Analysis of stool for dysbiosis in children is considered the main method that can determine the immaturity of the gastrointestinal tract, as well as a violation of healthy intestinal microflora. Dysbacteriosis in an infant can be a consequence of many pathologies. Dysbacteriosis does not have a specific clinical picture, so it can occur, accompanied by various symptoms. Many manifestations of this pathology are similar to signs of other diseases of the digestive tract. For this reason, in order to diagnose dysbiosis, it is necessary to undergo appropriate laboratory tests. The correct collection of material for analysis deserves special attention. This process can be difficult for parents, since with dysbiosis the child may experience constipation or difficulty defecating. What do you need to know when collecting biomaterial for analysis?
What does the analysis for dysbacteriosis show?
Dysbacteriosis is an imbalance of intestinal microflora: a condition in which the number of pathogenic and opportunistic bacteria exceeds the number of beneficial ones.
According to the provisions of the regulatory document of the World Health Organization, it is not considered a disease, but many pediatric doctors prescribe tests in the first year of a child’s life to identify dysbiosis and its causes. With this diagnosis, the baby may experience prolonged constipation, diarrhea, abdominal pain, and allergic reactions.
Experts believe that stool analysis for dysbiosis in infants should reflect information about the biocenosis in the intestines. In fact, the analysis only reflects the microbial composition of stool. From it you can judge what the current state of the microflora is, but how normal it is for a particular child cannot be understood from it.
Collection instructions
It is very important that the child defecates naturally. Therefore, you need to wait for this moment, keeping the pot and “packaging” containers ready. Next, the feces are scooped up with a spoon from a container, which is then tightly closed and put in the refrigerator.
Help: Most often, children go to the toilet after eating.
You can collect feces from a baby for analysis from a diaper or diaper. But you should be careful not to scrape the surface, otherwise excess impurities may get into the biomaterial.
Symptoms and norms
When clostridia, lactose-negative enterobacteria, Klebsiella, Candida fungus, Staphylococcus aureus and other pathogens begin to predominate in the intestine over beneficial microorganisms, dysbiosis develops. Increased proliferation of microbes in a baby is accompanied by the following symptoms:
- regurgitation;
- diarrhea;
- blood, mucus in stool;
- constipation;
- diseases of the digestive system;
- increased accumulation of gases in the stomach (bloating);
- allergic reactions;
- abdominal pain;
- poor appetite;
- there are traces of white coating on the tongue;
- bad breath;
- the baby is often sick.
They will prescribe a dysbiosis test for the baby during or after antibiotic treatment. These medications can cope not only with pathogenic bacteria that have affected the body (clostridium, klebsiella, Staphylococcus aureus, etc.), but also kill beneficial microflora.
Dysbacteriosis can only be detected through stool analysis. Thanks to it, it is possible to determine which pathogenic bacteria have exceeded the norm, which will make it possible to prescribe the correct therapy. This is explained by the fact that to destroy the Candida fungus, different methods are needed than when activating clostridia, Staphylococcus aureus, Klebsiella or other pathogen.
