Editor
Maria Bogatyreva
Doctor of the highest category, teacher
Since the discovery of X-rays (X-rays), they have been actively introduced into all areas of medicine, and phthisiology was no exception. Since the lungs of a tuberculosis patient have characteristic features, X-ray methods began to be used for diagnosis, monitoring the dynamics of the process and prevention.
We urge you not to self-medicate and consult a doctor in a timely manner! Please do not use the described treatment regimens without consulting a doctor - it is dangerous to your health!
List of visualization research methods
to diagnose tuberculosis :
- fluorography;
- radiography;
- computed tomography (CT).
Tuberculosis is a disease that is often not accompanied by clinical symptoms at its onset. For this reason, pathological changes are often an incidental finding during chest radiography. Every doctor and x-ray technician should know what the lungs look like with tuberculosis on an x-ray so as not to miss this dangerous disease.
A separate article has been written about the diagnosis and differential diagnosis of tuberculosis.
Photo examples
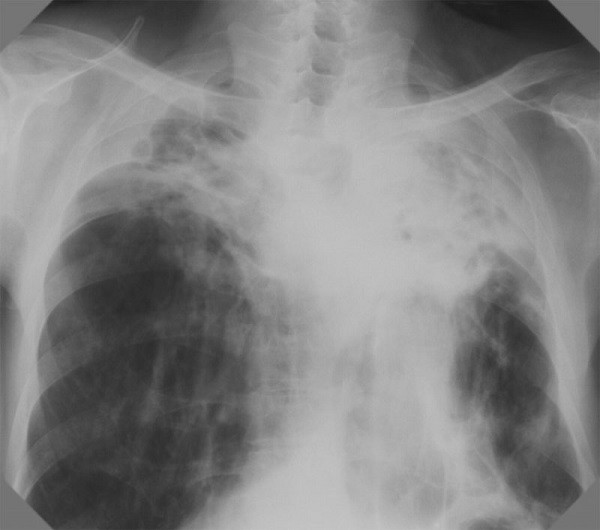
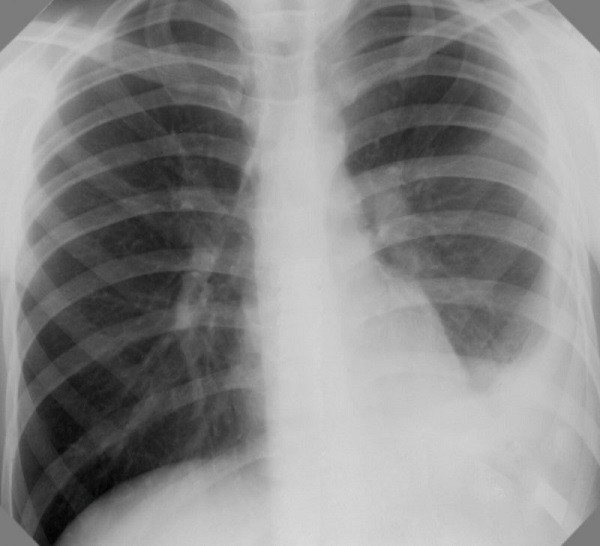
For comparison, you can see x-rays of the chest before and after the disease:
Normal chest and lung x-ray. The lung fields are clean, the roots of the lungs are without any features.
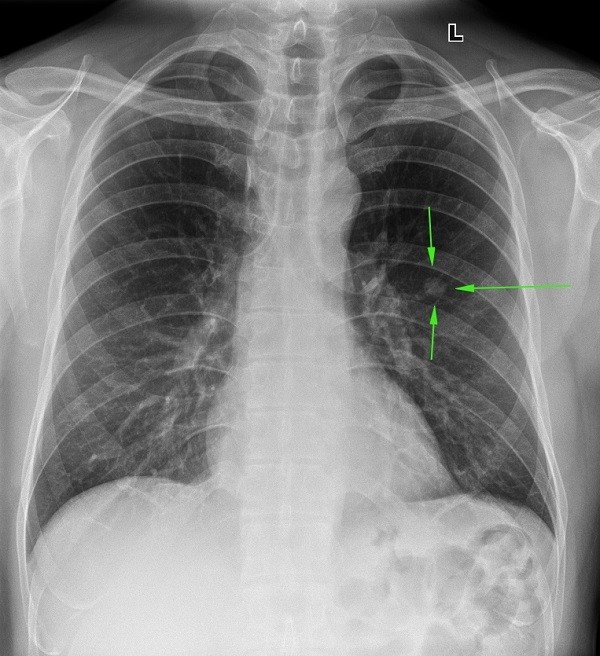
Focal tuberculosis at the initial stage. A small focal change in the left lung, 1-1.5 cm in diameter, with an uneven and unclear contour, the structure is heterogeneous.
