Colposcopy (Ancient Greek: κόλπος, translit. Kolpos, lit. "void, uterus, vagina" + skopos "to look") is a medical diagnostic procedure for examining the cervix and vaginal tissue. Many precancerous lesions and malignant lesions in these areas have noticeable characteristics that can be detected during examination. The examination is carried out using a colposcope - a special device that provides an increased field of view of the areas being examined, allowing the colposcope to visually distinguish normal from abnormal tissue that appears and perform a biopsy for further pathological examination. A colposcope is an illuminated binocular microscope connected to a video monitor that magnifies the area of interest 6 to 40 times its normal size. The main purpose of colposcopy is to prevent cervical cancer by early detection of precancerous lesions and treatment of them.
Historical facts
In 1924, Hinselmann was asked to write a chapter based on the etiology, symptoms and diagnosis of uterine cancer in the third edition of the Handbook of Gynecology. Hinselmann faced this challenge most successfully. He performed gynecological examinations and often encountered early detection of cervical cancer, which he believed could only be improved by optical means. He believed it was necessary to "provide an intense light source for the magnified image without sacrificing binocular vision."
Content:
- Historical facts
- Composition of a colposcope
- Indications for the use of colposcopy
- Differences between simple and extended colposcopy
- Preparing for the examination
- Methodology
- Complications after extended colposcopy
- Contraindications for the study
- Colposcopy and pregnancy
- Study protocol
By 1925, he reported the construction of the first colposcope. To this end, he connected a light source to Lake's binocular biological microscope. He connected the optical system to a stand that allowed movement in each direction and also supported a small screw for fine adjustment. After the invention of the colposcope, Hinselmann was able to state that “with regard to so-called early problems, colposcopy makes it possible to detect earlier cases.” Even a tiny tumor the size of a dot did not disappear and was visible even with an initial magnification of 7.5 times. Thus, Hinselmann discovered a completely new invention and proved its significance in the field of medicine.
Composition of a colposcope
Colposcopes come in two types: those with a fixed focal length lens whose magnification can be changed by changing the power of the eyepieces, and those with a fixed focal length lens but with multiple magnifications where the dial setting can be changed or a button pressed. .
Increase

Multiple magnifications are preferred, starting at ×5 or ×7.5, ×20 or ×30. The lowest magnification gives a bird's eye view and is great for locating or zooming in on an area of interest. The magnification commonly used for detailed examination is ×15. The modern colposcope is based on the original prototype, but differs from the original in that the magnification varies from 6 to 40 times, as opposed to the original 7.5 times. 10x magnification is suitable for everyday use. Higher magnification allows you to recognize some minor points, but it is not necessary to use it for an accurate diagnosis.
The most important accessories for a colposcope are photographic equipment and special spare parts for teaching. Also, simple low-power devices without any accessories are always available on the market, as well as more complex ones with electrical control, a zoom lens with fine tuning and a camera. For routine use, a simple colposcope is fine, but for training, both the camera and viewing tube are essential. All colposcopes have lenses, eyepieces, filters, a light source and a stand.
Lens
This in turn affects the focal length and therefore the working distance. The best focal length is between 250mm and 300mm. This allows you to easily operate and manipulate tools without interfering with your vision.
Eyepieces
Eyepieces must have the following good characteristics: the axes of the eyepieces can be straight or inclined at an angle of 45° to the optical axis of the device, they must have rubber cups installed on them, they must have independent focusing elements that adapt to human vision. Also one very important feature is the convergent line of sight for fatigue-free working.
Filters

Most colposcopes are equipped with green filters. They absorb red light and enhance the image of blood vessels that appear black. The contrast between normal and abnormal epithelium is also enhanced.
Light source
The light source must be at least 30,000 lux, must be constantly centered, and must have a rheostat to vary the light intensity. Some equipment has automatic brightness adjustment depending on the magnification used. Most colposcopes are equipped with a halogen lamp with a power of 6 to 12 W and 20 to 75 W. A recent innovation is the light emitting diode (LED), which is a better light source. They generate light through semiconductor processes rather than heating a wire filament, as in a halogen lamp. The advantages of an LED light source are that its light output is five to seven times higher than that of a lamp; this light uses a different optical system, significantly improving contrast, and with it overall visibility improves. The service life of an LED is also many times higher (up to 10,000 hours) than a halogen lamp. It lasts for approximately 10 years with daily use of approximately 4 hours.
Indications for the use of colposcopy
The main purpose of colposcopy is to detect intraepithelial neoplasia and early neoplasia of the cervix, vagina and vulva.