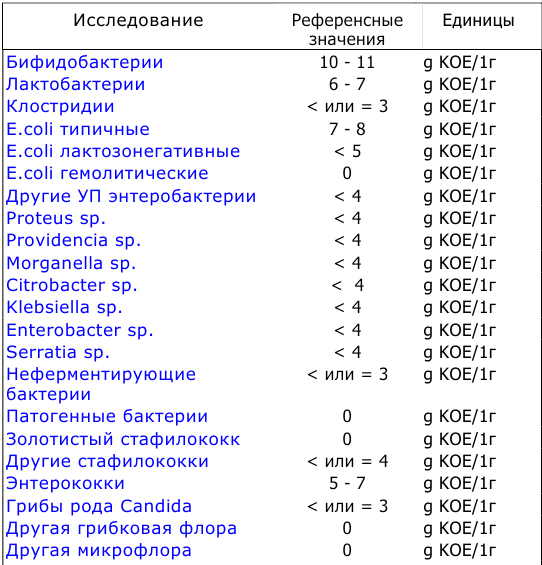
Normally, the number of beneficial and harmful bacteria in the intestines of a baby should fluctuate within the following limits:
| Bacteria | Normal for infants | Children 1 year | After a year | ||
| Form of feeding | |||||
| Chest | Mixed | Artificial | |||
| Bifidobacteria | 10 7 -10 11 | 10 6 -10 9 | 10 6 -10 8 | 10 10 -10 11 | 10 9 -10 10 |
| Lactobacilli | 10 5 | 10 4 -10 6 | 10 4 -10 6 | 10 6 -10 7 | 10 7 -10 8 |
| E. coli | 10 5 -10 8 | 10 6 -10 9 | 10 7 -10 9 | 10 7 -10 8 | 10 7 -10 8 |
| Lactose-negative enterobacteriaceae | 10 3 -10 6 | 10 5 -10 7 | 10 5 -10 7 | up to 10 4 | until 10 7 |
| Enterococci | — | 10 5 -10 9 | 10 6 -10 9 | 10 6 -10 7 | 10 7 -10 8 |
| Staphylococcus | 10 2 -10 4 | 10 3 -105 | 10 3 -10 6 | up to 10 5 | up to 10 4 |
| Clostridia | 10 1 -10 3 | 10 2 -10 4 | 10 3 -10 6 | up to 10 5 | up to 10 5 |
| Candida | 10 2 -10 4 | 10 1 -10 3 | 10 2 -10 4 | up to 10 3 | up to 10 4 |
It is not worth treating a child on your own, having only a transcript of the results in hand: a doctor must prescribe treatment. Each of these pathogens (clostridia, lactose-negative enterobacteria, Klebsiella, Escherichia) requires an individual approach to treatment. Otherwise, you can cause serious harm to the baby and provoke the development of chronic diseases that he will not get rid of even as an adult.
What will the tests show?
Only a doctor should interpret the results, but parents often want to know quickly whether there is cause for concern.
What is normal and what is not is listed in the following table.
| No. | Parameter | Norm | Possible deviations |
| 1 | Form | Decorated | Newborns are an exception; unformed, liquid and semi-liquid stools are normal. |
| 2 | Consistency | Dense | A waxy consistency can occur due to excessive consumption of fatty foods, as well as against the background of diseases of the gallbladder and liver. |
| 3 | Smell | Characteristic of feces, unsharp | A strong, foul odor is caused by fermentation or rotting of feces due to pancreatitis and dysbiosis |
| 4 | Color | All shades of brown | Black color – peptic ulcer of the stomach and duodenum. Colorless – gallstones, pancreatitis, hepatitis. Green – increased intestinal motility, red – ulcerative colitis |
| 5 | Acidity pH | 6-8 | High level of pH – diarrhea, fermentation processes, low – development of putrefactive processes |
| 6 | Blood | No | Yes – anal fissures, ulcerative colitis, hemorrhoids. This symptom is one of the first to occur in dysentery in children. |
| 7 | Slime | No | Yes – inflammation of the intestines, salmonellosis, dysentery. A small amount of mucus is allowed in the stool of children who are fed breast milk. |
| 8 | Undigested leftovers | No | Most cases are caused by poor diet |
| Reactions: | |||
| 9 | For protein | No | Yes – atrophic gastritis and chronic pancreatitis |
| 10 | For hidden blood | No | Yes – presence of parasites, duodenal ulcer, intestinal and stomach polyps |
| 11 | For bilirubin | No | Positive – acute gastroenteritis, food poisoning, antibiotic treatment |
| 12 | For stercobilin | Eat | No - anemia |
| 13 | Connective tissue fibers | No | Yes – insufficient absorption of nutrients |
| 14 | Undigested muscle fibers | No | Yes - poor digestion of meat foods, chronic pancreatitis and gastritis |
If all rules are followed, stool analysis will be as accurate as possible, which will avoid misdiagnosis and related problems. Many manipulations cause difficulties for inexperienced parents, so it is important to find out in advance how to prepare and collect material.
Causes of dysbacteriosis
The most common cause of dysbiosis is considered to be immaturity of the gastrointestinal tract. While the baby is in the mother's womb, its intestines are sterile. The first microorganisms enter it during childbirth, from the mother.