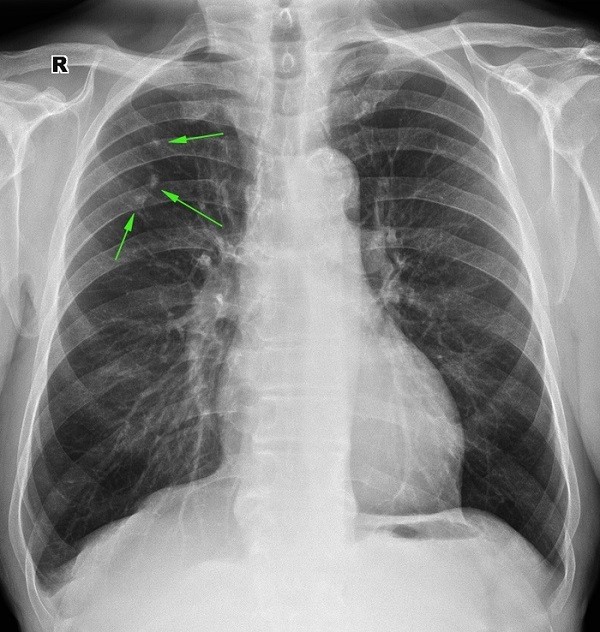
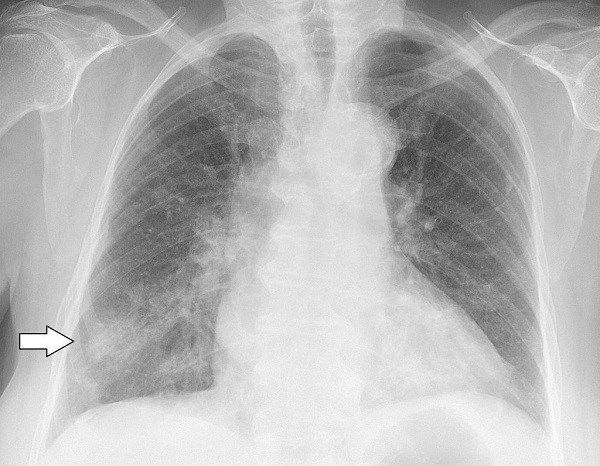
Residual calcifications after tuberculosis (52 years ago). Multiple rounded shadows in the right lung, strong intensity with a clear edge, homogeneous.
People with pulmonary tuberculosis may have a varied X-ray picture, which is associated with the variety of forms of the disease and stages of its course.
Signs and symptoms of pulmonary tuberculosis
The main symptom of pulmonary tuberculosis in adults is:
- Cough - from a slight cough to a cough with sputum, sometimes mixed with blood. In smokers with illness, the nature of their cough changes. A cough indicates damage to the bronchi.
- When the pleura is affected, chest pain and shortness of breath appear.
- When advanced forms are identified, all intoxication complaints, a sharp decrease in body weight, cachexia, anemia, and respiratory failure are evident.
Rice. 2. The main symptom of pulmonary tuberculosis is cough. When coughing, mycobacteria are released into the external environment.
Fluorography
Fluorography is a method of x-ray examination that involves photographing an image from a fluorescent screen that appears on it after X-rays pass through the human body. There are several types of techniques:
- small frame;
- large-frame;
- electronic.
Small- and large-frame fluorography may not show tuberculosis if changes in the lungs are small in size or not clear enough. This is its main drawback, due to which it is impossible to make a diagnosis based on this study. Currently, only electron fluorography is relevant, in which the above disadvantages are eliminated.
It is used to detect tuberculosis during mass preventive studies. Modern fluorography reveals pulmonary tuberculosis thanks to the high quality of the resulting image, the ability to dynamically change the contrast and computer image editing. These features allow you to find the smallest changes.
