Aliens somehow flew to Earth. We looked: glaciers are melting, ozone holes are growing, pandas are not reproducing. We began to think about why this was all happening. We went down to the Biryulyovo district of Moscow. They took a hundred people, stripped them, groped them, interrogated them. They concluded: the ozone holes are due to brunettes (there were a lot of them), pandas do not reproduce because of men - more than half of them were on the flying saucer. Well, global warming is because of the ruble: all the residents of Biryulyovo ended up with this currency in their pockets. The aliens flew to their home and, based on the results of the research, printed ten Ph.D. theses with their green tentacles.
This is how “dysbacteriosis analysis” is carried out. Let's talk about this diagnosis with GMS Clinic gastroenterologist Alexey Golovenko.
What's wrong with this study? Doctors often prescribe it!
- Let's make a reservation: it is prescribed by doctors only in the countries of the former USSR. Outside these states, simple stool culture to detect microflora imbalance is not performed. You will not find any indication of the need for this testing in the WGO guidelines for irritable bowel syndrome, or the ACG (American College of Gastroenterology) guidelines for acute diarrhea, or the AAFP (American Association of Family Physicians) standard for monitoring newborns with colic. Well, of course, there is no diagnosis of “dysbacteriosis” either in the International Classification of Diseases or in at least one (!) non-Russian-language textbook.
- Our gastrointestinal tract is home to at least 1000 (thousands!) species of bacteria, and the number of all identified species is 2172. When performing a “stool test for dysbacteriosis,” we place stool in a nutrient medium and wait for the growth (the appearance of colonies) of approximately 20 species of bacteria, which we have chosen only because they are able to grow in this nutrient medium. Most of the intestinal inhabitants are not cultivated, that is, we cannot see their colonies in a Petri dish with our own eyes. In other words, when drawing conclusions about the state of microflora based on the reproduction of 20 species, we ignore the vast majority of bacteria.
- The normal amount of bacteria in the stool, which we see in the dysbacteriosis test form, was determined in an unknown way. There is an entire industry standard for treating patients with dysbiosis. There is not a single phrase in it about why we should consider the content of any enterococci from 10^5 to 10^8 per gram of stool to be normal. The standard is full of references to literature, but, suspiciously, there is not a single foreign publication among them. Well, the articles and textbooks themselves do not describe how exactly the microflora of healthy and sick people was compared, that is, how exactly the conclusion was made about the normal content of a particular bacterium.
- The bacteria found in stool (which forms in the colon) is not the same bacteria found in the mouth or small intestine. In addition, the bacteria in the stool (that is, in the lumen of the intestine) are not the bacteria that live in the mucus that protects the intestinal wall. In general, an insane amount of foreign bacteria, fungi and viruses “fly” through our digestive tract. Fortunately, most of them cannot get close to the intestinal wall: the parietal microflora that lives there competes with the “aliens.” We call this phenomenon colonization resistance, and it is to it that we owe the fact that the very first opportunistic bacteria swallowed with a glass of Moscow water does not cause diarrhea in us.
- The composition and ratio of intestinal bacteria is different for each person. By studying (not by stool culture, of course, but by the most complex genetic methods) the composition of bacteria in the stool, you can, for example, guess whether a sample belongs to a resident of New York or the Amazon coast. Well, or in which region of a particular country (for example, Denmark). lives the person who sent his feces for analysis. In general, the true composition of the intestinal microflora is our “fingerprints,” and it is ridiculous to assume some kind of general norm, much less judge the “normality” of the flora based on only 20 species out of 1000.
- Whether bacteria will multiply on a nutrient medium depends not only on what bacteria live in the stool, but also on how the stool was collected (from the toilet, from sterile paper), how it was stored (in the refrigerator, near a radiator, near a window ), how quickly they were delivered to the laboratory. How many people who were recommended to test for dysbacteriosis read these instructions, according to which the stool needs to be collected in a sterile container, placed in the refrigerator and carried to the laboratory not by hand, but in a thermos with an ice cube? However, even when performing these actions, a normal doctor cannot interpret the result of the test for dysbacteriosis. Which means he shouldn’t even try to do it.
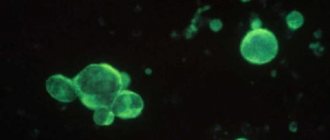
Colonies of bacteria appeared in the nutrient medium. Fortunately for us, the truly dangerous Salmonella grows in a nutrient medium. Most intestinal bacteria, alas, do not.
How to take the test correctly?
The reliability of the obtained test results for opportunistic flora is determined by the correct preparation of the patient, containers, direct collection of biological material and its storage. Typically, detailed recommendations regarding preparatory measures are given by the doctor during a consultation after prescribing the appropriate study.
Preparing for the test
Before collecting stool for analysis for opportunistic microflora, it is important to follow a few simple recommendations:
- Avoid drinking alcohol, fatty fried foods, sweets, and foods that enhance fermentation processes in the intestines a few days before collecting stool.