Dysbacteriosis in a child can also appear due to:
- late start of breastfeeding or lack thereof. Mother's milk contains an optimal range of nutrients and is a natural source of bifidobacteria. If a child eats breast milk from the very first day, then by the end of the first week an almost complete complex of necessary bacteria is formed in the intestines;
- use of antibiotics. The biggest risk associated with taking antibiotics is the loss of beneficial microflora. If a nursing mother took antibiotics, the process of deterioration of digestion will also be observed in the baby;
- early introduction of complementary foods. It is not recommended to introduce any complementary foods before six months - the baby’s body is not yet adapted to digest solid food;
- food allergies.
2Collect stool using a sterile container
A convenient and easy way to collect stool is to use a special sterile container with a plastic spatula attached to the lid. It is enough to collect the feces from the diaper or diaper with a spatula and close the container.
It is more difficult to collect liquid stool for analysis, since it is absorbed very quickly into a diaper or cloth diaper. To collect liquid feces in a container, it is advisable to use a medical oilcloth on which the baby is placed without a diaper. Oilcloth does not cause skin irritation, does not rustle or wrinkle. When using this method of collecting biomaterial, the temperature in the room where the child will be should be comfortable. The baby can wear a vest and socks, and if the baby falls asleep, he needs to be covered with a light diaper. When the child has emptied, you need to quickly collect the liquid feces with a spatula into a container.

Recommendations for parents
Parents of newborns should be especially attentive to the health of their children. To prevent the development of dysbacteriosis, it is necessary to monitor the baby’s hygiene, proper and timely complementary feeding, and a varied diet.
Breastfeeding plays an important role in the formation of proper microflora. If there are no problems with lactation, there is no need to stop feeding.
During treatment with antibiotics, the baby must take probiotics. What kind of medicine to choose for your child needs to be decided with the attending physician.
Possible mistakes
Many parents are mistaken if they think that the process of defecation will be accelerated by a heating pad applied to the child’s stomach or other warming methods. Do not give any medications, including laxatives. All this can only do harm.

Suppositories with glycerin are one of the last means to speed up bowel movements!
If stool is delayed, it is prohibited to insert soap, cotton swabs with Vaseline or cream into the anus. Vapor tubes are permissible only in extreme cases, when other methods are ineffective. Even the glycerin suppository, which is described above, is a “second” choice method.
Analysis collection rules
The rules for collecting stool for dysbiosis in infants include several important points.
1) 72 hours before the examination you should not:
- introduce new foods into the baby’s diet;
- give any medications, including prebiotics, sorbents, laxatives, etc.;
- give enemas or use suppositories.
Before the procedure, the child must empty the bladder so that urine does not mix with stool when a bowel movement occurs.
2) feces for dysbacteriosis in infants should be in the morning as much as possible.
3) the container must be delivered to the laboratory where the research will be carried out no later than 2-3 hours after stool collection. If necessary, the material for analysis can be placed in the refrigerator for a short time. You can't freeze stool! It is unacceptable to provide the laboratory with a jar of material for analysis that has been in the refrigerator all night, or obtained using rectal suppositories - to avoid the ingress of foreign impurities.
4) a stool test for dysbacteriosis in an infant is usually done within 1 week. During this period, data is gradually collected on the state of the baby’s intestinal microflora. Employees of the laboratory where the research is being conducted place feces in a specially created nutrient medium. All organisms contained in feces will grow in this environment. They will then be examined using a microscope.
Testing a stool sample
In general, stool test results are usually reported within 3 to 4 days, although parasite testing often takes longer to complete.
Examination of stool for blood
Your doctor sometimes checks your stool for blood, which can be caused by certain types of infectious diarrhea, bleeding in the gastrointestinal tract, and other conditions. However, in most cases, bloody discharge in a baby or toddler's stool comes from a small tear in the rectum, called a fissure, which is caused by straining through hard stool (this is quite common in babies and children with ongoing constipation).
Testing blood in the stool is often done using a quick test in a laboratory that can provide results immediately. First, the feces are smeared on a special card, then a few drops of a developing solution are placed on the card. An immediate change in color indicates that there is blood in the stool. Sometimes the stool is sent to a laboratory for a blood test, and the result will be reported within a few hours.
