04 August 2021
Bronchial asthma is a chronic lung disease that causes obstruction of the bronchi
Bronchial asthma is a chronic lung disease in which obstruction of the bronchi occurs. In healthy bronchi, the lumen is free and allows inhaled and exhaled air to pass through the respiratory tract unhindered.
Due to the development of inflammation, swelling of the walls of the bronchi occurs, it thickens, and at the same time, a contraction of the muscle fibers of the bronchi occurs with the development of bronchospasm. In the spasmodic bronchi, mucus accumulates, which disrupts the free passage of air flow, resulting in a feeling of lack of air, shortness of breath, and wheezing.
In modern society, asthma is considered a serious problem due to the progressive course of the disease, which bothers patients with frequent attacks and causes a deterioration in their quality of life. Today, more than 100 million people in the world suffer from bronchial asthma, which on average for each country is 4-8% of the adult population. Every year, asthma causes the death of 250 thousand people.
The mechanism for the development of a spasmodic reaction of the bronchi is always an allergy. There are many reasons for its development; in addition, there are a number of factors of bronchial asthma that contribute to the development of the disease as a whole and the occurrence of individual attacks: a hereditary predisposition, which is observed in a third of patients.
If one of the parents is sick, then the probability of the child developing this disease is about 30%, and if both parents are sick, then more than 70%; bacterial or viral infections that are constantly present in the body; any dysfunction of the immune system; bad habits, primarily smoking; work in an atmosphere contaminated with small particles; living in poor environmental conditions; chronic poor nutrition; uncontrolled use of pharmacological drugs.
To make an accurate diagnosis and appropriate treatment, bronchial asthma is divided according to several factors. Regarding its origin, the following varieties are identified: allergic; non-allergic; mixed; unspecified.
Symptoms of bronchial asthma
What should you be wary of? Among the early signs of bronchial asthma are the following:
Choking or shortness of breath. The condition can occur both during physical activity and at complete rest, as well as when inhaling air contaminated with allergen particles.
Cough. It occurs simultaneously with shortness of breath and has an annoying character. The cough is unproductive, and only at the end of the attack is it possible to release a small amount of sputum.
Shallow breathing. An asthma attack is accompanied by frequent shallow breathing and the inability to take a deep breath
Wheezing. They accompany a person’s breathing during an attack and are sometimes heard even remotely.
Orthopnea position. This is the position that a person reflexively takes during an attack - sitting, dangling his legs, tightly grasping a chair, bed or other object with his hands. This pose promotes deeper exhalation.
With exacerbation of asthma, these symptoms may include bloating of the chest, difficulty speaking, drowsiness, and rapid heartbeat. In atopic bronchial asthma, asthma attacks are often accompanied by a runny nose (stuffy or watery discharge, sneezing) and itchy skin, especially when in contact with an allergen (for example, when staying in a dusty room). The symptom intensifies during active games, stressful situations (during crying, fear), at night.
Examination program “Bronchial asthma”
Are you suspected of having bronchial asthma?!
BRONCHIAL ASTHMA
(from the ancient Greek άσθμα/ásthma - heavy, intermittent breathing, shortness of breath) is a chronic inflammatory disease of the respiratory tract, in which many cells and cellular elements take part.
Chronic inflammation causes bronchial hyperresponsiveness, which leads to recurrent episodes of wheezing, shortness of breath, chest tightness and coughing, especially at night and in the early morning. These episodes are usually associated with varying degrees of narrowing of the airways in the lungs, which are often reversible either spontaneously or with treatment (defined by the Global Strategy for the Treatment and Prevention of Asthma, GLOBAL INITIATIVE FOR ASTHMA/GINA).
The key mechanism of bronchial asthma of any origin is increased reactivity of the bronchial tree, which leads to reversible bronchial obstruction. A serious complication of the disease is status asthmaticus.
The main symptoms of the disease are:
Cough, episodes of shortness of breath, wheezing, asthma attack
(typically a forced position of the patient),
congestion in the chest, pain in the lower part of the chest
(with prolonged attacks of suffocation). Symptoms appear after contact with the allergen. There is also seasonal variability in symptoms. In some patients, the only trigger for an attack is physical activity.
