Hemoglobin in newborns is never stable until the age of 12 months. The highest indicator remains in the first 7 days of life - 145-215 g/l, by the year it decreases to 100-180 g/l.
Downward deviations will be considered an alarming sign if they are 20-30 g/l. With such blood count indicators, doctors recommend carrying out a number of therapeutic measures, including taking specific medications - Maltofer, Actifferin and others.
Children who are bottle-fed should receive complementary foods on time, eat adapted formulas and not receive whole cow's milk until the age of 9 months.
Why is it important to monitor hemoglobin in newborns?
In newborns, the level of hemoglobin will allow doctors to judge the maturity of the child - whether he was born fully formed or premature. Hemoglobin production begins at the earliest stage of fetal development. At first it is fetal hemoglobin, then it is replaced by fetal hemoglobin - by about 6-7 weeks of pregnancy, and by the time the child is born, “adult” hemoglobin is already present.
Three types of element are present in the blood of newborns, but a larger percentage is fetal. Literally within a few weeks it is completely replaced by an “adult”.
Norm by day to month
It is almost impossible to indicate the norm of hemoglobin in infants - this indicator fluctuates even within one day, so for the first two weeks doctors are guided by days:
- 1-3 days after birth – 145-225 g/l;
- 4-7 days of a newborn’s life – 135-215 g/l;
- 8-14 days after birth – 125-205 g/l;
- 15-30 days – 100-180 g/l.
Doctors emphasize that the lower and upper limits of the indicators are not clear limits for the norm; small deviations in both directions are quite acceptable, because the period of adaptation of a newborn is always difficult for his body. If the indicators deviate from the norm by 20-30 g/l, then the pediatrician may prescribe additional examinations for the newborn to identify the cause.
Normal hemoglobin level in infants and newborns
The hemoglobin level in newborns is increased during the first few days after birth. Its content in the blood can be 145−230 g/l. And this significantly exceeds the norm for older infants. And all because of the active breakdown of red blood cells in a newborn baby and the rapid formation of new ones, which contain the hemoglobin of an adult.
Fetal hemoglobin can remain in the blood of a newborn for several weeks. At the same time, its amount gradually decreases, and the amount of an adult increases. The dynamics of the decrease in hemoglobin content in children’s blood is as follows:
- At the age of 1 to 4 days, there is from 140 to 230 g/l of hemoglobin in the blood.
- In 1 week - 135 - 215.
- At 2 weeks - 125 - 205.
- At 1 month - 115 - 165.
- At 2 months - 105 - 125.
- In the period from 3 months to half a year - 100 - 135.
- At 6 - 12 months - 100-140.
But in premature babies, anemia can often be observed , that is, a low level of hemoglobin.
This may be caused by a deficiency of substances necessary for normal synthesis, disruption of the normal functioning of blood cells by the fetal liver, and then by the red bone marrow of the newborn. The development of a premature baby can be judged by the level of fetal hemoglobin . There are cases when a newborn is given donor blood. Low hemoglobin in a newborn may be a consequence of blood transfusion, when fetal blood enters the mother's blood during intrauterine development.
If twins develop inside the mother, the blood of one can enter the blood of the other. In this case, one child may have anemia, and the second may have an increased hemoglobin level. Fetal hemoglobin is completely replaced by adult hemoglobin by 12 months. An increased hemoglobin level can occur with leukemia - the formation of immature blood cells, an embryonic type of hematopoiesis.
Norm in indicators by month for children
After the first month, the child is still in a period of adaptation, especially since his active development begins - the hemoglobin level is not yet stable, but children have conditional norms for this indicator by month:
- in newborns at 2 months – 90-140 g/l;
- the norm for infants at 3 months is 95-135 g/l, and the figure practically does not change until the age of 6 months;
- 6-12 months – 110-140 g/l.
Often, in children, the body’s hemoglobin norm is “not respected,” but parents should not panic - a slight decrease or increase in it does not indicate the development of pathology. Doctors recommend simply monitoring the baby’s behavior so as not to miss excessive drowsiness, seemingly causeless whims, increased body temperature and other alarming signs.
What can premature babies have?
The difference between premature babies is that the fetal hemoglobin in their blood simply does not have time to change to “adult” hemoglobin before birth. Therefore, neonatal anemia for those born before 32 gestational weeks is not considered a critical deviation. Normalization of the indicators of this element in the blood occurs only in the 6th week of actual life, and the complete restoration of hemoglobin levels lasts throughout the first year.