- 3 days before the study, it is advisable to stop taking medications (the possibility of taking medications is discussed with your doctor individually). Antibiotics, regardless of the route of entry into the human body, lead to the death of some intestinal microorganisms, which can cause unreliable test results for UPF (see more about how antibiotics affect microflora).
- You should not collect feces directly after an enema, the use of rectal suppositories, or after using sorbent preparations. Sorbents are a group of drugs that bind and remove toxic compounds and various microorganisms from the intestinal lumen with feces.
- Before defecation, it is recommended to toilet the perineal area with clean water without using detergents.
In infants, it is not recommended to introduce complementary foods before collecting stool. Preparatory measures for collecting stool for analysis of UPF in older children are not fundamentally different.
Preparing containers
To obtain reliable results of stool testing for opportunistic microflora, it is important to prevent various microorganisms from entering the material from the outside. Therefore, sterile containers must be used to collect material.
- The pharmacy sells special disposable sterile plastic containers for collecting stool.
- It is allowed to use small glassware (glass jars for food, preserves). They should first be thoroughly washed with clean water and then boiled for several minutes. This will destroy microorganisms on the walls of the dishes.
Be sure to read:
Types of impurities in feces, the reason for their appearance and diagnosis
Collection of material
Feces for analysis of opportunistic microflora are collected after a natural act of defecation. It is not recommended to collect feces from the toilet, so it is better to defecate on a prepared clean sheet of paper, polyethylene, or in a dry vessel. Stool collection is carried out using a clean wooden spatula or a disposable plastic spoon. A small volume of material, which should not exceed 1/3 of the container, is placed in a sterile container and screwed on with a lid. A direction with passport data must be attached to the container with the material taken for research. In children, feces are collected with a spoon from diapers or nappies.
Material storage
Quite often, feces taken for examination cannot be immediately delivered to the laboratory. It can be stored in a cool place at an air temperature of +3 to +5° C. The duration of such storage should not exceed 8 hours. The ideal option is to deliver the collected material to the laboratory within a period of time not exceeding 3 hours.
So, there is no such thing as “dysbacteriosis”?
Of course have. For example, pseudomembranous colitis - severe inflammation of the colon after an antibiotic - is a real dysbiosis: competitors have died, and therefore Clostridium difficile multiplies. Just to treat this, there is absolutely no need to state the obvious - the composition of bacteria in the intestine has changed. It is enough to confirm the infection (identify C. difficile toxins) and prescribe treatment.
Intestinal microflora, without a doubt, affects all processes in our body. By transplanting stool from an obese mouse to a mouse of normal weight, we induce obesity in the latter. The composition of gut bacteria is fundamentally different between people with anxiety and depression. Well, adding the probiotic Bacteroides fragilis to mice that have been artificially induced to have autism improves their social skills. Read the popular book “Look What's Inside You” by the famous microbiologist Rob Knight: our knowledge about microflora is colossal, but we are just beginning to apply it in practice (that is, to treat diseases).

The composition of bacteria can and should be studied. This is the subject of an ambitious international study, the Human Microbiome Project, with a budget of $115 million. Naturally, no “stool cultures” are used. Metagenomics methods are used to analyze the microbial jungle of the gut. They make it possible to describe how many unique DNA sequences are present in a particular person, which groups of bacteria predominate and which are absent. By the way, when such technologies (for example, 16S rRNA sequencing) appeared, it turned out that 75% of the species detected during genetic analysis of the same feces are not known to science at all.
Stop. So there is no point in doing stool culture at all?
I did not say that. We always perform a stool culture if we want to detect the growth of truly harmful bacteria. For example, in a person with bloody diarrhea, we look for Salmonella or Shigella, Campylobacter, or a special type of E. coli. Here, stool culture is vital, because this way we can prescribe antibiotic treatment to kill a specific pathogen.
A competent physician performs a diagnostic test only when the result may change treatment. If the same medicine or diet is prescribed for both a “deficiency” of lactobacilli and an “excess” of E. coli, the analysis is a waste of money.
A full study of one’s own microflora can already be done on a commercial basis in the USA and Europe. The “pleasure” costs about 100 euros, and as a result of a genetic analysis of the microflora you will receive a conclusion (for example, this one) about the bacteria predominant in your digestive tract. The problem is that these results cannot be applied in practice. Because:
We do not yet have a way to selectively change the composition of intestinal bacteria.
Suppose we have clearly established that a person has a deficiency of a specific microorganism (for example, lactobacilli). We can:
- Give a probiotic (that is, a specific live bacterium) and hope that it will remain living in the intestines.
- Give a prebiotic (that is, “food” for the bacteria) and hope that this will enhance the growth of the bacteria we need.
- Give an antibiotic (poison for the bacterium) and hope that it is the overly multiplied bacterium that dies.
- To transplant someone else's microflora into a person - to perform a fecal microbiota transplant (introduce diluted stool from a healthy person into a sick person).