The correct diagnosis can only be established through a comprehensive examination
Examination program for suspected bronchial asthma:
Doctor visit:
- examination and consultation with a pulmonologist, candidate of medical sciences; if necessary, an ENT doctor, an allergist-immunologist;
Laboratory diagnostics:
- general clinical blood test (detailed analysis, erythrocyte sedimentation rate, leukocyte formula (with microscopy of a blood smear in the presence of pathological changes);
- blood test for C - reactive protein;
- blood test for total immunoglobulin E (IgE);
- if necessary: blood test for specific immunoglobulins E (IgE);
- general sputum analysis (if available);
Instrumental diagnostics:
- chest x-ray;
Functional diagnostics:
- study of external respiration function, including:
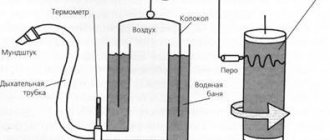
- spirometry;
- test with a bronchodilator;
- pulse oximetry;
- measurement of nitrogen monoxide (NO) in exhaled air;
- If necessary, a provocative test with methacholine is performed.
Repeated consultation with a pulmonologist, candidate of medical sciences based on the results of the studies, primary verification or confirmation of a previously established final diagnosis (if there is no need for additional examinations), determination of tactics or further tactics (if the patient has previously been prescribed a comprehensive therapy) management and treatment.
The information presented in this section is for informational purposes only. The required scope of examination is determined by the doctor individually.
Sign up for an examination by phone +7
Diagnostics
Diagnosis is based on an analysis of complaints, life and disease history, medical examination data, laboratory tests, special functional and allergological tests. A careful study of complaints and medical history (especially first-time attacks) allows us to suspect asthma in 70% of cases. For this purpose, there are special questionnaires developed by allergists. Instrumental diagnostic methods are also widely used: x-rays of the chest and sinuses; electrocardiography; study of external respiratory function with peak flowmetry; diagnostic bronchoscopy; tests for bronchial reactivity under the influence of various drugs and physical activity
spirometry.
The main method for diagnosing bronchial asthma is spirometry (external respiration function test). Spirometry must also be carried out to monitor the progress of asthma treatment: it is necessary to focus not only on the presence or absence of complaints during treatment, but also on the objective indicators that spirometry provides. There are simple devices (peak flow meters) for independent use by asthma patients.
During the interictal period, pulmonary function may be normal; sometimes in these cases provocative tests are performed, usually with methacholine. A negative test with methacholine excludes bronchial asthma, but a positive test does not yet confirm this diagnosis. The methacholine test is positive in many healthy people; it may be positive, for example, for several months after a respiratory viral infection.
Chest X-ray is mandatory for severe attacks, as it allows us to identify hidden complications that require immediate treatment. To identify provoking factors, allergic status is determined. Blood and bronchial mucus tests determine the severity of the disease. The examination plan is developed by the attending physician individually for each patient, taking into account the recommendations received during consultation with an allergist, pulmonologist and ENT specialist.
Diagnosis of bronchial asthma
Making a diagnosis of bronchial asthma
Asthma is no longer considered a condition with isolated acute episodes of bronchospasm.
It is now commonly characterized as a chronic inflammation of the airways, due to which the bronchial tree becomes constantly sensitive or hyperreactive. When hyperreactivity occurs when exposed to various stimuli, obstruction of the bronchial tree occurs (Fig. 2) and exacerbations (or attacks) of the disease occur, manifested by coughing, wheezing, a feeling of constriction in the chest and difficulty breathing. Attacks can be mild, moderate, severe, or even life-threatening. The reasons for the appearance of initial inflammation in the respiratory tract of the airways in patients with asthma remain to be clarified. Currently, the most important risk factor is considered to be atopy, a congenital hereditary tendency to allergic reactions. The most common allergens that are risk factors for the development of the disease are house dust mites, furry animals, cockroaches, pollen and mold. A powerful risk factor, especially in young children, is passive smoking. Chemical and air pollutants can sensitize the respiratory tract and lead to the development of bronchial asthma. Respiratory viral infection, prematurity and poor nutrition are also associated with the development of asthma. Many of these risk factors (house ticks, pollen, animals covered with hair, air pollutants, tobacco smoke, viral respiratory infections) can also cause exacerbations of bronchial asthma, so they are also called triggers. Other triggers include smoke from burning wood, physical activity (including running and other forms of exercise), excessive emotional stress (laughter, excessive crying), cold air and weather changes, nutritional supplements and aspirin. For someone with asthma, one or more triggers may be important, and different people have different triggers. Avoiding exposure to the trigger can reduce the risk of respiratory irritation (see Identifying and Managing Risk Factors). The risk can be further reduced by taking medications that target inflammation in the airways.
