A smear for ureaplasma in a woman, preparation for which requires compliance with certain rules, is an important point in the gynecological examination. Every representative of the fair sex is obliged to take care of her reproductive health and visit a gynecologist twice a year. Ureaplasmosis is a dangerous disease that is sexually transmitted. It needs to be identified as early as possible and treated appropriately. To get a reliable result, you need to properly prepare for the test.
Definition of research
A smear is a collection of cells from the mucous membrane of a certain organ for the purpose of diagnosing infectious diseases.
To study the collected material, various laboratory diagnostic methods are used, which make it possible to identify the causative agent of the infection:
- microscopy of bacteriological smear;
- PCR method;
- cultural sowing.
How long does it take to test for ureaplasmosis? The period required to obtain results depends on the research methodology. The fastest way is smear microscopy. However, its results are preliminary and are not used to make a final diagnosis. The choice of method for determining ureaplasma in a smear is made by a doctor depending on the clinical situation.
Bacteriological smear
A smear for ureaplasmosis is taken in the presence of an inflammatory process on the mucous membrane of the vagina or urethra. How is a smear taken? To do this, the gynecologist first inserts a speculum into the vagina. The manipulation itself is not painful, but causes the woman minor discomfort. During the procedure, the patient’s breathing should be calm and deep, and the vaginal muscles should not be strained. This will help reduce discomfort.
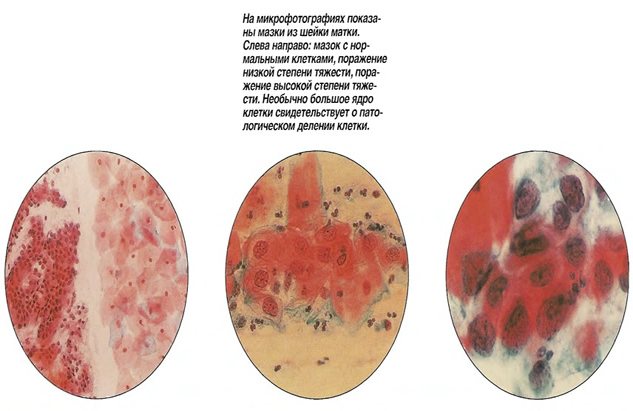
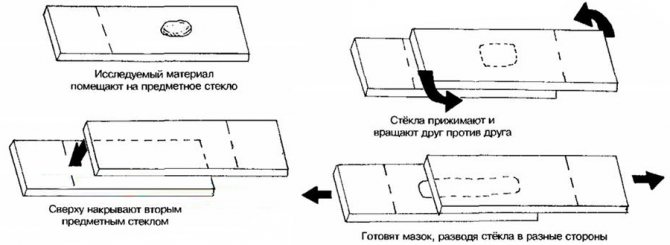
Where do they get the material for analysis? Using a sterile probe, a smear is made from 3 places: from the mucous membrane of the cervical canal of the cervix, vagina and urethra. The doctor applies the material taken in this way onto a glass slide. The smear is stained with a special paint and examined under a microscope. Each type of bacteria gets its own shade.
A bacteriological smear from a healthy patient reveals not only beneficial microorganisms, such as lactobacilli, but also a small amount of streptococci, staphylococci, and fungi. Such indicators are considered to be the norm. The presence of an infectious disease is indicated by a change in the composition of the vaginal microflora and the presence of inflammatory processes in the genital area.
What is ureaplasmosis
Ureaplasmosis is an excess titer of opportunistic bacteria - ureaplasma.
Normally, this titer should not exceed 10*4 CFU/ml. The microflora of a healthy person is dominated by lactobacilli, but in dysbiosis gardnerella, staphylococcus and ureaplasma may predominate. Symptoms of the disease are nonspecific and depend on the affected part of the genitourinary system.
Most often, the urethra or bladder becomes inflamed, which is manifested by painful sensations when urinating and the appearance of mucous discharge from the urethra. In this case, the pathological process can spread to other organs. An important caveat: urethritis and other pelvic inflammatory diseases (PID) can be caused by a variety of bacteria, but ureaplasmosis is diagnosed only if the inflammatory symptoms are caused specifically by Ureaplasma bacteria. Quote from the book by obstetrician-gynecologist Olga Belokon “I am a woman”
“Ureaplasma is not treated or detected. These are opportunistic pathogens that most women normally have in their vaginas. They do not affect pregnancy, do not lead to miscarriages, and do not cause infertility. Diseases need to be treated, such as bacterial vaginosis, as well as mycoplasma genitalium.”
Prevalence of the disease
Ureaplasmosis is dangerous for women primarily due to the development of urethritis, cervicitis, vaginitis and PID. According to statistics, inflammatory diseases of the pelvic organs are the reason for visiting antenatal clinics in 65% of cases. At the same time, patients with PID make up 30% of the total number of patients undergoing treatment in the hospital. The prevalence of salpingitis (inflammation of the fallopian tubes) and oophoritis (inflammation of the ovaries) in the Russian Federation is 1236 per 100,000 women.
