Nowadays, modern diagnostic methods are actively used in gynecological practice, allowing timely detection of pathology and modern treatment. Ultrasound of the pelvic organs is considered an informative, accessible, safe and painless method of examination. Of course, this procedure is the main one for many diseases, but diagnosing endometriosis using ultrasound can be very difficult, since the data obtained are indirect signs of the disease.
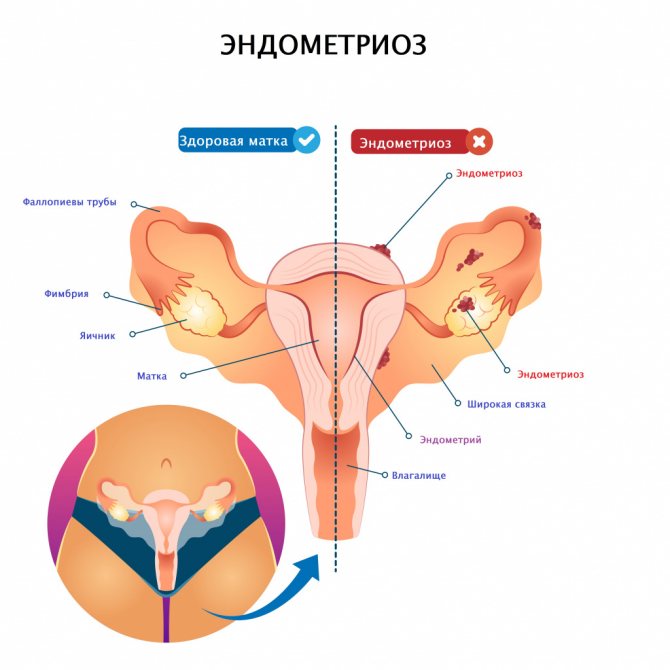
Endometriosis is a disease that is associated with the proliferation of tissue similar to the endometrium. Pathological foci can affect different parts and organs. Endometriosis is divided into internal (pathology affects the layers of the uterus) and external. There are also 4 degrees of endometriosis:
- Superficial lesions.
- Endometrioid lesions are located deep in the tissues; single cysts up to 6 cm are possible.
- Multiple pathological foci, spread of the process in width and depth, the appearance of small adhesions.
- Multiple foci and a pronounced adhesive process.
Internal, or genital, endometriosis is best seen on ultrasound. In this case, diagnostic signs are formed only at stage 2 of the disease. It is most informative to conduct an ultrasound in the late secretory phase of the menstrual cycle.
What is the essence of the disease?
The word "endometrium" translated from Latin means "inner lining of the uterus." We are talking about the same mucous layer that is shed once a month during menstruation. By definition, it should not be outside the uterus, but sometimes it manages to escape beyond its boundaries. The very phenomenon when some tissue is out of place is called ectopia. Having climbed beyond its allotted boundaries into the abdominal cavity, onto the fallopian (uterine) tubes, ovaries, and sometimes even into the lungs and very rarely into the mucous membrane of the eyes, the ectopic endometrial tissue continues to behave as if it remained in its place, then there is cyclic bleeding under the influence of female hormones. By the way, bloody tears, described in the Bible and a number of other sources, are considered by some scientists to be one of the rare manifestations of endometriosis.
Possible complications of endometriosis
Common complications:
- formation of scars and adhesions;
- inflammatory processes in the pelvis;
- peritonitis;
- ovarian exhaustion and cessation of ovulation;
- development of infertility;
- pregnancy pathologies;
- complications during childbirth;
- malignant degeneration of pathological tissues;
- increased risk of ovarian cancer.
The inability to conceive is a serious consequence of endometriosis. It is not great in the early stages of the disease, and increases significantly with the degree of its progression. This is due to the fact that overgrown endometrial tissue can block the fallopian tubes, which prevents the fertilization of a mature egg. Therefore, with endometriosis, you cannot postpone your planned pregnancy “for later.”
Why is endometriosis dangerous?