Stool culture
Stool can be cultured for pathogenic bacteria. The stool sample is placed in an incubator for at least 48-72 hours, after which any pathogenic bacteria are identified and isolated. Remember that not all bacteria in stool cause problems; in fact, about half of the stool is bacteria, most of which live there normally and are essential for digestion. In stool culture, laboratory technicians are most concerned with identifying the bacteria that cause disease.
To culture the stool, the laboratory will need a fresh or refrigerated stool sample. The best examples are loose, fresh stool; well-formed stools are rarely positive for pathogenic bacteria. Sometimes more than one stool will be collected for a single crop.
Swabs from your baby's rectum can also be tested for viruses. Although this is not done regularly, it can sometimes provide clues to certain illnesses, especially in newborns or very sick children. Viral cultures can grow for a week or longer, depending on the virus.
Checking stool for eggs and parasites
The stool may be tested for parasites and eggs (parasite egg stage) if the child has long-term diarrhea or other intestinal symptoms. Sometimes a doctor will collect two or more stool samples to successfully identify parasites. If parasites - or their eggs - are detected when a stool smear is examined under a microscope, the child will be treated for parasitic infestation. Your doctor may give you special parasite collection containers that contain chemical preservatives.
On Vikids you can:
Read similar articles or write your own.
Go to Forum
Find/Make an appointment with a pediatrician.
How to collect stool for analysis
So, the doctor ordered a test for dysbiosis in the baby. How to collect material for analysis?
Experts do not recommend using a diaper to collect feces. If the toilet is performed at a certain time in the morning, it is necessary to place the child on a clean oilcloth, and then carefully collect what happened from it.
If you have problems with bowel movements, you can help your baby by bending his legs towards the navel or laying him on his tummy. You can also use a rubber gas tube for stimulation, lubricating the tip with Vaseline. It needs to be inserted into the anus - shallowly - and rotated slightly. A few minutes after this procedure everything will happen. Feces need to be collected with a spoon, which comes with the container for testing.
You can also help your baby by giving him a tummy massage. Place your palm on the belly near the navel and gently massage your baby's tummy in a clockwise direction. Periodically press the baby's bent knees toward his stomach to speed up the process.
On the container with the received material, it is necessary to indicate the surname, first name and age of the child, as well as the time of stool collection.
Little tricks
There are some tricks that help you collect urine quickly and without difficulty:
- if a child sleeps in a diaper at night, then in the morning you just need to unfasten the diaper, the baby will become cool and he will pee;
- turn on the water - the murmur of water will speed up urination;
- press lightly with a warm hand on the lower abdomen, give a small massage;
- If the child already knows how to stand, then in the morning, in advance, turn on the warm water to heat the bottom of the bath. As soon as your baby wakes up, take him to the bathroom, put him in the bathtub and keep a container under him. The result will not take long to arrive.
Usually, the first morning urine is needed for research, but if a special analysis is required (according to Nechiporenko), then an average portion must be collected. But in a small child it is difficult to collect urine at all, and even more so the first urine in the morning. Therefore, just any morning urine sample is suitable for analysis.

Types of bacteria in the results of stool analysis for dysbacteriosis
Pathogenic and opportunistic bacteria
Pathogenic bacteria are bacteria that parasitize other organisms and can cause infection. Under favorable conditions they reproduce very quickly. Pathogenic bacteria are extremely harmful bacteria that are the causative agents of infectious diseases: typhoid fever, salmonellosis, dysentery, etc. Normally, these bacteria should not exist at all.
Opportunistic bacteria are bacteria that, under normal conditions, do not cause harm to human health. However, if health deteriorates and immunity decreases, they become pathogenic, can cause inflammation and lead to the development of certain diseases.
Gram-positive and gram-negative bacteria
They are named after the Danish scientist Gram, who first introduced these concepts into use. When staining microorganisms with a special dye—gentian violet—Gram noticed that one group of bacteria (Gram-positive) was stainable, while the other (Gram-negative) was not. The reason for this is the thickness of the cell wall.
Gram-positive bacteria produce spores and exotoxins. They pose a danger to the body. But their shell allows antibacterial drugs to pass through.