| Fig.Z. Is this asthma? Ask the patient or parent these key questions if you suspect you have asthma. Has the patient had attacks or repeated episodes of wheezing (high-pitched whistling sounds during exhalation)? Does the patient have a cough that worsens especially at night or upon awakening? Does the patient wake up with a cough or difficulty breathing? Does the patient cough or wheeze after physical activity, including running or other exercise? Does the patient have difficulty breathing during certain seasons? Does the patient have coughing, wheezing, or chest tightness when inhaling allergens or irritants? Does a cold “go down” to the chest and does it take more than 10 days to recover? Is the patient taking any medications when symptoms appear? How often? Do symptoms go away after taking medications? If the patient answers “Yes” to any of the questions, asthma should be suspected. However, it is important to be aware of other causes of respiratory symptoms (see Difficulties in Diagnosis). |
Most exacerbations (or attacks) can be prevented by simultaneously avoiding the trigger and taking anti-inflammatory medications; the effectiveness of such prevention depends on who has asthma, how well the acute symptoms are controlled, and how well the medications are prescribed and the triggers are identified.
History and nature of symptoms
The clinical diagnosis of asthma is often based on the presence of symptoms such as occasional shortness of breath, wheezing, chest tightness and cough, especially at night or in the early morning. However, these symptoms themselves cannot be the only diagnostic criterion, nor can they be the basis for determining the severity of the disease. When studying the history, it is important to establish the dependence of the onset of symptoms on exposure to one or more triggers. The disappearance of symptoms after using bronchodilators means that the doctor is dealing with bronchial asthma. In Fig. 3 provides questions to clarify the diagnosis of bronchial asthma.
Clinical examination
Because the symptoms of asthma vary throughout the day, your doctor may not detect symptoms that are characteristic of this disease during an examination. Thus, the absence of symptoms during the examination does not exclude the diagnosis of asthma. During an attack of bronchial asthma, spasm of bronchial smooth muscles, edema and hypersecretion lead to a narrowing of the lumen of the small bronchi. To compensate for this condition, the patient hyperventilates his lungs to keep the air flow through the bronchi at the same level. The greater the obstruction of the bronchial tree, the more pronounced the hyperventilation, which should ensure normal flow of air into the alveoli. Thus, if a patient has symptoms of asthma, then the likelihood of having the clinical manifestations presented below is quite high. Shortness of breath Wheezing, especially when exhaling Nasal flaring when inhaling (especially in children) Intermittent speech Agitation Acute emphysema (use of accessory respiratory muscles, raised shoulders, forward bending of the body, reluctance to lie down - orthopneic position) Cough Constant or recurring Worse at night and early morning, sleep disturbance Associated conditions Eczema Rhinitis Hay fever When diagnosing asthma, do not rely solely on the presence of wheezing or other auscultatory phenomena. Obstruction of the small bronchi may be so severe that wheezing is not heard. A patient in this condition usually has other clinical signs indicating the severity of the condition, such as cyanosis, drowsiness, difficulty speaking, tachycardia, and acute pulmonary emphysema (see "Determining the severity of bronchial asthmaTeaching patients" in the part that discusses the issue of the need for long-term monitoring of PEF).
Assessment of allergological status
In some patients, the allergy status can be determined by performing skin tests or determining specific IgE in the blood serum. Positive skin tests in themselves do not confirm the diagnosis of bronchial asthma, however, comparing their results with the patient's medical history allows us to identify asthma triggers, which helps to develop an effective management plan. In addition, examinations of children with asthma show that allergies influence the persistence and severity of the disease.