Here are some examples of what tuberculosis looks like in a fluorography image:

Small-frame fluorogram.
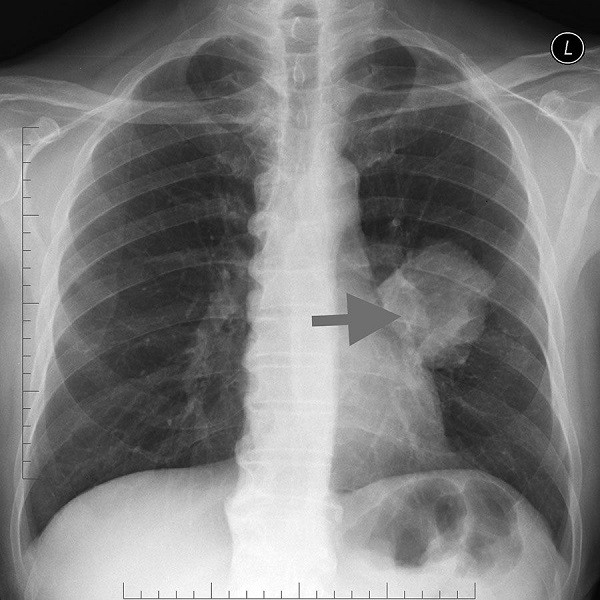
Electronic fluorography. A large focal shadow in the region of the root of the left lung, heterogeneous in structure, has a clear contour.
Radiography
Chest X-ray is a research method that allows you to assess the condition of the bone skeleton of the chest and the organs contained in it. The image is obtained in real scale by projecting the shadows of body parts onto x-ray film. Electronic radiography, which allows image editing for better visualization, is becoming increasingly popular.
There are several mandatory rules for performing chest x-rays:
- the photograph must be taken in two projections (frontal and lateral);
- the frame should capture the apexes of the lungs and costophrenic sinuses.
Following these simple rules will prevent diagnostic errors and allow tuberculosis to be visualized on an x-ray.
The correct description of the radiograph of the lungs is of great importance; for this you need to adhere to the developed algorithm:
- assessing the quality and completeness of the image;
- condition of bone structures;
- comparison of pulmonary fields by pattern, shape;
- study of pathological changes (if any);
- assessment of the condition of the roots of the lungs;