Gram-negative bacteria can also cause serious illness. They do not form spores, but under certain conditions their shell, when destroyed, releases endotoxins, which can lead to various serious diseases. Unlike gram-positive bacteria, their shell is insensitive to antibiotics.
The correct ratio of gram-positive and gram-negative bacteria maintains normal internal microflora in the body.
Bifidobacteria
Bifidobacteria are gram-positive anaerobic bacteria that are shaped like curved rods. They make up the bulk of the intestinal microflora. To date, more than 30 species of bifidobacteria are known. They inhabit the large intestine. In the body, bifidobacteria perform the following functions:
— ensure normal functioning of the intestines by producing organic acids;
- control the proliferation of bacteria and viruses in the body;
- fight allergens;
— ensure the absorption of microelements, break down proteins, fats and carbohydrates;
— stimulate intestinal motility, ensure the processes of protein and fat metabolism;
- support immunity.
Lactobacilli
Lactobacilli are also gram-positive bacteria. They are located in many parts of the gastrointestinal tract, including the oral mucosa. Their main function is to maintain a normal acid-base balance in the body: lactobacilli convert lactose that enters the body with food into lactic acid. Lactobacilli also actively fight harmful microorganisms and create optimal conditions for successful digestion.
Eschejeria
Eschericheria (non-pathogenic Escherichia coli) is a type of gram-negative rod-shaped bacteria that is part of the normal microflora of the gastrointestinal tract. The main functions are to ensure digestion, activate the immune system, destroy pathogenic bacteria, produce vitamins B1, B1, B3, B5, B6. A decrease in the number of Eschecheria may indicate the presence of worms.
As a percentage of other representatives of the intestinal microflora, Escherichia coli does not exceed 1%.
Bacteroides
Bacteroides is a genus of gram-negative anaerobic rod-shaped bacteria. They belong to opportunistic bacteria. They are representatives of normal intestinal microflora. Their main function is the breakdown of fats. A child who was recently born does not have them in the body; they appear after six months.
Enterococci in stool analysis for dysbacteriosis
Enterococci are a genus of gram-positive bacteria of the Enterococcus family (Enterococccaceae), the most important representative of the body's microflora. They have a round or slightly oval shape and multiply quickly at temperatures of 35-37 degrees. Enterococci exist even with a small amount of oxygen.
Enterococci are opportunistic bacteria; excess levels of these bacteria can cause inflammation.
When performing an analysis for dysbacteriosis, among other bacteria, the number of enterococci is also examined. Enterococci in an analysis for dysbacteriosis in an infant should not exceed the norm - from 105 to 107 per 1 gram of feces.
The main therapy for fecal enterococcus is bacteriophages. They are less harmful than antibiotics in terms of the number of side effects, and they are often prescribed to children when an excess of the permissible limit is detected.
Microbes of the genus Protea
Microbes of the genus Protea are a genus of gram-negative bacteria, facultative anaerobes. The average size of an individual is 0.6 * 2.5 microns. They belong to opportunistic bacteria. They can provoke the development of many serious diseases requiring hospitalization.
Klebsiella
Also included in the list of opportunistic microorganisms. If the body is weakened, it can lead to pneumonia, urinary tract infections, and diarrhea.
What does Klebsiella lead to? Read personal experience here
Staphylococcus aureus
Staphylococcus aureus is an opportunistic microorganism. Refers to pathogens that can cause sore throats, folliculitis and other acute pathologies.
Staphylococcus epidermidis
Also refers to opportunistic bacteria. Lives in the surface layer of the skin - the epidermis. Can cause cystitis, urethritis, kidney pathology, tonsillitis, laryngitis, damage to the reproductive system and respiratory tract.
Enterobacter
It is an opportunistic bacteria that lives in the large intestine. Can cause nosocomial infections, blood poisoning, damage to the respiratory and genitourinary systems.
Pseudomonas aeruginosa
Gram-negative bacterium, opportunistic organism. One of the most common pathogens of nosocomial infections. Retains viability even in disinfectant solutions. It can affect various organs - skin, eyes, ears, gastrointestinal tract, urinary tract.