In premature babies, the hemoglobin level can be 120-170 g/l - this is a low content of red cells, which provokes hypoxia, insufficient oxygen supply to the tissues of organs and systems. Tests for hemoglobin in infants who were born earlier than expected are carried out regularly - at least once every three days. Even minor deviations in the direction of decreasing levels may indicate the development of complex pathologies.
How is the analysis taken?
Blood for general clinical analysis is taken from capillaries or from a vein. In pediatrics, preference is given to the first method, because it is much easier to implement. But there is a problem - capillary blood coagulates very quickly, tiny clots form, which can distort the result.
In newborns, blood is taken from a finger or heel; venous sampling can be prescribed only if the neonatologist has doubts about obtaining informative, truthful results.
Low hemoglobin in a breastfed infant: the development of anemia and its symptoms
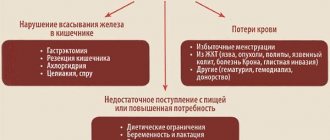
Low hemoglobin levels in breastfeeding infants may be associated with:
- lack of iron, which leads to low hemoglobin synthesis;
- acute blood loss;
- a blood disease that results in excessive destruction of red blood cells.
Such pathological causes lead to a critical decrease in blood element parameters and require drug treatment. But low hemoglobin can also be due to:
- maternal malnutrition;
- tying the umbilical cord too early or too late during childbirth.
The same indicator may indicate the development of thallasemia, bone marrow diseases, intestinal polyposis, kidney pathologies, Meckel's diverticulum.
Regardless of what is the true cause of low hemoglobin in newborns, the symptoms of a blood count disorder will be the same:
- excessive sweating, even when the baby is in a cool room;
- low appetite or its complete absence;
- sleep disturbance, regardless of adherence to the regime;
- the formation of small cracks in the corners of the mouth;
- pronounced pallor of the skin;
- excessive dryness of the dermis;
- general lethargy, frequent whims for no apparent reason, anxiety.
Low hemoglobin in infants. Causes
The first time after the birth of a child is filled with many joyful events and pleasant troubles. But at the same time, the number of reasons for concern is growing - colic, teething, fever, rashes and other health problems of the baby puzzle young parents. But the listed diseases are immediately visible to the naked eye, so they can be quickly cured and prevented from developing.
In addition to these diseases, there are more insidious ones. They may not manifest external symptoms at all, or these symptoms are not immediately noticeable to the parent’s eye and only a doctor can recognize them. Moms and dads can notice any manifestations of the disease only when it has already gone far enough.
One of these diseases is low hemoglobin in infants. It can also be reduced in adults, but for them it is less dangerous (although, of course, not harmless).
This is a blood disease. Another, more scientific name is anemia. Characterized by a decrease in red cells (erythrocytes) in the blood. These bodies are responsible for supplying the blood with oxygen. Oxygen, in turn, gives us energy.
Normal limits
Each age has its own norm. For example, in babies under one year old (especially those who are breastfed), the norm may exceed 100 g/l. At first glance, this is not a low figure at all, but this is the number that is the norm, and you need to make sure that the figure does not fall. Because low hemoglobin in a baby can be difficult to increase, it is easier to maintain the norm and not let it “fall” initially.
So, for example, in the first days of a baby’s life, a good indicator is from 145 to 225. In the first week, the number should “fall” a little - 135-215, after two weeks - another decrease - 125-205, in the first month of life - 100-180 , the second - 90-140, at 3 months the infant’s hemoglobin is even lower, and this figure persists until about six months - 95-135, up to a year - 100-140. A small error is acceptable. But it’s better to talk to your pediatrician about the limits of this error - he will tell you when you should be wary and start treating your child.
Causes
Nothing happens for nothing. Especially when certain processes relate to health. Moreover, the health of the baby.
Why does a baby have low hemoglobin? This is influenced by circumstances both dependent and independent of the baby’s mother and her behavior during pregnancy and lactation. Dependent factors include
- unhealthy diet;
- rare walks in the fresh air
And to the independent ones
— hereditary diseases;
— previous operations;
— pathologies of fetal development
How a child develops in the womb directly depends on the expectant mother: does she have bad habits, does she eat properly, does she go for walks regularly, does she have any infectious or other diseases... Of course, there are exceptions: the mother throughout her entire life during pregnancy she smokes, drinks alcohol or eats fast food, and she gives birth to an absolutely healthy toddler, to whom no disease “sticks” throughout her life. But this is one case out of a hundred. And to hope that this single case is yours is, to say the least, unreasonable. No, we do not teach you how to live correctly. We are simply informing you.