- mediastinal shadow.
If the algorithm is followed, the analysis is as complete and consistent as possible, however, even if all the rules are followed, it is not always clear what pulmonary tuberculosis looks like on an X-ray. Such cases are rare, but they do occur. It is important to remember this and not rely entirely on this diagnostic method, especially if there are clinical signs of the disease.
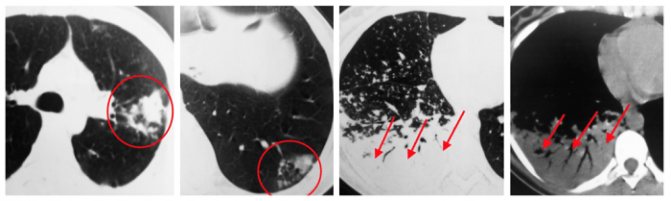
There are many types of tuberculosis, and each of them has its own special x-ray picture:
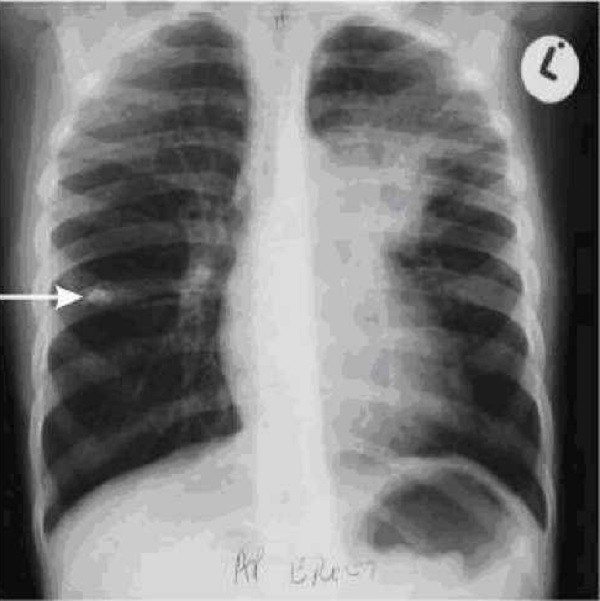
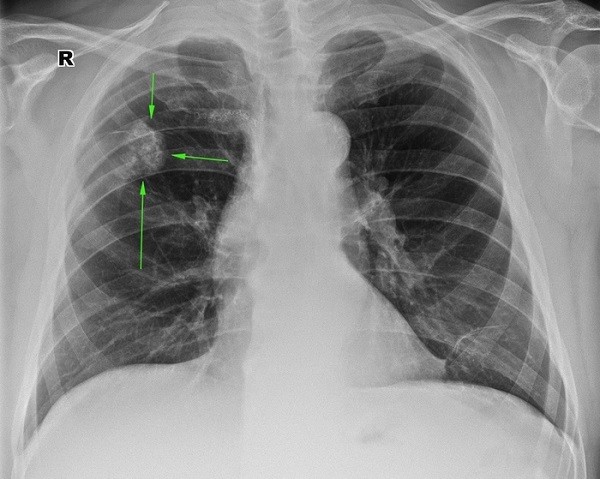
Primary tuberculosis complex. A dense focal shadow in the right lung, a “path to the root” is observed. The pulmonary pattern is enhanced.
This x-ray shows tuberculosis of the hilar lymph nodes. Homogeneous focal shadows in the roots of both lungs, strong intensity, with a clear edge.

Disseminated lung disease. Multiple lesions in the upper lobes of the right and left lungs. The changes affect the roots and are accompanied by infiltration of lung tissue in the affected area.
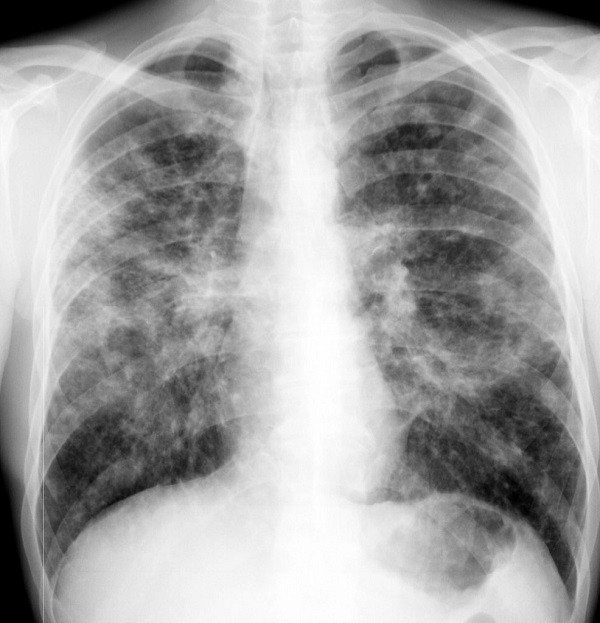
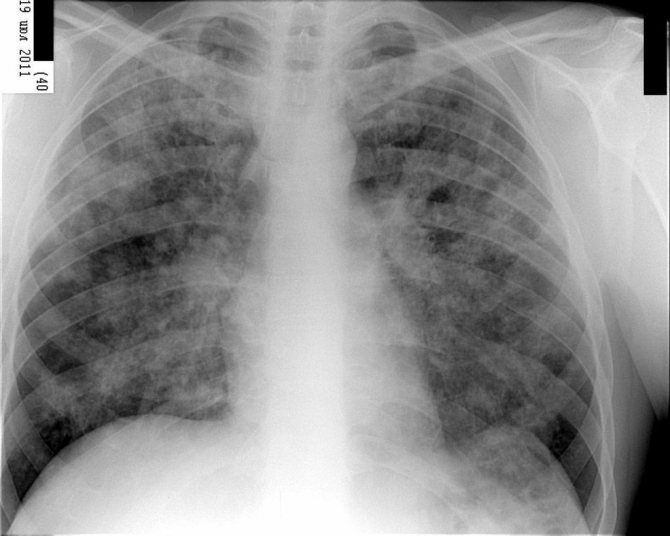
Miliary tuberculosis. A huge number of small millet-like foci in all lung fields, with signs of fusion.