Clostridia
Gram-positive bacteria. They live in the mycophore of the gastrointestinal tract, on the skin, and in the oral cavity. May cause tetanus, gas gangrene, colitis.
Features of therapy
Treatment largely depends on which microorganisms have deviated from the norm, whether there is mucus, blood and other particles in the stool that should not be there. The doctor, studying the results, makes a diagnosis no earlier than he analyzes all the indicators.
If the transcript shows a decrease in the amount of E. coli, this may indicate the presence of worms in the intestines. Sometimes the cause may be a decrease in enzymatic activity, which is why this bacterium does not bring any benefit (although it does not harm). Despite all the benefits of E. coli, its number should not exceed the norm. If this happens, it means that dysbiosis is developing in the body.
As for hemolytic E. coli, in young children they should be completely absent. These pathogens produce toxins that negatively affect the nervous system and intestines, and can also cause various intestinal diseases and allergies.

Deficiency of bifidobacteria and bacteroides leads to long-term intestinal disorders in both children and adults. These bacteria appear in the baby on the tenth day of life. At the same time, children born through cesarean section have significantly fewer of them than babies born naturally.
Lactose-negative enterobacteria in children and adults should not exceed the norm. If the analysis shows their increased proliferation, this can explain the baby’s heartburn, regurgitation, belching, and increased gas formation. Enterococci normally do not harm the body and are even beneficial. But if their number is higher than normal, they will cause the development of infectious diseases of the pelvic organs and urinary tract.
While non-pathogenic staphylococci do not particularly harm the body (within normal limits), the presence of Staphylococcus aureus is dangerous for children. It causes diarrhea, vomiting, abdominal pain, high fever in the baby, mucus and blood are present in the stool. Therefore, Staphylococcus aureus should be absent in the feces of infants . If Staphylococcus aureus is present in the body, then its effect depends on beneficial bacteria . If their number is normal, the body is not afraid of Staphylococcus aureus and the baby does not need treatment. In severe cases, hospitalization is required.
When the doctor prescribes treatment, his instructions must be followed. To destroy fungus, clostridia, Klebsiella, lactose-negative enterobacteria, Staphylococcus aureus, normalize the digestive system, and get rid of mucus in the feces, special medications designed for small children are needed.
During treatment, special attention should be paid to the nutrition of children, since in many cases it is an incorrectly selected diet that causes the growth of clostridia, enterobacteria, Klebsiella and other pathogens. The diet must be agreed with your doctor. If the baby is breastfed, the mother must follow the diet.
When testing for dysbacteriosis in a child’s body, a tendency is immediately revealed that confirms the immaturity of the organs of the digestive system. At the same time, this type of analysis confirms the existing imbalance in the intestinal microflora. Most often, with dysbacteriosis in infants or newborns, there is a risk of having any diseases, as a result of which a malfunction occurred in the body. In most cases, dysbiosis does not have pronounced symptoms and is usually similar to any other disease of the digestive tract. In this regard, it becomes quite difficult to determine and identify dysbiosis in the child’s body. Therefore, submitting stool for analysis is one of the reliable and accurate laboratory methods that can confirm this diagnosis.
What to do if you are constipated
A newborn can be given a light abdominal massage, making circular movements around the navel. There is no need to press hard. An exercise like a “bicycle” will also help to strengthen intestinal motility, when the child lies on his stomach, and the parent bends his legs at the knees and rotates them back and forth.
Carrying the baby in your arms can speed up the process. But not in the usual way, but with his back to himself and with his legs bent, pressed against his stomach. The child seems to be folded in half, as his knees will be next to his chest.
These actions are considered safe, they do not harm the baby and are therefore acceptable, for example, for colic.
In case of failure, you can use inert (non-medicinal) glycerin suppositories, which will not affect the results. They work by relaxing the sphincter muscles. Very young children should not be given the entire suppository, but ¼. And be sure to check that there are no sharp edges left after cutting.
The suppository is inserted into the anus slowly and shallowly, a maximum of a centimeter. It melts quickly and has an almost instant effect. The presence of glycerol in the analysis, if it gets there, will not affect the results in any way.