Difficulties in diagnosis
Often the diagnosis of asthma is not established immediately, which leads to incorrect and ineffective treatment (for example, courses of antibiotics and cough suppressants). It should be assumed that a patient with bronchial obstruction and associated symptoms suffers from bronchial asthma until proven otherwise. In some cases the diagnosis is especially difficult. In children, asthma symptoms often appear only during a viral infection, during physical activity, or only as a night cough. A diagnosis of asthma should be considered if a child's cold "sinks into the chest" or takes more than 10 days to recover. The presence of recurrent episodes of nighttime cough in an otherwise healthy child should alert the physician to asthma as a possible diagnosis. Night coughs can be explained by recurring sinusitis, tonsillitis and adenoids, but if this symptom causes the child to wake up in the early morning hours, it is almost always asthma. A good response to asthma medications can help make the diagnosis. Young children may experience episodes of bronchial obstruction associated with an acute respiratory viral infection (often as the first episode of bronchiolitis caused by respiratory syncytial virus). Typically, in children without a family history of atopy, symptoms disappear with age, but if there is a strong family history of allergies, the child may develop asthma. Therefore, in young children with repeated obstruction of the bronchial tree, the presence of bronchial asthma can be assumed. Repeated episodes of bronchial obstruction respond better to anti-inflammatory drugs than antibiotics. Smokers often suffer from chronic obstructive bronchitis, and they exhibit symptoms similar to those of bronchial asthma: cough, sputum production and wheezing. It is necessary to find out whether they also suffer from bronchial asthma and whether anti-asthma treatment can help them. Convince a smoker to quit smoking. Older people may also have undiagnosed asthma, the symptoms of which can be relieved. Their asthma can be confused with bronchiolitis, emphysema and interstitial fibrosis of the lungs. An increase in PEF by 15% after anti-asthmatic treatment confirms the diagnosis of bronchial asthma. However, failure to perform functional tests can make diagnosis difficult. People whose occupations expose them to inhaled chemicals and allergens may develop asthma. Occupational asthma is often mistaken for chronic or chronic obstructive bronchitis, leading to untreated or inappropriate therapy. In this case, early recognition of the disease is necessary (peak flowmetry at the workplace and at home), cessation of further contact with the substance and early initiation of treatment. People suffering from seasonal asthma have inflammation in the respiratory tract that defines the disease, but symptoms only occur at certain times (pollination of trees, grass, etc.). In patients with the cough variant of bronchial asthma, wheezing is rarely observed, but cough is the main, if not the only, symptom of the disease. Often a cough occurs at night, and during the daytime examination no abnormalities are noted. Patients with repeated acute respiratory infections (ARI), especially in children, may have undiagnosed bronchial asthma, since the symptoms of ARI and asthma are similar. In developing countries, ARIs more often occur in the form of bacterial pneumonia, which requires treatment with antibiotics. When a child with bronchial obstruction responds well to short-acting bronchodilators and has no other signs of pneumonia, this indicates asthma. In this case, the diagnosis of asthma must be confirmed and long-term treatment prescribed. If in patients with suspected asthma there is no effect from 1 - 2 courses of treatment, then perhaps they do not have bronchial asthma. The following alternative diagnoses are possible:
- localized airway obstruction
- laryngeal dysfunction
- gastroesophageal reflux
- Chronical bronchitis
- emphysema
- cystic fibrosis
Determining the severity of bronchial asthma
The severity of asthma varies. The course of the disease can be intermittent, mild, moderate or severe (Fig. 5). Attacks of the disease can be mild, moderate or severe. The course of asthma varies from person to person at different times. For example, asthma can be moderate in childhood, mild in adulthood, and severe in certain seasons. The severity of the disease is determined based on symptoms and clinical picture. However, it would be wrong to focus only on these parameters, and the use of peak flowmetry allows one to obtain additional information (up to 5 years, determining and monitoring the degree of severity by studying pulmonary function, including using peak flowmetry, is impossible). Treatment of bronchial asthma is based on a stepwise approach, in which the intensity of drug treatment increases (step up) with increasing severity and decreases (step down) with a sustainable effect.
Bronchial asthma: genetics and immunity
Today, bronchial asthma, along with allergies, has acquired the status of another “disease of civilization.” According to leading experts, in addition to genetic predisposition, excessively “sterile” living conditions, especially in early childhood, contribute to such an increase in morbidity. And among the triggers of pathology there are thousands of different agents.
Genetic basis
An asthma attack is known to be accompanied by wheezing, shortness of breath (or suffocation) and coughing, followed by the production of viscous, glassy sputum. This is due to the excessive activity of initially protective mechanisms.
Normally, any damage to bronchial cells is accompanied by:
- increasing mucus production and increasing its “stickiness” in order to more effectively “glue” damaging substances together;
- an increase in the tone of the “bronchial muscles” and a narrowing of their diameter, which not only reduces the “new” intake of irritants, but increases the pressure and speed of the outgoing air flow (one of the cough mechanisms), promoting the movement of mucus outward.
In the case of bronchial asthma, the receptors on the surface of the bronchi become overly sensitive to the action of even “ordinary” factors, which can provoke almost complete closure of the lumen of the bronchi due to spasm and mucus.
This predisposition is believed to have a genetic basis. However, there are about a hundred genes supposedly “culpable for asthmatic tendencies.” And just the presence of a mutation in them is not a guarantee of future asthma. To activate pathology, trigger factors are needed.
Immunity
As already noted, one of the factors in the prevalence of pathology is “household sterility,” and the basis for future asthma is laid precisely in childhood.