In the United States, at least 1,000,000 cases of PID are reported every year. These diseases mainly affect women 17-28 years old who are sexually active and do not resort to barrier methods of contraception.
Pathogen
To date, microbiologists have identified 14 types of ureaplasma, but only Mycoplasma hominis, Ureaplasma urealyticum (T 960) and Ureaplasma parvum pose a potential threat to humans. It is these types of bacteria that can cause inflammatory diseases of the urethra and pelvic organs.
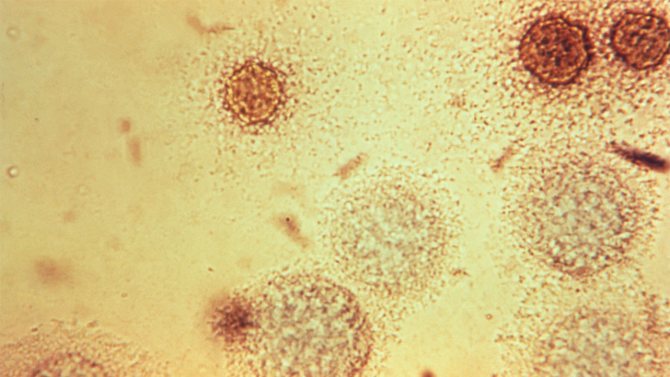
Bacteria Mycoplasma hominis. Photo: PHIL CDC
Mycoplasma genitalium deserves special mention - this microorganism is less common, but is highly pathogenic and resistant to many groups of antibiotics. It is transmitted predominantly through sexual contact, although infection cannot be ruled out through contact with the blood of a patient. Among mycoplasmas, only mycoplasma genitalium is recognized as the undisputed causative agent of STDs. Its detection is a diagnosis that requires treatment for both partners.
Ureaplasmas have an extremely unpleasant feature: being intracellular parasites, they penetrate the membranes of the cells of the genital organs, which significantly complicates the fight against them. The fact is that when the activity of foreign cells (antigens) is detected, our body forms a so-called immune response - it produces antibodies that destroy pathogenic agents. However, if these agents are securely hidden in the body’s cells, as ureaplasma does, the antibodies experience a kind of cognitive dissonance: it seems that the cells are their own, although they are somehow suspicious. To attack or not? Typically, antibodies choose the second option, which quite logically leads to an ineffective immune response.
The types of ureaplasma listed above are called opportunistic because they are part of the natural microflora of the genitourinary tract, and under normal circumstances they do not remind of themselves in any way. However, there are factors due to which ureaplasma is capable of creating a lot of trouble for its carrier (that is, a person). For example, if the ureaplasma titer exceeds the upper limit of normal (it is 10*4 CFU/ml), an inflammatory process may begin on the mucous membranes of the urogenital tract with all the ensuing consequences.
Conditional pathogens that live in the vagina of healthy women include:
- Mycoplasma hominis (mycoplasma hominis),
- Ureaplasma urealyticum (ureaplasma urealyticum),
- Ureaplasma parvum (ureaplasma parvum),
- gardnerella vaginalis,
- coli,
- leptothrix,
- staphylococci,
- streptococci,
- Enterococcus, Klebsiella.
Their detection in the body does not indicate illness. They should be treated only in the context of inflammatory diseases of the pelvic organs.
Contributing Factors
Additional factors also contribute to the development of inflammatory diseases against the background of ureaplasmosis:
- weakening of the immune system,
- frequent change of sexual partners, leading to disruption of the microflora of the genital organs,
- regular stress,
- bad habits,
- pregnancy,
- abortion,
- unprotected sex,
- taking hormonal drugs,
- a history of sexually transmitted diseases,
- douching,
- use of alkaline intimate hygiene products.
Many women are especially vulnerable to infection during pregnancy, since immune activity decreases significantly with the onset of pregnancy.
Transmission routes
The most common method of transmission of ureaplasma is sexual. The risk of infection exists even with oral-genital contact. Infection during childbirth from mother to child is also possible - in medicine this is called vertical transmission of infection. Experts regard the domestic route of transmission as unlikely, since ureaplasma is unstable in the external environment and quickly dies outside the cells of the host organism.
Forms of the disease
There are two main forms of ureaplasmosis:
- Spicy. It is relatively rare. With this form, the clinical picture can be traced quite clearly: pronounced symptoms of inflammation of the pelvic organs arise, which are often accompanied by symptoms of intoxication.
- Chronic. This form is much more common. Symptoms are mild and often completely absent. The chronic course is dangerous because the disease is more difficult to detect, and delayed treatment is always fraught with serious complications.