The root of the trouble is cyclic bleeding from the endometrium located in the wrong places. Because of this, the surrounding tissues become inflamed, which leads to an adhesive process. Adhesions not only cause pain, but also contribute to the development of infertility if, for example, they are located on the peritoneum of the small pelvis, in the depression between the uterus and rectum, or block the fallopian tubes, blocking the egg from reaching the uterus.
Photo: freepik.com
It also happens that the endometrium is not limited to the surface layer, but begins to penetrate deep into the uterus, causing adenomyosis. Likewise, ectopic tissue can grow into the cervix, vagina and ovaries, which is especially unpleasant. As a result, cysts with oozing blood appear here, which gynecologists call chocolate because of their characteristic color. Numerous endometrioid cysts around the ovaries also prevent the release of the egg and prevent a woman from becoming pregnant.
Local form of endometriosis of the uterine body on ultrasound
In the myometrium, individual bright hyperechoic inclusions without an acoustic shadow, irregular round, oval or blocky shape, size 2-6 mm, are found. These are areas of fibrosis around one or more endometriomas in the thickness of the myometrium. While cyclic processes occur in the foci, they can increase in size and take on the appearance of small, clearly defined nodes of irregular shape. In the local form of endometriosis, the uterus is of normal size and typical shape, the endometrium is not changed.
In almost all such cases, there is a habitual overdiagnosis of intramural fibromatous nodes with a predominance of fibrosis and calcification. Please note that the clear dependence of the lesion on the phase of the cycle indicates local fibronodular endometriosis.
How do pieces of mucous membrane get to other places?
This happens in different ways. In some people, endometrial ectopia occurs in the embryonic period at the stage of tissue and organ formation. For some reason, the intrauterine development program failed, and the result was endometriosis!
It also happens that some of the cells of certain tissues and organs are taken and transformed into endometriotic cells under the influence of hormones and other biological stimulants. And during menstruation, endometrioid cells easily enter the bloodstream and travel through the circulatory system to settle in one place or another in the body.
It’s good when a woman has only one of the mechanisms described above for the development of endometriosis, but what if suddenly all three? Then the disease will progress especially actively and persistently, which means you need to seek help from a doctor as early as possible. All necessary examinations can be completed at a medical clinic, or you can do nothing and wait for the disease to go away without the intervention of a doctor.
Causes of the disease
The most common cause is hormonal imbalance, in particular increased estrogen levels and progesterone deficiency.
The mechanism of development of the disease is not yet fully understood. The likelihood of developing endometriosis increases due to:
- hereditary predisposition;
- menstrual irregularities;
- endocrine pathologies;
- overweight;
- numerous abortions;
- chronic diseases that weaken the immune system;
- long-term use of an intrauterine device;
- significant or long-term stress;
- intense physical activity during menstruation;
- promiscuous sex;
- permanent toxic effects on the body.
Repeated curettage of the uterus during abortion also contributes to the scattering of endometrial cells beyond their natural location, and the occurrence of endometriosis.
Is it possible to hope that endometriosis will go away on its own?
This is indeed possible, but only with the onset of menopause, which in modern women occurs after 50 years. Are you really ready to wait that long, given that the active phase of endometriosis development occurs between 30 and 40 years, and the initial stage is often found in girls 25 years old or even younger? A couple of decades ago it was believed that endometriosis did not occur at this age. Even if its symptoms grow slowly, you still shouldn’t endure them for almost a quarter of a century, risking the opportunity to have children and your intimate life. The fact is that with this pathology it is painful to have sex, including from the back, especially if endometriosis has spread to the retrocervical canal, located between the posterior wall of the cervix and the rectum.
Degrees
Based on the depth of damage to the muscular body of the uterus by endometriotic formations, 4 degrees of pathology are determined.
- Endometrial cells are located only in the upper layer of muscle tissue.
- Endometrial cells penetrated deep into the middle of the muscle layer.
- The lesions spread throughout the entire thickness of the uterine walls.