Focal tuberculosis. A small focal change in the left lung, 1-1.5 cm in size, with an uneven and unclear contour, the structure is heterogeneous.
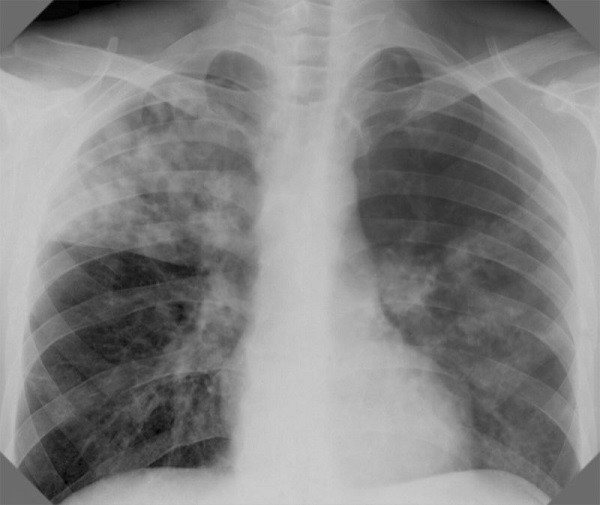
Infiltrative TBC of the right lung. Severe infiltration of the upper lobe of the right lung with involvement of the root, as well as the lower lobe of the left lung. The pulmonary pattern is enhanced.
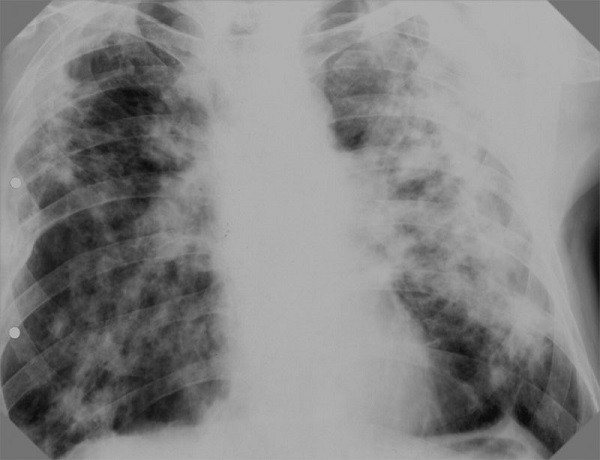
Caseous pneumonia. Severe disseminated infiltration of both lungs.
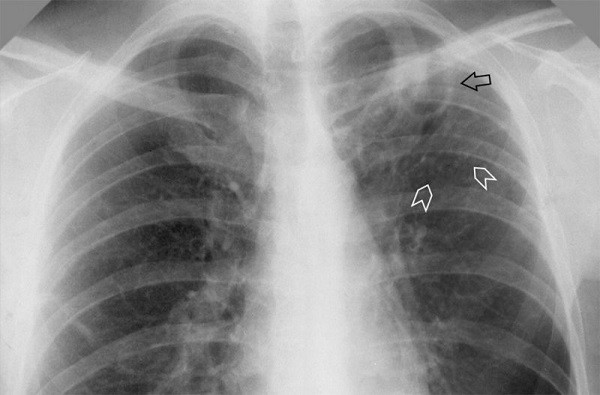
Tuberculoma of the right lung. Heterogeneous large-focal formation in the right lung with an unclear double contour.
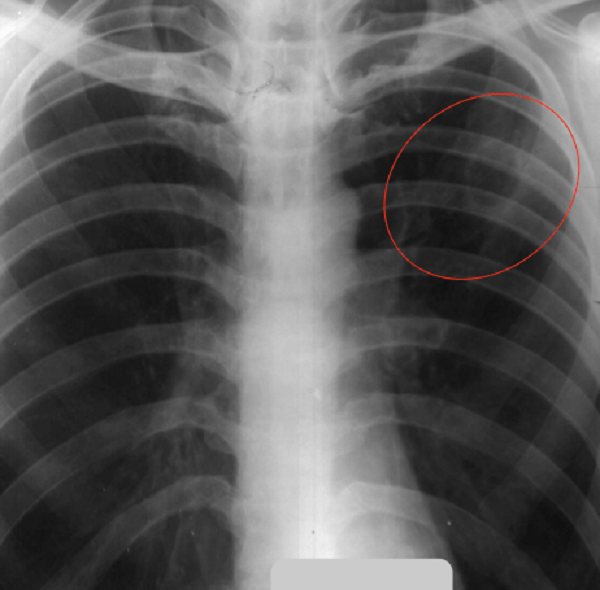
Cavernous tuberculosis of the left lung. Ring-shaped shadow in the upper lobe of the left lung (indicates the presence of a decay cavity).