Complications
In most cases, diseases caused by ureaplasmosis are asymptomatic. This makes it impossible to start treatment on time and leads to complications. Inflammation due to ureaplasmosis in women can cause the following consequences:
- development of ascending PID (cervicitis - Fig. 1, salpingoophoritis),
- infertility - as a consequence of the diseases listed above,
- termination of pregnancy and congenital pathologies in the child,
- narrowing of the urethra as a result of the growth of scar tissue in its lumen (accompanied by a deterioration in the outflow of urine).
Figure 1. Inflammation of the cervix or cervicitis is one of the common diseases associated with ureaplasmosis. Typical symptoms of cervicitis include white, grayish, yellow or bloody vaginal discharge, pain during sex, pelvic pain, and pain when urinating. Source: Mayo Clinic
Danger during pregnancy
Due to PID caused by an increase in ureaplasma titer, premature birth, frozen pregnancy and spontaneous abortion are possible. The child also has a risk of congenital pathologies.
What will happen if left untreated?
If left untreated, ureaplasmosis can cause inflammatory processes in the uterus, fallopian tubes, and ovaries. The formation of scar tissue inside and outside the fallopian tubes, in turn, makes them obstructed and leads to infertility. Untreated inflammatory diseases can also cause ectopic pregnancy and chronic pain in the pelvis and abdomen. Finally, any genitourinary infection increases the risk of developing cervical cancer.
Preparation for a bacteriological smear
You can get tested for ureaplasma on the first day after the end of menstrual bleeding or a couple of days before it starts. When preparing for the study, the following recommendations should be followed:
within 2 days before taking a smear, you must abstain from sexual intercourse;- It is prohibited to douche with antiseptics and use local contraceptives on the eve of the examination;
- 7–10 days before the study, stop treatment with vaginal medications and antibiotics;
- on the eve of the test, intimate hygiene is carried out in the evening with warm water without soap;
- you need to refrain from urinating for 2–3 hours before submitting the material for research.
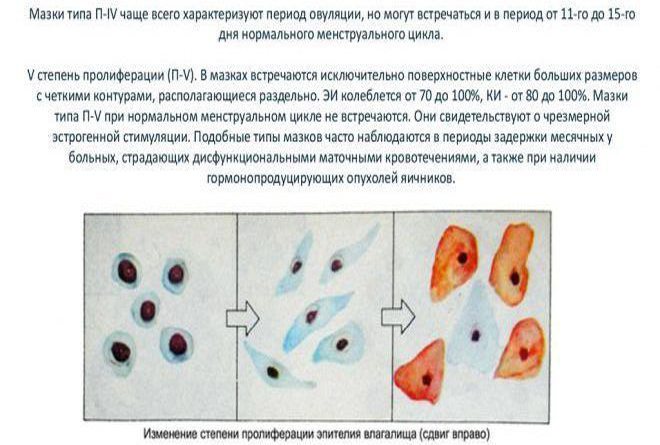
A smear examination takes 30–60 minutes. During such an analysis, foreign bacteria are detected, but it is impossible to determine their nature. The causative agents of ureaplasma are not visible under a microscope. A change in the composition of the vaginal flora indicates the presence of a sexually transmitted infection. In such a situation, the attending physician should order additional tests to confirm suspicions.
PCR method for detecting ureaplasmosis
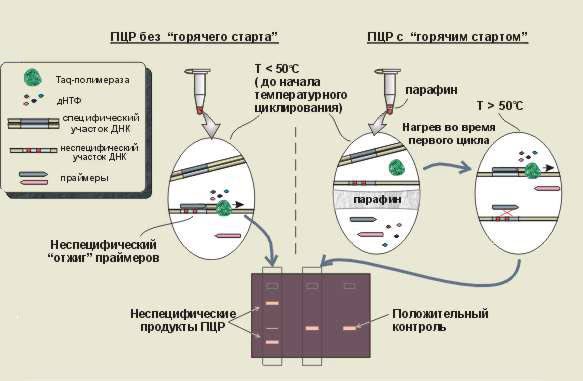
The polymerase chain reaction technique is one of the most informative and reliable in terms of detecting ureaplasma in the body. It allows you to detect microorganisms even in single numbers during the study of biomaterial. The modern method of laboratory diagnostics, PCR, is based on the determination and identification of the DNA of the pathogen.
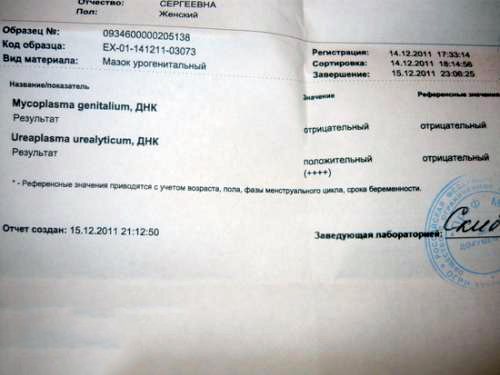
How to take a test to determine infection using polymerase chain reaction? The material for PCR research is taken from the uterine canal. The result of the study can be obtained within 5 hours. During the analysis, the presence of hidden forms of ureaplasma can be detected.