Colposcopy is used for the following purposes:
- is an integral part of every gynecological examination in combination with cytology;
- used to display the location of lesions;
- to clarify the nature of clinically suspicious pathologies;
- used as part of a forensic sexual assault investigation;
- for diagnosing diseases caused by human papillomavirus infection;
- for changes associated with immunosuppression, such as human immunodeficiency virus (HIV) or a transplant patient.

Indications for the mandatory use of extended colposcopy are:
- presence of condylomas of the vagina and vulva during examination;
- pathological changes according to the results of a cytological smear;
- pathological conditions visible on the cervical mucosa;
- preoperative periods and before cervical biopsy;
- routine examinations after treatment of cervical diseases.
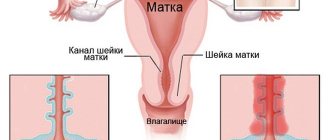
This manipulation allows the gynecologist to diagnose pathological processes such as cervicitis - inflammation of the cervix, the presence of condylomas, papillomas, polyps, genital warts, erosion, dysplasia, cervical and vulvar cancer, leukoplakia, erythroplakia, possible progression of precancerous and cancerous changes.
Is cervical cancer visible on colposcopy?
The results of cervical colposcopy obtained during the examination are the most accurate source of information about the likely presence of cancer cells, but more often doctors are able to identify a precancerous condition, which is known as cervical dysplasia.
Doctors tend to classify any accumulation of abnormal cells that indicate dysplasia as potential cervical cancer (abbreviated cervical cancer):
- delicate mosaic with blurry edges;
- moderate mosaic and punctation;
- pronounced mosaic of the cervical mucosa with changes in the nuclear structure of cells;
- altered vascular pattern - atypical curls, thickened capillary network.
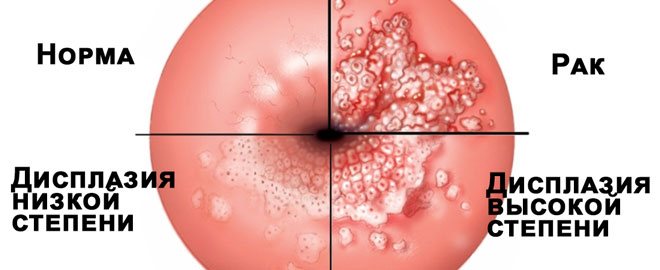
Such changes are not yet cervical cancer, but the condition requires close monitoring. To timely monitor the progression of the pathology, the doctor will need the results of colposcopy more often: up to 2-4 times a year, depending on the area of the abnormal zones.
Important! As a rule, for cervical cancer, the colposcopy transcript contains information about the presence of necrotic foci, ulcers and bleeding vessels.
Despite the presence of the signs described above in the diagnostic transcript, it cannot be said that they showed oncology. The final result will be known after the histology and cytology interpretation is received.
Differences between simple and extended colposcopy
An extended examination of the cervix and vagina differs from a simple procedure by using certain other drugs and medical tests. During an extended study, doctors most often use:
- Three percent acetic acid. This acid has the property of constricting intact blood vessels, so all doctors must use it. The acid causes short-term swelling of the epithelium, the blood supply to the mucous membrane decreases, the cells of the spinous layer swell and the subepithelial vessels contract. This allows you to accurately determine the presence of pathological conditions, types of epithelium (stratified squamous, cylindrical), and assess the condition of blood vessels (typical and atypical).
- Schiller's test. This is a test with Lugol's solution, which contains iodine. Its property is the release of glycogen into the epithelium, coloring the healthy mucosa dark brown. If the cells of the stratified squamous or columnar epithelium are pathological, then this area will not be stained. It will look like whitish spots on a dark background.
- Chrobak's test. A method by which a doctor can recognize cancer of the vaginal part of the cervix. It is carried out by applying light pressure with a thin probe to suspicious areas of the mucous membrane. The appearance of bloody fluid is considered a sign of cancer.
- Color colposcopy – chromocolposcopy. Gynecologists perform this procedure much less frequently. It is carried out by applying special solutions that stain the stratified squamous epithelium in blue shades, without staining the columnar epithelium. For example, these are solutions of hematoxylin, toluidine blue, gentian violet, and methyl violet.

A simple colposcopy can be said to be a preliminary manipulation before an extended examination. The cervix is opened with a vaginal speculum, any discharge on the surface is removed with tampons, and then the doctor examines the vaginal part of the cervix using a colposcope.