The reasons for low hemoglobin in infants do not end there. In order for the blood to be sufficiently enriched with oxygen and its overall composition not to deviate from the norm, the body needs iron. The reserve of this element, which is present in the body of a newborn by default, is only enough for six months. Then it is necessary to maintain iron levels through proper nutrition of the mother (and, as a result, breastfeeding).
If you are feeding your baby formula, choose one that contains iron. E. O. Komarovsky, a well-known pediatrician, together with other doctors, actively advocates the introduction of iron into the diet - it will quickly increase low hemoglobin in infants.
A little later (after six months), you can slowly introduce your son or daughter to regular food through complementary foods (meat, vegetable and fruit purees, cereals, juices).

Why else could a very young child have low hemoglobin? For example, as you grow, as your weight changes, changes may occur in your body that require more energy than is produced. Accordingly, the necessary elements leave the body faster, and their supply is not replenished. This is where all the causes of low hemoglobin in infants originate.
What do you need?
What should you do to ensure that the problem of low hemoglobin in your baby never affects you? The conditions under which hemoglobin will be formed and produced in normal quantities are much simpler than it seems:
- breastfeed your baby for as long as possible;
— when breastfeeding, the mother must eat a balanced diet, when artificially feeding, she must be able to choose the right mixture with the most natural composition;
- monitor the condition of the baby’s gastrointestinal tract;
- neither the mother nor the child should have problems with the circulatory system
Symptoms
Is low hemoglobin as dangerous as they say? And why is it dangerous? The symptoms, of course, are not fatal, but should make parents wary:
- pale skin (especially the face and palms);
- weakness;
- lethargy;
- dizziness;
- bluish discoloration of the skin under the eyes;
- increased heart rate
All this looks like normal malaise, low blood pressure, fatigue. But aren't these symptoms a reason to take action?
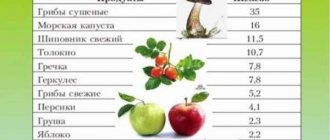
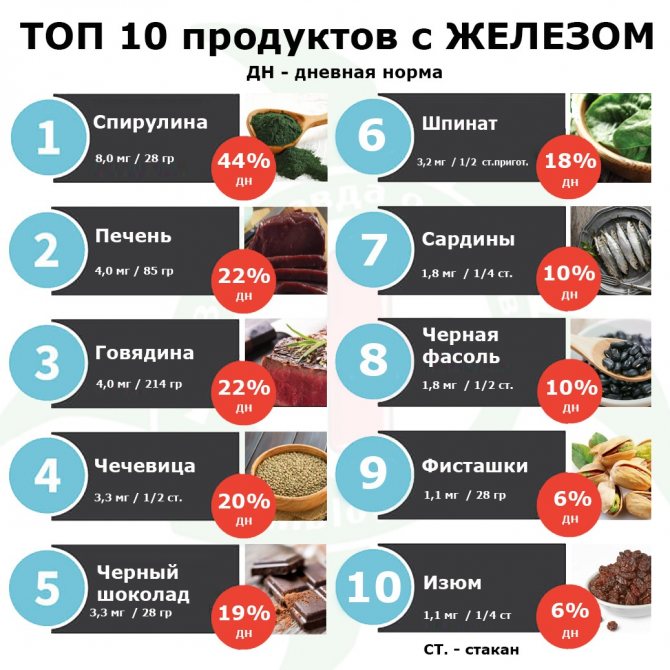
Of course, no one wants to take medications again. And in the case of children, it is better to resort to medication only in extreme cases. You can try to enrich your body with iron through food. Such as beef, apples, buckwheat, liver, beets, carrots. They can be given to the child in the form of purees or juices (depending on chewing ability).
Some facts
What is hemoglobin? Its basis is the protein globin. There is also an iron-containing component. Anemia often affects not only children, but also pregnant women - literally every other day.
Upon reaching six months of age, it is necessary to donate blood for analysis. Six months is a turning point for an infant when indicators can change dramatically. In addition, a blood test is simply a check of its composition, which, you see, is never superfluous.
And while the baby is breastfed, doctors may advise you to take folic acid (it is also prescribed during pregnancy to prevent various abnormalities in the fetus) and B vitamins.