This theory of the disease is due to the fact that the child’s immunity is characterized by special plasticity and “learnability”. And this allows the immune forces to learn to distinguish between threatening and harmless “everyday” stimuli. And also remember the response options in this or that case.
In immunological terms: upon contact with bacteria, viruses and parasites, the activity of the immune system shifts towards T-helper lymphocytes type 1 and, at the same time, the activity of T-helper cells type 2, which stimulate the production of immunoglobulin E (IgE), responsible for asthma and allergies, is suppressed.
In other words, the more stimuli the immune system is “acquainted with” in childhood, the less “attention” it will pay to them in adulthood. And what the immune system does not have time to “get acquainted with” is “read” in an adult as a threat and is accompanied by a pronounced response.
Triggers
The most common triggers for the development of asthma are household allergens:
- animal fur,
- house dust mites
- and the dust itself,
- mold (especially black mold)
- and cockroaches.
And also, “allergenic” trees and grasses play a significant role, however, in this case, exacerbation of asthma is seasonal and associated with flowering; and some food products (peanuts, cow's milk and others).
In general, of course, asthma is not necessarily linked to these allergens and any other substances can provoke pathology. However, the listed allergens are still much more likely than others to become the culprits of the disease.
In this case, the concentration of IgE, both general and specific (to a specific allergen), increases in the blood. And in a general blood test, the level of eosinophils increases, although not in all cases.
Thus, if “asthma-like” symptoms occur, you should immediately exclude a reaction to the most “common” allergens. And, if one is not identified, look for the irritant more individually.
In children, asthma also often occurs against the background of gastroesophageal reflux disease (GERD). When, for a number of reasons, the acidic contents of the stomach are thrown back into the esophagus, entering, reflexively irritating the respiratory tract. The tendency to hyperreactivity is activated and the bronchial mucosa is damaged during coughing attacks
Eliminating reflux, in most cases, completely eliminates cough symptoms or leads to a significant improvement in the condition.
Treatment of bronchial asthma
Before treating BA, clinical signs determine what degree of severity it corresponds to. This can be an intermittent form with symptoms occurring less than once a week, a mild persistent form with symptoms appearing several times a week, and a severe persistent form with daily manifestations. It should be noted that the severity of asthma exacerbation does not correlate with its clinical form. First of all, measures are taken to eliminate allergenic factors from the patient’s life: from organizing a hypoallergenic lifestyle to dietary restrictions. In addition, careful, mainly using conservative techniques, sanitation of foci of chronic infection is required. Smokers are required to stop smoking. As a rule, the selection of drug therapy is carried out after monitoring PEF for 2–3 weeks. During monitoring, it is advisable for the patient to achieve 80% of the expected PEF (the required values are indicated in all instructions supplied with the peak flow meters). If this does not happen, then it is necessary to determine the best value for it, but already against the background of a course of taking, for example, glucocorticosteroids (GCS) for oral use. The purpose of prescribing medications for the treatment of asthma is to prevent or prevent the symptoms of bronchospasm. For this purpose, control (anti-inflammatory, basic) drugs and emergency drugs are used to eliminate developed bronchospasm (symptomatic drugs). Basic drugs are intended for long-term daily use, which allows you to control the course of the disease. Symptomatic medications are used to quickly eliminate bronchospasm, coughing attacks, wheezing and whistling in the chest. Drugs in this group are used situationally. Basic therapy drugs for asthma:
- GCS for inhalation use.
- Antileukotriene drugs.
- Long-acting ß2-agonists for inhalation use.
- Long-acting ß2-agonists for oral use.
- Preparations of the cromones group: “Sodium cromoglycate”, “Nedocromil sodium”.
- "Theophylline."
- Antibodies to immunoglobulin E.
- Systemic GCS.
- Oral antiallergic drugs.
- Allergen-specific immunotherapy.
AD is still classified as an incurable disease, but it can be controlled with basic therapy.
Essential drugs
There are contraindications. Specialist consultation is required.

- Acolat (Zafirlukast) is an anti-leukotriene drug for the prevention of attacks and maintenance treatment of asthma. Dosage regimen: prescribed orally, 1 hour before meals or 2 hours after meals. Should not be taken with food. The initial dose is 20 mg 2 times a day; maintenance dose - 20 mg 2 times a day; the maximum dose is 40 mg 2 times a day. The drug must be taken regularly.