- Endometriotic formations have invaded nearby organs.
At degrees 3-4, a typical complication often occurs: internal endometriosis in combination with uterine fibroids.
By what signs can endometriosis be recognized?
The main complaint with this diagnosis is pain. It begins a week before menstruation, intensifies to a maximum on critical days and gradually subsides within 2-3 days after their completion.
Unpleasant sensations of varying intensity occur in different places depending on where the source of endometriosis is located. If the bladder is affected, symptoms may resemble cystitis. Pain in the lower abdomen intensifies when trying to empty the bladder, and blood is often found in the urine.
And if pain occurs in the lower back, sacrum and tailbone, makes it painful to try to go to the toilet in a big way, and even blood appears on the toilet paper, the woman decides that her hemorrhoids have worsened. In fact, this is a typical picture of rectovaginal endometriosis, which has chosen its place in the space between the rectum and vagina.
Why hemorrhoids! Monthly attacks of appendicitis, clearly according to the menstrual calendar, with paroxysmal pain in the right lower abdomen, at which time the patient feels sick, can also be a consequence of endometriosis. This means that he sent his tentacles into the vermiform appendix.
If you have such pain or discomfort, consider visiting one of the qualified gynecologists in the Health network of medical clinics . Doctors have extensive experience in diagnosing endometriosis, regardless of its form - genital or extragenital, that is, extending beyond the genital organs.
Photo: katemangostar / freepik.com
Endometriosis of the ovarian ligaments on ultrasound
TA-ultrasound is optimal with a full bladder, then the ovaries are pushed upward, the ligaments are stretched and fully included in the image. During TV-ultrasound on an empty bladder, the ovaries descend, the ligaments hang and occupy an almost vertical position in relation to the vaginal vaults, the image includes transverse and oblique sections of the ligaments, which merge with the surrounding tissues.
On ultrasound, endometriosis of the ovarian ligaments is a hyperechoic nodule or a large linear adhesion up to 30-32 mm that covers the ligament in a muff-like manner.
What examination do you need to undergo?
Even a routine gynecological examination in a chair allows the doctor to suspect endometriosis by the enlargement of the ovaries and the presence of characteristic nodular formations. There are many of them, touching them causes discomfort in the patient. They are localized in the area of the uterosacral ligaments or between the rectum and vagina, increasing closer to menstruation and decreasing after their end.
Ultrasound examination using a vaginal probe will help clarify the diagnosis, and laparoscopy may be required for its final confirmation. This procedure allows you to view your pelvic organs through a flexible, fiber-optic tube. The device is inserted through a small hole in the lower abdomen. Don't be afraid, it won't hurt: the procedure is performed under local anesthesia. The latest equipment for ultrasound examination, as well as expert doctors from the Zdorovye medical clinic network, will help you quickly and accurately make a diagnosis.
Photo: tutatama / freepik.com
What can be seen in the photographs
An MRI examination clearly shows the location and extent of the disease. Foci of endometriosis are clearly visible.
- At the initial stage, thickening of the walls of organs and unevenness of their internal surface are clearly visible. Tubular structures are visible penetrating the inner lining of the uterus. MRI takes pictures - “slices” at short distances, which allows you to examine literally every centimeter of internal organs. Measuring the thickness of the walls and assessing their condition does not happen “by eye”, this is done by a computer program. Therefore, errors are excluded even at the very beginning of the disease, when tissue changes are not very pronounced.
- At the second stage of the disease, the difference in the thickness of the walls of the organ begins to become apparent. Cystic inclusions are visible, which are defined as dense nodular formations.
- At the third stage, you can see the spread of the pathological condition throughout the entire thickness of the tissue. Its heterogeneous structure is visible. Tumor surfaces vary in shape and size and are located randomly or in a single layer.
- The fourth stage of the disease is marked by the presence of endometriosis already in the peritoneal cavity. Adjacent tissues are affected by cystic and nodular formations. The photographs show their heterogeneity and friability. Adhesive processes develop.