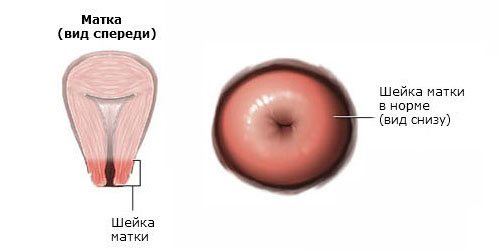
Normal results: what a healthy cervix should look like
The preliminary results of colposcopy become known to the doctor from the first seconds of examination of the vagina. The following visual signs support the norm:
- pale pink or slightly bluish color of the outer layer with a uniform, slightly shiny structure;
- the rounded shape of the pharynx of the cervical canal in nulliparous girls and flat, slit-like in those who have given birth;
- a cylindrical epithelium separated by a clear line in the pharynx of the cervical canal and flat epithelium on its part facing the vagina - the transition zone;
- There is no inflammation (colpitis) - there are no hyperemic or swollen areas.
All these indicators are recorded as the norm before using a solution of vinegar, Lugol and other chemical reagents, with the help of which metaplasia is detected.
In the absence of pathologies, uniform staining occurs under the influence of reagents:
- under the influence of vinegar, healthy mucous membranes turn pale, and after a few seconds they become pink or bluish again;
- under the influence of iodine and Lugol, the neck is evenly colored brown;
- under the influence of adrenaline, the tissues evenly lighten, and then they return to their normal appearance.
Important! If there is a normal reaction of the mucous membranes, the interpretation of the results contains o or “negative”.
Methodology
When the patient initially visits her gynecologist, the doctor collects anamnesis, namely the number of previous pregnancies and births, the course of pregnancy, previous illnesses, information about the menstrual cycle, the use of contraceptives, previous smear results, the presence of allergic reactions, medications taken, whether harmful habits and other related issues.
A colposcope is used to identify visible signs indicating abnormal tissue. It works as an illuminated binocular or monocular microscope to magnify the view of the cervix, especially the vaginal part and the vagina in general. Low magnification (2 × 6 ×) can be used to obtain a general view of the mucosal surface. Magnification from 8x to 25x is already used for a full assessment of the vagina and cervix. High magnification coupled with a green filter is often used to identify certain vascular structures that may indicate the presence of more complex precancerous or cancerous lesions. Acetic acid solution and iodine solution are applied to the surface to improve visualization of abnormal areas.
Colposcopy is performed by a woman lying on her back on a gynecological chair. A Simon or Cusco speculum is placed in the vagina and the doctor performs a gynecological examination. Then, twenty centimeters from the area being examined, the doctor installs the colposcope and adjusts its clarity. The cervix is now illuminated by a bright beam of light. A simple colposcopy is performed, and then an extended one. Three percent acetic acid is applied to the cervix using cotton swabs. Areas of acetate are correlated with higher density. The “transformation zone” is a critical area on the cervix where precancerous and cancerous lesions most often occur. Areas of the cervix that turn white after acetic acid is applied or have an abnormal vascular pattern are often taken for biopsy. If no lesions are still visible, iodine may be applied to the cervix to help highlight abnormal areas.
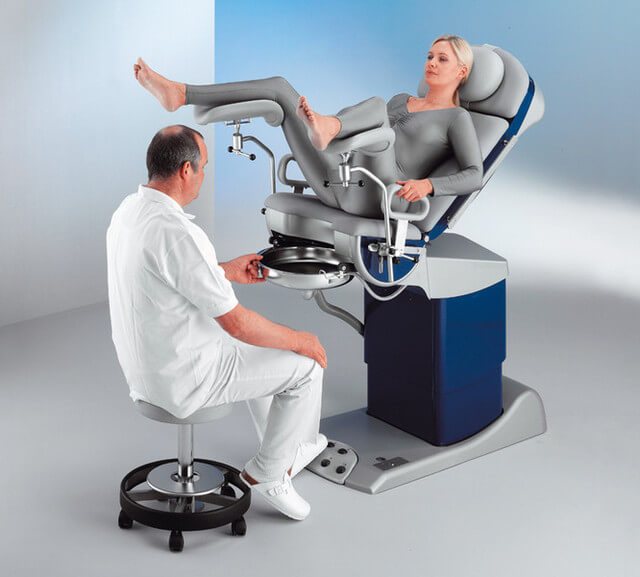
After a complete examination, the gynecologist identifies the areas with the highest degree of visible pathology and decides whether a biopsy is necessary. Most doctors and patients consider anesthesia for biopsies unnecessary, however some now recommend and use a local anesthetic such as lidocaine to reduce patient discomfort, especially if multiple samples are taken. The procedure without a biopsy takes a maximum of thirty minutes.
Complications after extended colposcopy
Colposcopy is a fairly safe diagnostic method that rarely gives complications; if they happen in very rare cases, they are not of a general nature. They may include bleeding from the genital tract during the first three to five days of a dark brown color, the color of Lugol's solution, an increase in body temperature to low-grade levels, and increased menstruation. Rarely, there are cases of infection on the biopsy site or on the endometrium after manipulation some time later.