X-ray of fibrous-cavernous tuberculosis. A ring-shaped shadow at the apex of the left lung with a clear, dense contour. Finely focal seeding of the left lung.
Cirrhotic pulmonary tuberculosis. Total darkening of the left and upper lobes of the right lungs (indicates severe sclerosis of the lung tissue).
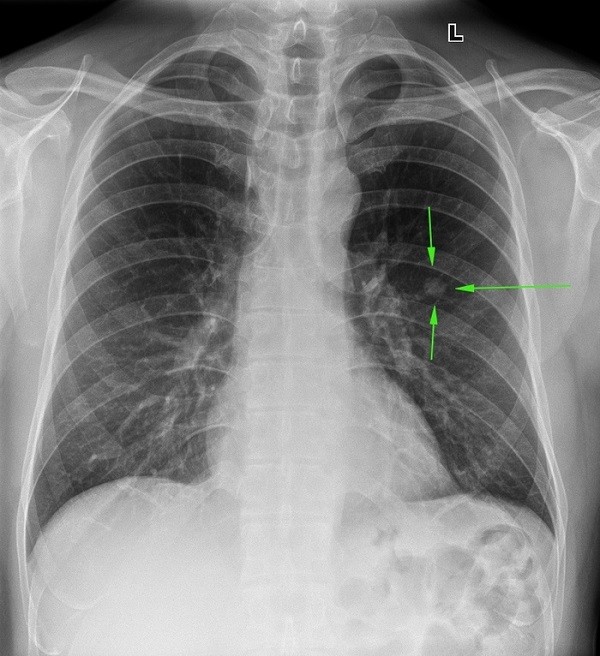
Left-sided exudative tuberculous pleurisy. Darkening in the lower parts of the left half of the chest. The pulmonary pattern on the left is weakened.
An X-ray of the lungs may not show bronchial tuberculosis in isolation, since it occurs only in conjunction with other forms. Infiltration along the large bronchus of the right lung. The pulmonary pattern is strengthened, the root is deformed.
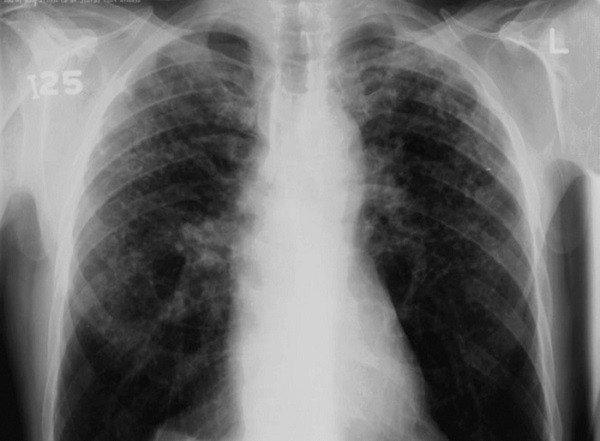
Silicotuberculosis. Disseminated infiltration of both lungs.
An X-ray examination is mandatory if a patient is suspected of having tuberculosis; it corresponds to the GPP level of evidence, i.e. current clinical practice.
We also recommend reading the article about tests for tuberculosis.
Pulmonary tuberculosis
Tuberculosis is an infectious disease caused by several species of acid-fast mycobacteria (genus Mycobacterium) (obsolete name - Koch bacillus). The outdated name for pulmonary tuberculosis is consumption (from the word to waste away), in ancient Russia it was called dry.