Do not neglect the precautionary rules regarding your women's health. If any discomfort occurs in the pelvic organs, this may be a consequence of a serious disease. A competent doctor, having suspected endometriosis, will always prefer to play it safe and send the woman for an MRI examination in order to take timely measures to save the health and happiness of her patient.
How is endometriosis treated?
For those who managed to see a doctor in time, without allowing the disease to go far, hormonal therapy helps well. A specialist may also prescribe physical therapy for you. If endometriosis has entered an advanced stage, gentle endoscopic surgery is resorted to. Instead of a scalpel, there is a laser beam configured in such a way that multiple endometrioid inclusions, in the literal sense of the word, evaporate from the surface of the peritoneum and pelvic organs, while healthy tissue remains unharmed.
Instead of a laser, you can use cryosurgery - using the same laparoscopic method to freeze the endometrial islands with liquid nitrogen or freon. You can also destroy ectopic tissue with electric current: this method is called electrocoagulation.
When it comes to adenomyosis with hyperpolymenorrhea and the introduction of the endometrium into the rectum, the tactic is this: carry out hormonal therapy for several months to reduce the size and area of endometriotic growths, and then remove their remains surgically. In the Zdorovye network of medical clinics, a treatment regimen is developed individually for each patient, depending on the severity and extent of the disease.
Photo: romanzaiets / freepik.com
Endometriosis
ECO
Iron deficiency
2084 October 14
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Endometriosis: causes, symptoms, diagnosis and treatment methods.
Description
Endometriosis is a disease characterized by the growth of endometrial tissue (the inner mucous membrane of the uterine body) outside the uterine cavity.
Endometriosis can affect the muscular layer of the uterus, the internal genital area, the pelvic peritoneum, and even organs outside the reproductive system (kidneys, bladder, etc.). Endometriosis has the ability to penetrate into surrounding tissues and organs with their subsequent destruction, as well as metastasis (the appearance of distant secondary foci of elimination); has a chronic, relapsing course.
Among all gynecological pathologies, endometriosis ranks third, second only to fibroids and various inflammatory processes.
Approximately 30% of women of reproductive age complain of symptoms characteristic of this disease. The peak of endometriosis occurs in the age group from 30 to 50 years.
Causes of endometriosis
In healthy women, endometrial cells should not survive in unusual places due to their programmed death and the inhibitory effect of the peritoneum on their development. However, in patients with an established diagnosis of endometriosis, there is a decrease in the processes of spontaneous cell death in the foci of endometriosis.
There are several theories about the origin of this disease.
The theory of retrograde menstruation
suggests that endometriosis occurs due to retrograde flow and reflux of endometrial cells through the fallopian tubes into the pelvic cavity during menstruation.
Metaplasia theory
suggests that under the influence of hormonal or immune factors, some peritoneal cells transform into cells of the endometriotic lesion.
Hormonal theory
states that endometriosis develops as a result of a violation of the content and ratio of steroid hormones.
Theory of oxidative stress and inflammation
suggests that under the influence of reactive oxygen species, lipid peroxidation occurs, which leads to DNA damage in endometrial cells, the development of inflammation, which contributes to the attachment of fragments of endometrioid tissue to the surface of the peritoneum.
The immune theory
suggests that as a result of a defect in the immune response to the reflux of endometrial cells into the abdominal cavity, their removal is impaired, which promotes the implantation and growth of endometrial cells in areas unusual for their location.
Genetic theory
states that endometriosis can be hereditary.
The stem cell theory
states that endometriosis lesions form from stem cells outside the uterus.
Classification of endometriosis
I. Genital endometriosis (in the genital area):
- External, located outside the uterus:
- ovarian endometriosis,
- fallopian tube endometriosis,
- endometriosis of the pelvic peritoneum,
- endometriosis of the rectovaginal septum and vagina.
- Internal, located in the body of the uterus - endometriosis of the uterus (or adenomyosis).