If a biopsy was performed, then for two to three days there may be slight discomfort in the lower abdomen, which is not a reason to panic.
What to expect after colposcopy
| After a simple colposcopy | After extended colposcopy | After cervical colposcopy with biopsy |
| There are no restrictions on the patient’s usual lifestyle. There may be mild discomfort associated with the insertion of vaginal speculum. All sensations go away after a couple of days, as after a regular gynecological examination. | After an extended procedure, vaginal discharge may appear due to the use of reagents. The color depends on the technique and the reagent used. When using Lugol and iodine, the discharge may have a brown tint. If probes were used, the discharge will be mixed with blood. A woman’s activity will not decrease and will not require restrictions if a biopsy is not taken during colposcopy. Light discharge for 3 days is considered normal. If they intensify, itching or pain appears, or something bothers you for more than 3 days, you need to urgently consult a gynecologist. | During a biopsy, you need to abstain for about a week from:
You should consult a doctor immediately if:
|
Colposcopy and pregnancy
The study is done in pregnant women to determine whether invasive cervical cancer exists. Because the procedure is more difficult in a pregnant woman due to several factors such as increased mucus and uterine production.
If the initial test is inconclusive, the test should be repeated every six to twelve weeks or after 20 weeks. Because the pregnant cervix tends to bleed excessively, a biopsy is usually avoided for fear of harming the unborn baby. Typically, a biopsy is performed on a pregnant woman if all evidence indicates a huge risk of developing cancer or dysplasia. A colposcopy done correctly will never harm the patient if she is pregnant, and it will not harm her fetus in any way.
Study protocol
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Each woman who has undergone this diagnostic method is given a protocol with the results of the examination. It must be completed by the doctor who examined the patient. The results sheet includes the following items: type of cervix (cylindrical, conical, hypertrophied, deformed), type of external uterine pharynx (round, slit-like, semilunar), rupture (yes, no, post-traumatic deformation), ectropion (yes, no), ectopia columnar epithelium (yes, no). Normal transformation zone: open glands or closed (Nabothian cysts), keratinized glands. Atypical transformation zone: acetate, iodine-negative epithelium, punctation (pinpointing - tender, rough), mosaic - tender, rough. Presence of vessels (yes, no, regular type, strengthening, atypical), leukoplakia (yes, no), cervical relief (smooth, uneven, raised), presence of scar changes, coagulated cervical syndrome, endometriosis, polyps, exophytic condylomas, inflammation (diffuse and local), atrophy, ulcers (true erosions), pinpoint ulcerations.
Normal cervical mucosa
The mucous membrane of the vaginal part of the cervix is covered with stratified squamous epithelium; upon examination, it has a pale pink color and shines. It has a cyanotic tint in the second half of the menstrual cycle in women. The pattern of vessels is of the correct type, evenly spaced, the relief of the cervix is even. Any other pathologies are a signal for further research and treatment.
It can be concluded that this research technique is absolutely safe and painless, it allows you to carry out both diagnostic and therapeutic measures, for example, it can be used to remove polyps and condylomas, and perform a biopsy of a suspicious area. The study allows us to identify inflammatory diseases, carry out differential diagnostics, and identify serious pathologies in the early stages with the possibility of early treatment.
More fresh and relevant information about health on our Telegram channel. Subscribe: https://t.me/foodandhealthru
We will be grateful if you use the buttons:
Colposcopy: what is this procedure?
This is a diagnostic method for examining the vulva, vagina, and mucous membrane of the cervix. To carry out the procedure, a special optical device, a colposcope, is used, which gives the doctor the opportunity to conduct an examination under magnification.
colposcopy prescribed and who needs it?
? Briefly, we can say that this procedure is prescribed by a gynecologist, and it is performed both on healthy women and those who have complaints. This is done in order to establish whether there are any pathological changes in the cervix, and if so, what is the nature and intensity of the changes.
How is the procedure carried out?
The patient is examined by a gynecologist using a special device called a colposcope, which has a built-in backlight and lenses that allow you to magnify the image 15–40 times.
Colposcopy precedes other procedures that were planned by the doctor for the patient. Before the procedure, all discharge must be removed from the surface of the cervix.
If necessary, if there is suspicion, the doctor can do a targeted biopsy of potentially dangerous areas. This is required to make an accurate diagnosis - to confirm or exclude the presence of pathologies.
Is it painful to have a colposcopy? No, the procedure is painless; slight discomfort may occur when taking material for a biopsy or when processing it with reagents.