Children's health problems make parents seriously worry. What can help prevent low blood iron? Let's repeat:
- proper nutrition;
- walks in the open air;
- any activity (outdoor games, walking, swimming...);
— timely introduction of complementary foods. There is no need to rush into this, but you also shouldn’t be afraid to introduce your son or daughter to adult food - someday you will still need to do it;
— consultations with a pediatrician who will help to detect an insidious disease in time and prescribe medications if necessary.
Take care of your health and it will not let you down!
Folic acid for infants with low hemoglobin

Folic acid, or vitamin B9, is prescribed to infants in 20% of cases of low hemoglobin. The dosage for an infant aged 3 months is ¼ tablet 2 times a day. At such a young age, drugs in tablet form are given as follows:
- the prescribed dose is turned into a fine powder - you can knead it with a spoon or roll it with a rolling pin under a napkin;
- dilute the resulting form of the drug in a small amount of warm water - not hot, so as not to deprive the medicine of its medicinal properties;
- Give the baby something to drink from a spoon, syringe or bottle.
Many mothers are sure that when they take folic acid, they pass it on to their baby through breast milk. Pediatricians warn that such treatment will clearly not be enough: even if a woman consumes 1000 mcg of the vitamin in question, a maximum of 50 mcg will enter the baby’s body.
How to increase hemoglobin in a breastfed baby
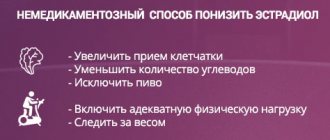
It is possible to raise the hemoglobin of a breastfed baby not only with folic acid; there are a number of measures, the regular implementation of which will restore the blood formula to normal values: daily routine, mother’s diet, and in some cases, the inclusion of medications.
Correct daily routine

The baby should take a full walk: the more time spent in the fresh air, and even under the sun’s rays, the faster the hemoglobin level increases. Additionally, you need to build the baby’s daily routine so that he:
- got enough sleep - both night and daytime sleep are important, going to bed at the same time;
- fully developed physically - you need to turn him over, literally force him to lift his body from the horizontal plane, imitate crawling, do gymnastics and massage with the child;
- was not in a state of stress - if the child does not perceive strangers, then for a while you need to refuse visiting and inviting guests, and avoid loud sounds.
It is important to strengthen the baby's immune system: bathing in warm and cool water, sleeping in the fresh air or indoors with open windows/doors.
Mom's nutrition
When breastfeeding, foods that should be included in the mother’s diet will help increase the child’s hemoglobin level:
- chicken, veal, rabbit;
- liver and tongue, other offal;
- buckwheat and oatmeal porridge;
- dried apricots, pomegranates, green apples such as Simirenko;
- fresh herbs, spinach, young nettle, broccoli.
You just need to carefully monitor the baby’s condition, because he may develop an allergy to any of the listed products - it should be immediately removed from the nursing woman’s menu. Almost all of them can be used for complementary feeding of a baby, so if the level of hemoglobin is constantly low, you should not delay the moment of its introduction.
Vitamin C also helps to absorb iron from breast milk, so a nursing woman can and should consume black currants, citrus fruits, and kiwi, but only in limited quantities to avoid the development of allergies in the child.
Pharmacy drugs

If the decrease in hemoglobin in a baby is critical, or it is not possible to return to normal levels within 1 month of following the above recommendations, then the pediatrician will prescribe the following medications to the child:
- Maltofer;
- Ferrum Lek;
- Actifferin;
- Ferronal 35.
A nursing mother can take complex vitamins and folic acid. But any medications are prescribed only by specialists and taken in strictly prescribed dosages.
Parents should understand that the increase in hemoglobin in infants occurs extremely slowly, sometimes it takes 1.5-2 months.
How to increase hemoglobin in a baby who has already been introduced to complementary foods
If the child has already been introduced to complete complementary feeding (preferably no earlier than six months), then hemoglobin can be increased by adding the iron-containing products listed above to his diet. If your baby is introduced to complementary foods before six months, the absorption of iron from breast milk will become worse. It has also been noted that anemia is common in children who are fed cow's and goat's milk. This is due to the fact that these products do not contain enough microelements necessary for hematopoiesis. In addition, the baby’s body is often unable to break down cow protein.

Be sure to include berries in your child’s diet (even frozen or dried, if it’s winter): blueberries, strawberries, black currants, cranberries.