II. Extragenital endometriosis (outside the genitals):
- intestinal endometriosis,
- endometriosis of the skin scar,
- other endometriosis (lungs, pleura, salivary glands, lacrimal glands, urinary organs, navel, etc.).
Symptoms of endometriosis
Foci of endometriosis look like nodules or nodes (from 1 to 30-40 mm in diameter) of dense consistency, having one or many cavities filled with fresh or altered dark blood.
In foci of endometriosis, under the influence of ovarian hormones (parallel to the menstrual cycle), cyclic transformations similar to changes in the mucous membrane of the uterine cavity occur. During menstruation, in foci of endometriosis, the epithelium exfoliates and disintegrates with hemorrhage into closed cavities.
During pregnancy, changes in the cells of the endometriotic lesion may occur, similar to changes in the uterine cavity in preparation for pregnancy.
Endometriosis has the ability to grow into any tissue or organ and destroy it.
Foci of endometriosis very rarely become a source of tumors (adenoacanths and adenocarcinomas).
With endometriosis, women may experience nagging pain in the lower abdomen and lumbar region throughout the menstrual cycle. The pain intensifies on the eve of menstruation. There may be scanty, dark chocolate-colored spotting before and after menstruation, prolonged and heavy menstruation and, as a result, a decrease in the level of red blood cells and hemoglobin in the blood.
Some women complain of pain during intercourse, which makes them avoid sexual activity.
When the endometrium grows into the bladder, there is pain when urinating and blood in the urine. When the endometrium grows into the rectum, blood may appear in the stool.
When the lungs are affected, a cough with bloody sputum is often present. Moreover, hemoptysis occurs with the onset of menstruation and stops with menstruation.
Before menstruation, many women complain of headaches, nervousness, worsening mood, decreased performance, and sleep disturbances.
Even with a small spread of endometriosis to the peritoneum (the thin translucent serous membrane that covers the inner walls of the abdominal cavity and the surface of the internal pelvic organs), severe pain can occur, leading to disability.
Diagnosis of endometriosis
Analysis of the patient's complaints and gynecological examination can only suggest a diagnosis of endometriosis. Additional research is required to confirm this:
- Ultrasound of the pelvic organs.
Diagnosis of endometriosis
Diagnosis of endometriosis depends on the location of the disease. For example, for cervical endometriosis, a gynecological examination with speculum and colposcopy is sufficient.
For other forms of the disease, the following types of examinations may be required:
- hysteroscopy (examination of the uterine cavity, fallopian tubes and cervical canal using a hysteroscope);
- laparoscopy, with biopsy of suspicious lesions;
- cystoscopy (examination of the bladder using an endoscope);
- ultrasound examination of the pelvic organs;
- CT, MRI;
- colonoscopy, rectoscopy;
- analysis for tumor marker CA-125.
What diseases have symptoms similar to endometriosis
Ovarian cysts
— Fluid contents with low signal intensity on T1-weighted image and high signal intensity on T2-weighted image
- Functional cysts decrease in size
— Smooth thin capsule, no septa
Dermoid cysts, teratomas
— Demonstrate the fat component: high signal intensity on T1- and T2-weighted images, low signal intensity on T1-weighted images in fat suppression mode
Ovarian neoplasms
— Solid mass with/without a cystic component, contrast enhancement of the solid component, hyperintense areas on T1-weighted image
Subserous leiomyoma
– Located next to the uterus, has a leg
— Low signal intensity on T1-weighted image
— Increase in signal intensity after contrast enhancement
Pregnancy with internal endometriosis
Pregnancy in the presence of pathology is unlikely, but the possibility of conception cannot be completely excluded. The disease poses serious threats to the development of pregnancy: spontaneous miscarriage, rupture of the uterine wall.
This is why it is necessary to regularly visit a gynecologist for a preventive examination: timely diagnosis of the disease (especially when planning pregnancy) significantly increases the chances of a successful outcome of its treatment.
To make an appointment or get advice, call the 24-hour number
+7
or fill out the form