Pulmonary tuberculosis is an infectious disease characterized by the formation of foci of specific inflammation in the affected tissues and a pronounced general reaction of the body. In many economically developed countries, in particular in Russia, the incidence of tuberculosis and mortality from it have significantly decreased. According to WHO information, about 2 billion people, a third of the total population of the Earth, are infected with tuberculosis. Currently, 9 million people worldwide fall ill with tuberculosis every year, of which 3 million die from its complications. It has been noted that the incidence of tuberculosis depends on unfavorable conditions (prison), as well as on the individual characteristics of the human body (for example, blood type). There are several factors that cause a person’s increased susceptibility to tuberculosis; AIDS has become one of the most significant in the world.
Pathogens of tuberculosis - tuberculosis in humans is caused by a conditionally isolated complex of M. tuberculosis, including Mycobacterium tuberculosis (human species), Mycobacterium bovis (bovine species), Mycobacterium africanum, Mycobacterium bovis BCG (BCG strain), Mycobacterium microti, Mycobacterium canetti. The main species characteristic of Mycobacterium tuberculosis (MBT) is pathogenicity, which manifests itself in virulence. Virulence can vary significantly depending on environmental factors and manifest itself differently depending on the state of the microorganism that is subject to bacterial aggression. Tuberculosis in humans most often occurs when infected with human and bovine species of the pathogen. Avian tuberculosis is also noted, which occurs mainly in immunodeficient carriers. In organs affected by tuberculosis (lungs, lymph nodes, skin, bones, kidneys, intestines, etc.) a specific “cold” tuberculous inflammation develops, which is predominantly granulomatous in nature and leads to the formation of multiple tubercles with a tendency to disintegrate.
Primary infection with Mycobacterium tuberculosis and latent course of tuberculosis infection. Primary infection of humans with MBT usually occurs through the aerogenous route. Other routes of penetration - nutritional, contact and transplacental - are much less common. The respiratory system is protected from the penetration of mycobacteria by mucociliary clearance (secretion of mucus by goblet cells of the respiratory tract). Violation of mucociliary clearance during acute and chronic inflammation of the upper respiratory tract, trachea and large bronchi, as well as under the influence of toxic substances, makes it possible for mycobacteria to penetrate into the bronchioles and alveoli, after which increases the likelihood of infection and tuberculosis disease significantly.
Mycobacteria are retained in organs with the most developed microvasculature (lungs, lymph nodes, renal cortex, epiphyses and metaphyses of tubular bones, ampullar-fimbryonic sections of the fallopian tubes, uveal tract of the eye). Since the pathogen continues to multiply, and immunity has not yet formed, the population of the pathogen increases significantly. When immunity is weakened, there is a threat of activation of the remaining MBT population and tuberculosis disease. Acquired immunity to MBT decreases with AIDS, diabetes, peptic ulcers, alcohol abuse and long-term drug use, as well as with fasting, stressful situations, pregnancy, treatment with hormones or immunosuppressants. In general, the risk of developing tuberculosis in a newly infected person is about 8% in the first 2 years after infection, gradually decreasing in subsequent years.
Clinic. Pulmonary tuberculosis can be asymptomatic or low-symptomatic for a long time and discovered by chance during fluorography or a chest x-ray. The fact of contamination of the body with tuberculous mycobacteria and the formation of specific immunological hyperreactivity can also be detected by performing tuberculin tests. In cases where tuberculosis manifests itself clinically, usually the very first symptoms are nonspecific manifestations of intoxication: weakness, pallor, increased fatigue, lethargy, apathy, low-grade fever (about 37 ° C, rarely above 38 °), sweating, especially disturbing the patient at night, weight loss Often generalized or limited to any group of lymph nodes, lymphadenopathy (an increase in the size of the lymph nodes) is detected. Sometimes it is possible to identify a specific lesion of the lymph nodes - “cold” inflammation. In the blood of tuberculosis patients, laboratory tests often reveal anemia (decrease in the number of red blood cells and hemoglobin content), moderate leukopenia (decrease in the number of white blood cells). Further, as the disease develops, more or less obvious symptoms appear - cough, sputum discharge, wheezing in the lungs, runny nose, sometimes difficulty breathing or chest pain (usually indicating the addition of tuberculous pleurisy), hemoptysis. As a rule (but not always), damage to the lungs is primary, and other organs are affected secondarily through hematogenous seeding.