Treatment of ureaplasma
What to do if during a routine examination you were diagnosed with ureaplasma?
First of all, additional diagnostics are needed.
It is imperative to conduct research to identify concomitant infections: chlamydia, gonorrhea, trichomoniasis.
After this, both spouses are assigned a course:
- antibacterial therapy aimed at eliminating the pathogen
- enzymes for antibiotic delivery
- immune drugs
- local treatment (rinsing, baths)
Typically, ureaplasma responds well to complex treatment, and the duration of the therapeutic course is 15-20 days.

However, when treated only with tablets, especially if only antibiotics are used, then ureaplasma, as a rule, disappears from tests, but remains in the body.
Therefore, it is better to be treated correctly the first time and not resort to self-medication.
Remember! The result of any analysis is not a diagnostic conclusion.
A detailed diagnosis is made by the doctor based on examination, medical history and the results of all studies.
Often in this case the question arises: “to treat or not to treat?”
Preparation for PCR research
A test for ureaplasma is taken from women in the middle of the menstrual cycle, and not before the start of menstruation or after its end, as with a bacteriological smear. To obtain a reliable result of a PCR study, you must adhere to simple rules:
- Before taking the test, it is prohibited to treat with antibiotics;
- 2 days before the study, stop using local medications and contraceptives;
- wash themselves the evening before the test without using soap, and in the morning before the test, intimate hygiene and douching with antiseptic solutions are prohibited;
- 2 days before the study, sexual activity is completely excluded;
- it is forbidden to urinate for 3 hours before taking the test;
- It is not recommended to do a smear immediately after taking colposcopic samples to determine cervical tumors.
Culture culture for ureaplasma
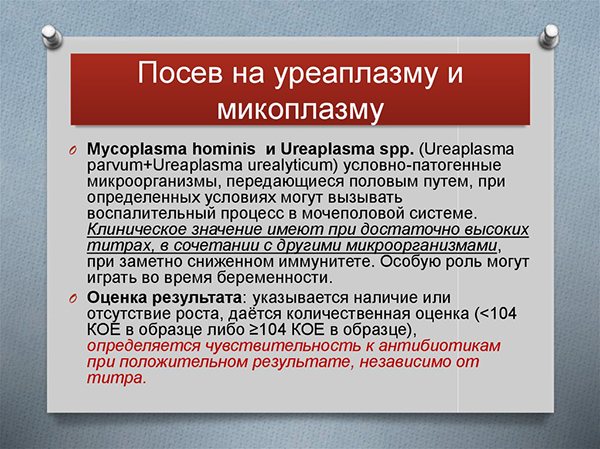
Cultural seeding is a modern and effective research method that helps determine the type of causative agent of ureaplasmosis:
- parvum;
- urealicticum;
- hominis.
The test is also used to determine the effectiveness of treatment. The advantage of this diagnostic method is the ability to determine the sensitivity of pathogens to the main groups of antibacterial drugs.
Material for sowing is collected from 3 points: from the walls of the vagina, the urethral mucosa and the cervical canal. The material is transferred to a nutrient medium and kept under appropriate conditions for 3 days. Then the causative agent of ureaplasmosis is identified.
Culture culture for ureaplasmosis is carried out no earlier than 2–3 days after the cessation of menstruation. It does not require special training. It is enough to follow the same rules as when taking a bacteriological smear. It is important to remember that during this period you should not take antibacterial drugs.
Preparation for analysis for ureaplasma is carried out in order to obtain accurate results and timely diagnosis. It is necessary to take a smear test with special responsibility, since only treatment at an early stage of the disease will prevent the development of irreversible complications.
Ureaplasma parvum: complications
The disease often occurs without significant symptoms.
Patients consult a doctor already at the stage of complications.
There are systemic complications of ureaplasmosis, especially arthritis and conjunctivitis.
These processes can begin simultaneously and are an important diagnostic sign.
Arthritis is usually accompanied by the manifestation of urethritis.
Other localizations of the process, such as pneumonia, are rare.
In addition to systemic complications, there may also be local unpleasant manifestations.
The process develops in the reproductive system.
In men, inflammation of the testicles and prostate often occurs.
The process of sperm formation is disrupted.
Ureaplasma is able to integrate intracellularly, the function of germ cells is lost.
This process leads to infertility.
Women suffer from ureaplasmosis much more often, and their complications are more severe.
An inflammatory process develops in the uterus and tubes.
Treatment can be quite long.