (hypoestrogenism), increased androgen levels.
- 2Atrophic colpitis.
Exceeding the norm is a sign of:
- 1Inflammatory process in the reproductive system: colpitis, cervicitis, endometritis, salpingoophoritis. By intensifying the rejection of the epithelium, the mucous membrane “tries” to prevent the proliferation of pathogenic flora.
- 2 Sexually transmitted infections.
- 3Bacterial vaginosis.
- 4 Hormonal imbalance.
3.5. Slime
Mucus is also a normal part of vaginal discharge and is part of the secretion of the glands.
If mucus in the analyzed smear is detected in a small (+) or moderate (++) amount, then this is interpreted as normal.
There must be no mucus in the material taken from the urethra. If its volume is significant, one should suspect the presence of an inflammatory process (usually colpitis or cervicitis) and hormonal imbalance.
3.6. Key cells
The key cells are the cells of the desquamated vaginal epithelium, along the edge of which many gram-variable bacteria, thin rods and cocci are attached. Under microscopy, they give the cell an uneven, granular appearance.
Normally, they should not be present in a woman’s vaginal discharge. Their presence is a specific marker of vaginal dysbiosis – bacterial vaginosis.
Mucus in a smear in men
Mucus may also be present in a smear in men. Its presence is normal if biological material for evaluation is taken from the urethral area. In this case, as in the case of women, the amount of discharge plays a role.
If there are more than two pluses on the form, then you should be wary. The presence of excess mucus in a man’s body is assessed only in conjunction with additional indications. Without them, it is impossible to draw conclusions about the presence or absence of any disease.
Take into account:
- the presence of an excess number of leukocytes in the results
- the presence of epithelial cells in large numbers, which indicates tissue death
- presence of clearly pathogenic microorganisms
- excess of bacteria belonging to the class of opportunistic pathogens (meaning an excess of certain titers, which are determined for each type of bacteria individually)
It is also important to remember that in the stronger sex, excess mucus can be explained not only by infections.
The culprit for the appearance of a symptom in the test results may be prostatitis. With this disease, mucous components are also produced in excess. This leads to an increase in the mucus indicator in the study results. The disease can be combined with urethritis, which only makes the indicator even more pronounced.
Read also: Genital warts
When to see a doctor
If a woman discovers uncharacteristic vaginal discharge, feels pain in the lower abdomen, discomfort during intimacy, the menstrual cycle is disrupted, and other signs of inflammation appear, then this is a reason to consult a gynecologist.

The doctor will perform a general examination of the genital organs, conduct a diagnostic examination and select smears for further microbiological examination.
Men who feel a prolonged burning sensation during urination, find unusual discharge from the urethra, pain in the perineum, various types of erectile and sexual disorders, should seek medical help from a urologist.
A visit to specialized specialists should take place in the first 1-2 days after the onset of pathological symptoms. The average cost of an examination is 2100-2800 rubles.
Mucus in the smear and cystitis
Patients often forget that the urethra is in close connection not only with the genitals.
Moreover, many patients tend to believe that only the genitals can be a source of mucus. Although in fact this opinion is incorrect.
The main job of the urethra is to remove fluid from the body in the form of urine. This means that the urethral tract is connected not only with the genitals, but also with the organs of the urinary system, such as the bladder and kidneys. In this regard, mucus in a urethral smear can indicate not only damage to the genital tract. Often it indicates involvement of the bladder, kidneys, and ureters in the pathological process.
The most common inflammation of the bladder in practice is cystitis. Most often, cystitis occurs in the fair sex. This is due to the structural features of their genitourinary system. Pathology can be caused by E. coli and other pathogens.
For men, cystitis is an uncharacteristic disease, but it should not be ruled out.
Yes, it is less common in the practice of urologists, but the likelihood of encountering it remains.
Causes of bacteria and mucus
The reasons for the presence of bacteria and mucus in the smear are infection of the body in various ways.
Bacteria cause inflammatory reactions in the affected organs of the genitourinary system and contribute to the appearance of infected mucus.
The causes of infection can be very different.
The bacteria may be coccal or another form.
Cocci come in gram-positive and gram-negative forms.
We talk about gram-positive cocci when we talk about lactobacilli, enterococci, staphylococci and streptococci.
Gram-negative cocci include gonococci, Proteus and Escherichia coli.

If gram-negative cocci are found intracellularly, then most likely we are talking about gonococci.
When very small sticks are found in the mucus, we talk about Gardnerella.
Are infections always to blame when there is mucus in a smear?
Mucus in a smear is not always a sign of an inflammatory process of infectious origin.
Many patients forget about this, causing panic when receiving test results. In fact, the indicator can be observed in other conditions of the body.
For example, this happens if:
- woman is pregnant
- a representative of the fair sex was tested on the eve of ovulation or during it
- on the eve of the study there was an episode of active sexual contact (because of this, it is also recommended to limit sexual activity during preparation)
A number of therapeutic and diagnostic interventions can provoke pronounced deviations from normal indicators. In this case, its appearance is explained quite simply: the urethra is irritated, which triggers the mechanisms of excretion production.
Cystoscopy, or taking a smear from the urethra in men, is a common cause of increased rates. We must not forget about non-inflammatory diseases that provoke changes in tests.
With urolithiasis or sand in the kidneys, the indicator may increase.
It often changes with oncological pathologies of the urinary system.
Mucus in a flora smear always requires careful assessment in combination with other indicators.
In no case should a patient be diagnosed solely on the basis that the examination results show an increased amount of this element! Naturally, the patient himself should not engage in self-diagnosis. He should seek help from a doctor.
Collection of material for research
Taking a gynecological smear is possible from three points: the urethra (if necessary), the posterolateral vaginal vault and the vaginal part of the cervix.
The material for analysis is vaginal discharge, discharge from the cervical canal, discharge from the urethra (according to indications).
Vaginal discharge is multicomponent, it includes:
- 1Mucus of the cervical canal - needed for the penetration of sperm into the uterine cavity and higher for fertilization. Its thickness depends on the level of estrogen in a woman’s body; its viscousness can be used to judge the phase of the menstrual cycle.
- 2 Secretion of the glands of the external genitalia.
- 3Desquamated vaginal epithelium.
- 4Bacteria (vaginal flora). Normally, the microflora in the smear is represented by a large number of lactic acid bacteria (Gram-positive Doderlein bacilli) and a small amount of opportunistic flora (most often coccal).
2.1. Preparing for a smear collection
Before collecting material, a woman must meet certain conditions:
- 1It is better to take the test on days 5-7 of the menstrual cycle. During menstruation, discharge is not collected.
- 2 Avoid the use of vaginal suppositories, lubricants, douching and sexual intercourse 24 hours before the test.
- 3Before taking a smear, you do not need to use scented intimate hygiene products; it is better to toilet the external genitalia with running water.
- 4It is not advisable to take a hot bath on the day of the test.
2.2. Technique for obtaining material
- A smear on the flora is taken strictly before a bimanual examination, the woman is on a gynecological chair.
- A Cusco-type bicuspid speculum is inserted into the vagina, and the vaginal part of the cervix is exposed (exposed).
- Focusing on it, the doctor uses a special spatula to collect material from the posterolateral vaginal vault and transfers it to a glass slide, which, after filling out the directions, is delivered to the laboratory for microscopic examination.
- Analysis from the external opening of the urethra is taken with a bacteriological loop or a Volkmann spoon. If there are purulent discharges, it is advisable to take them by lightly pressing on the external opening from the outside.
- Analysis is taken from the surface of the vaginal part of the cervix with an Erb spatula.