Decoding the analysis for dysbacteriosis
Below is a breakdown of the test for dysbacteriosis in infants . As mentioned earlier, the results of the test for dysbiosis may vary from child to child. The following indicators are considered the recognized norm for infants:
- Bifidobacterium spp. (bifidobacteria) - from 109 to 10 12. A decrease in numbers indicates the presence of dysbacteriosis.
- Lactobacillius spp. (lactobacteria) - from 107 to 109. . A decrease indicates a risk of exposure to allergens.
- E. coli with normal enzymatic activity – from 107 to 108.
- E. Coli with weak enzymatic properties - no more than 105.
- E. Coli lactose-negative - no more than 105. Excess means a violation of the intestinal microflora.
- E. Coli hemolytic – must be absent. The presence indicates a violation of the microflora and a tendency to allergies.
- Enterococcus spp. (enterococci) - from 105 to 107.
- Proteus spp. (microbes of the genus Protea) – no more than 104. Exceeding the norm is a sign of dysbacteriosis.
- Klebsiella spp. (klebsiella) - no more than 104.
- Other opportunistic bacteria - no more than 104.
- Enterobacter spp. (Enterobacter) - no more than 104. Excess can cause disease of the kidneys, urinary tract, genital organs, etc.
- Staphylococcus aureus (Staphylococcus aureus) – must be absent.
- S. epidermis (Staphylococcus epidermidis) – should not exceed 105.
- S. saprophiticus (saprophytic staphylococcus) – should not exceed 105.
- Fungi of the genus Candida are yeast-like fungi. Normally should be absent
- Non-fermentative gram-negative bacteria – should not exceed 104.
- Pseudomonas spp. (Pseudomonas aeruginosa) - should be absent from the analysis.
- Clostridium spp. (clostridia) – must be absent.
- Clostridium difficile – should be absent from the analysis.
The form with the results of the analysis may be different in different medical institutions.
Indications for examination in children
In infants, dysbiosis is most often caused by changes in diet and various diseases. Sometimes, when new products are introduced in children under one year of age, the frequency and nature of stool changes. However, after a few days everything returns to normal. It is worth thinking about the development of dysbiosis and conducting an examination of the baby if the following signs appear:
In older children, the signs of dysbiosis are in many ways similar to those in infants under one year old, only they, unlike babies, may complain of discomfort and abdominal pain. Dysbiosis is caused by poor nutrition, infectious diseases, food poisoning, poor environment, stress, helminthic infestations, and hormonal changes in adolescents.
Why do stool tests?
Fecal analysis is part of a study aimed at identifying malfunctions in the baby’s body while searching for foci of inflammation. It is usually prescribed when a baby has digestive problems, which are manifested by stool upset and anxiety. You can suspect something is wrong by the appearance of the stool, especially if it contains foam, mucus, blood and an unpleasant odor.
Stool analysis also helps identify parasites living in the baby’s intestines. Children most often have pinworms, which cause itching and redness of the anus. They reproduce at a tremendous speed; in the evenings, females crawl out of the anus, laying eggs. As a result, the child experiences unpleasant sensations.
Coprology, or general stool analysis, is prescribed for a number of symptoms:
- nausea, vomiting;
- yellowing of the skin, whites of the eyes;
- blood in stool;
- bloating and pain in the abdominal area;
- a sharp decrease in appetite and weight loss;
- changes in the consistency, color, or smell of stool.
The study will determine how the digestive system functions, whether there are any foci of inflammation, and whether food is being digested. The test determines whether there are enough enzymes needed for organ function. It also makes it clear whether there is hidden blood. If the result is positive, then an additional test is prescribed, which will reliably indicate the presence or absence of internal bleeding. At the same time, the indicators of a general blood test, which is always referred for when inflammation is suspected, change significantly.
A carbohydrate test allows you to determine whether your baby has lactase deficiency. In this case, the stool is usually liquid and foamy. It can be both frequent and too rare. Parents usually have to help their child go to the toilet.

Help with constipation
Proper preparation for the test and submitting it on time will help determine the cause of the child’s ailments. Only a doctor, pediatrician or gastroenterologist can decipher the results.
Note! Indicators alone are not the basis for making a diagnosis. The child’s well-being is important, which is assessed by the doctor during the examination.