How to increase low hemoglobin in a bottle-fed baby

If low hemoglobin is diagnosed in a bottle-fed infant, then all of the above measures will be appropriate to normalize the indicators.
“Artificial babies” need to carefully select formulas for feeding: they must be adapted, enriched with iron or folic acid. But such feeding can only be started after consultation with a doctor, since an excess of certain substances leads to disruption of the gastrointestinal tract.
It is strictly forbidden to give bottle-fed infants whole cow's milk - it negatively affects the delicate intestinal mucosa and causes microbleeding. And regular blood loss, even in minimal quantities, will further reduce hemoglobin levels.
In this condition, doctors recommend that bottle-fed children introduce complementary foods earlier - vegetable purees from broccoli, cauliflower, fruit juices and purees, dairy-free buckwheat or oatmeal porridge, and meat automatically saturate the baby’s body with the required amount of iron.
Low hemoglobin in infants
In an infant, low hemoglobin is observed with anemia and anemia. Anemia can be of the following types:
- Posthemorrhagic . Very rare in infants. Occurs when blood loss occurs after injury or surgery.
- Dyshematopoietic . It rarely happens in infants. It can be caused by a disorder of hematopoiesis in the bone red marrow.
- Hemolytic . Caused by pathological increased breakdown of red blood cells. Occurs after taking certain medications for a long time, during intoxication with hemolytic poisons and salts of heavy metals, with incompatibility of the blood of the fetus and mother, in premature babies.
- Folate deficiency . Lack of vitamin B9 and folic acid, necessary for the synthesis of RNA, DNA, and nucleic acids.
- B12-deficient . Occurs when a woman has hypovitaminosis during pregnancy and breastfeeding. Large amounts of vitamin C block the action of vitamin B12.
- Iron deficiency . The cause is iron deficiency, which is necessary for the synthesis of heme and hemoglobin. During pregnancy, a woman's body becomes deficient in iron. It is because of this that a newborn may experience this type of anemia.
In rare cases, infants may experience hemopathy - the formation of pathological hemoglobin with an altered protein part of the molecule. This anemia may be caused by hereditary factors or mutations in the fetus (in rare cases).
Symptoms that indicate that a baby has anemia:
- Bowel problems (diarrhea or constipation).
- Possible heart murmurs.
- Jaundice is observed in hemolytic anemia.
- Decreased tactile sensitivity.
- Drowsiness.
- Weakness.
- Pallor.
A child suffering from anemia is weakened and may become infected with bacteria or viruses more often than a healthy child. The hemoglobin level may drop to 70 g/l.
Prevention of anemia in children
The first positive results of treatment for anemia in newborns will be noticeable after 2 weeks, but you cannot stop all actions - a certain amount of hemoglobin must accumulate in the child’s body, and his immune system must become stronger. In order to prevent the development of anemia in infants in the future, you need to adhere to the following recommendations for prevention from doctors:
- provide the baby’s body with physical activity and often walk with the child in the fresh air;
- if the child is breastfed, then the mother’s menu needs to be adjusted, including reducing the amount of tea consumed - the drink interferes with the absorption of iron;
- an “artificial” child needs to select adapted formulas and only together with an observing pediatrician;
- Complementary foods should be introduced in a timely manner and in the amount permitted by the doctor.
A decrease in hemoglobin in infants is rarely critical; doctors must see deviations from the norm of 20-30 g/l in blood tests to begin treatment. Regardless of whether the child is breastfed or bottle-fed, a slight decrease in hemoglobin can be corrected by physical activity, walks in the fresh air and food of the mother or the baby himself. Medicines are prescribed only in the absence of positive dynamics of therapy and a critically low hemoglobin level.
How else can you increase hemoglobin in an infant?
An important factor in the treatment of anemia in infants is the normalization of the daily routine. Provide your baby with adequate sleep, long walks in the fresh air (1.5–2 hours a day), the opportunity to move a lot, and strengthen him. These factors also play a significant role in increasing hemoglobin.
Among some naturopaths there is still an opinion that the child’s hemoglobin is influenced by the emotional state of the mother. According to this theory, if a mother is full of fears, then these fears block the flow of life (which is equivalent to the flow of blood) both through her channels and through the channels of the child. If there is no place for joy and a smile in her life, but there is a lot of anger and resentment, then changing her diet will most likely not change anything. If you find a resource of inner joy in yourself, stop “spoiling” your blood, stop sorting things out with your family, then this is how you can increase your baby’s hemoglobin.