Obviously, only the administration of a probiotic can be considered a selective action. The maximum dose of the best commercial probiotic is 10 billion viable bacteria per dose of the drug. The intestines are home to about 100 trillion bacteria. That is, for every bacteria “from the pharmacy” there are 10 thousand bacteria already “living” in the intestine. It is unlikely that this insignificant number of bacteria will be able to overcome colonization resistance and “populate” the intestine. In addition, the mechanism of action of probiotics (when they work) may generally be associated not with the bacteria themselves: in transgenic mice predisposed to intestinal inflammation, this very inflammation was stopped by using not a “live” probiotic, but in general DNA and some proteins isolated from a drug “killed” by temperature.
Well, and most importantly: theory and laboratory research are one thing, clinical trials (that is, studying the effect of drugs in people) are another matter. Let’s look at three typical situations for Russia when a person is asked to take a “stool test for dysbacteriosis”:
Colic in a newborn
The mother complains that the child cries a lot. By the way, any child in the first three months of life screams from 117 to 133 minutes per day (meta-analysis). The presence or absence of colic (unreasonable crying for more than 3 hours a day at least 3 days a week), in general, does not affect the risk of child developmental delay. In one study, simply talking to parents about colic "safety" reduced crying time from 2.6 to 0.8 hours per day. Children are empaths.

More often than not this is not the case. A stool test is performed for dysbacteriosis, and naturally (the norm is taken from the “ceiling”), “deviations” are found. A probiotic is prescribed. And it often helps: of course, because the frequency of colic inexorably decreases with the age of the child. However, we are not sure that probiotics are generally effective for colic. Numerous meta-analyses examining the treatment and prevention of this condition have failed to unequivocally confirm the effectiveness of probiotics. The probiotic Lactobacillus reuteri may have some beneficial effects. But in order to prescribe this drug, we do not need a stool test for “dysbacteriosis”.
Atopic dermatitis in a child
Everyone is sure that skin problems are caused by the “stomach”. If this were so, atopic dermatitis would probably be perfectly treated with probiotics. But this approach is not very effective. The latest meta-analysis shows that the use of probiotics (mainly Lactobacillus rhamnosus GG) slightly reduces the severity of eczema, but this effect is very symbolic, and additional probiotic therapy does not reduce the frequency of use of topical steroids, which (together with skin hydration) remain the mainstay of treatment for atopic dermatitis. And again: we can prescribe this probiotic regardless of the “results” of the “dysbacteriosis test”.
Bloating and abdominal cramps in an adult
Bloating is most often a symptom of small intestinal bacterial overgrowth (SIBO), which is helped not by a probiotic but by an antibiotic such as rifaximin. This condition is diagnosed using a special breathing test. Often, constant bloating is a consequence of exocrine pancreatic insufficiency: a deficiency of enzymes in the stool can be detected using a test for fecal elastase, and if it decreases, constant enzyme therapy can be prescribed. But most often, the feeling of “bloating” is associated with increased sensitivity of the gut (visceral hypersensitivity), which develops in people with irritable bowel syndrome. As you may have guessed, in order to assess the number of bacteria in the small intestine, the function of the pancreas, or the sensitivity of the intestine to distension, it is pointless to study 20 bacteria in the stool. And the effectiveness of probiotics for irritable bowel syndrome is questionable.
Decoding indicators
The interpretation of the results of a stool test for opportunistic microflora includes indicators of the number of certain types of bacteria; it is presented in the form of a table:
| Intestinal microorganism | Age, years | Content standard |
| Bifidobacteria | From 0 to 1 year | 1010 and above |
| Children over 1 year old and adults | 109 and above | |
| Lactobacilli | From 0 to 1 year | 106-107 |
| Children over 1 year old and adults | 107-108 | |
| Escherichia coli (total) | From 0 to 1 year | 107 |
| Children over 1 year old and adults | 108 | |
| Enterobacteria lactose-negative | From 0 to 1 year | 104 |
| Children over 1 year old and adults | 105 | |
| Enterococci | From 0 to 1 year | 105-107 |
| Children over 1 year old and adults | 105-108 | |
| Bacteroides | From 0 to 1 year | 107 |
| Children over 1 year old and adults | 108 | |
| Staphylococcus saprophytes | From 0 to 1 year | Under 104 |
| Children over 1 year old and adults | Under 104 | |
| Clostridia | From 0 to 1 year | Under 103 |
| Children over 1 year old and adults | Less than 105 | |
| Candida | From 0 to 1 year | Under 103 |
| Children over 1 year old and adults | Under 104 | |
| Peptostreptococci | From 0 to 1 year | 103-105 |
| Children over 1 year old and adults | 109-1010 | |
| Staphylococcus aureus | From 0 to 1 year | No |
| Children over 1 year old and adults | No | |
| Enteropathogenic Escherichia coli | From 0 to 1 year | No |
| Children over 1 year old and adults | No | |
| Proteus | From 0 to 1 year | No |
| Children over 1 year old and adults | No | |
| Pathogenic fungi | From 0 to 1 year | No |
| Children over 1 year old and adults | No |
Be sure to read:
List of intestinal antiseptics and their use
The interpretation and subsequent prescription of treatment, if necessary, is carried out by the attending physician.
Read on the topic: How to restore intestinal microflora at home