- Ipratropium bromide (Atrovent N) is an M-anticholinergic, bronchodilator. Dosage regimen: for adults and school-age children, 2 inhalation doses (injections) 4 times a day are recommended. The total daily dose should not exceed 12 inhalations per day.
- Beclomethasone (Beclazone) is a glucocorticosteroid (GCS) for inhalation. Dosage regimen: inhalation - recommended for adults: 400-800 mcg per day in 2-4 doses. When the patient's condition stabilizes, the dose is reduced. High dosage regimen: for adults - 1500-2000 mcg per day, with further gradual reduction of the dose when control of asthma symptoms is achieved. The maintenance dose is 100-200 mcg 2 times a day. For metered dose inhalers, a spacer should be used to optimize penetration of the aerosol into the distal bronchial tree. Powder for inhalation is administered by inhalation using the included inhalation device (dishaler, etc.). Intranasal: 50 mcg (1 injection into each nasal passage) 2-4 times a day (200-400 mcg/day), then the dose is reduced depending on the patient’s response. Beclomethasone can be used in combination, inhalation and intranasally, in a total daily dose of up to 1000 mcg in adults.
- Salbutamol (β2-adrenergic stimulant). Dosage regimen: dosage forms - dosed aerosol for inhalation. Solution for inhalation (nebula). Powder for inhalation with inhalation device. Pills. Solution for infusion. To relieve asthma attacks, 200 mcg is prescribed once (1-2 inhalations). If there is no effect after 5 minutes. repeated inhalation is possible. Used to improve the penetration of basic anti-asthmatic drugs to the distal parts of the bronchial tree - 100-200 mcg 15-20 minutes before inhalation of sodium cromoglycate, nedocromil sodium or inhaled glucocorticoid. The powder for inhalation is administered using an inhaler (diskhaler, cyclohaler). Tablets for oral administration are swallowed whole without chewing. Long-acting forms and bilayer tablets: 8 mg every 12 hours; maximum dose - 32 mg/day.
- Montelukast (Singulair) is an anti-leukotriene drug for the treatment, prevention of attacks and basic therapy of asthma. Dosage regimen: taken orally 1 time per day, regardless of meals. When treating bronchial asthma, it should be taken in the evening. The dosage is one 10 mg tablet per day before bedtime. The patient should be advised to continue taking Singulair even after control of asthma symptoms is achieved, as well as during periods of exacerbation of asthma. Singulair can be added to the treatment of patients whose asthma is not controlled by bronchodilators alone (salbutamol, fenoterol, salmeterol, formoterol). Once a therapeutic effect appears (usually after the first dose), the patient's bronchodilator treatment can be reduced accordingly. Singulair cannot immediately replace inhaled corticosteroids.
- Seretide (combined anti-asthma drug for inhalation use). Dosage regimen: intended for inhalation only. Seretide aerosol for inhalation: 1 aerosol dose of Seretide contains salmeterol 25 mcg, fluticasone propionate 50; 125 mcg and 250 mcg. Seretide powder for inhalation, 60 doses in a Multidisc inhaler. 1 dose of Seretide contains salmeterol 50 mcg, fluticasone propionate 100 mcg; 250 mcg and 500 mcg. The initial dose of Seretide is determined based on the dose of fluticasone propionate. The initial dose of Seretide should then be gradually reduced to the minimum effective dose. The daily dose of fluticasone propionate is 100, 250 or 500 mcg in two doses.
- Foradil Combi (combined anti-asthma drug for inhalation use). Dosage regimen: intended for inhalation only. The package contains 60 formoterol capsules and 60 budesonide capsules + aerolyzer. When switching from oral to inhaled corticosteroids or when reducing the dose of oral corticosteroids, budesonide can be prescribed at a dose of 1600 mcg/day in 2-4 doses.
From the patients:
- late appeal,
- self-medication, especially uncontrolled use of bronchodilators, which is one of the main causes of mortality in asthma,
- underestimation of the severity of the condition,
- fear of treatment with corticosteroid drugs,
- failure to appear for follow-up examinations with a doctor, reluctance to participate in educational programs.
As you can see, the guilt of doctors and patients coincides on many points.
Asthma can occur at any age, most often after a respiratory tract infection. In most cases, the development of asthma attacks is preceded for several years by allergic rhinitis, conjunctivitis, and nonproductive cough. The frequency of attacks depends on the severity of the disease, but I would like to especially emphasize that asthma of any severity requires examination and treatment. Like any chronic disease, asthma requires adequate treatment during exacerbation and prevention during remission.
Medical standards for diagnosis and treatment of patients with bronchial asthma