Diagnostics. Laboratory diagnostic methods - material obtained during bronchoscopy; pleural fluid studies; biopsy of the pleura, lung; sputum microscopy; genetic methods of bacterial diagnostics (polymerase chain reaction (PCR) method, serological methods;
X-ray methods - fluoroscopy; radiography; tomography; fluorography; computed tomography.
Tracheobronchoscopy , thoracoscopy (pleuroscopy);
Transbronchial biopsy (a direct indication for its implementation is the presence of pathology in the main, lobar, segmental or subsegmental bronchi) ; transthoracic needle biopsy; p levral puncture and puncture biopsy of the pleura.
Treatment is medication; surgical treatment of pulmonary tuberculosis (removal of the affected part of the lung).
Prevention . For the purpose of prevention, the following measures are necessary:
- carrying out preventive and anti-epidemic measures adequate to the current extremely unfavorable epidemiological situation regarding tuberculosis.
- early identification of patients and allocation of funds for drug provision. This measure will also be able to reduce the incidence of illness among people who come into contact with sick people in outbreaks.
- carrying out mandatory preliminary and periodic examinations upon entry to work on livestock farms affected by bovine tuberculosis.
- increasing the allocated isolated living space for patients suffering from active tuberculosis and living in crowded apartments and dormitories.
- timely implementation (up to 30 days of life) of primary vaccination for newborn children.
Computed tomography (CT)
Computed tomography is the most informative diagnostic method in comparison with other x-ray examinations. But due to high cost and low availability, the method is not used very often.
Indications for computed tomography of the lungs for tuberculosis:
- clarification of the diagnosis;
- determining the location and volume of the lesion;
- differential diagnosis with other lung diseases;
- assessment of the dynamics of the process under the influence of therapy.
Expert opinion
Anna Sandalova
Pulmonologist, doctor of the highest category
Ask a Question
CT for this disease is performed only when necessary, in cases where other methods are ineffective or ineffective.
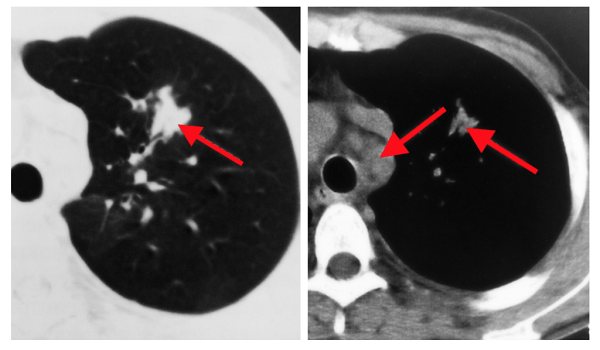
CT images for pulmonary tuberculosis look like this:
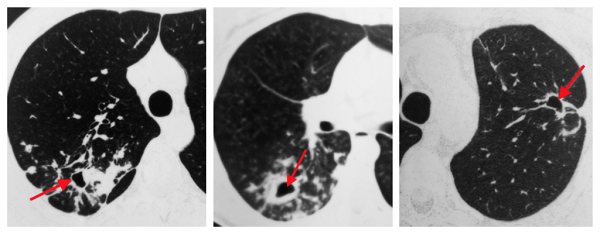
Cavernous tuberculosis. A cavity with dense thick walls is observed.
Primary tuberculosis complex. A focus of compaction of the lung tissue and enlarged lymph nodes of the mediastinum and root of the lung.
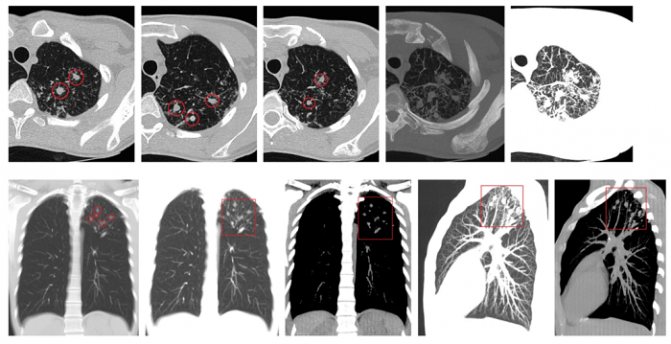
Focal tuberculosis. Small focal compactions in the upper lobe of the left lung.
Infiltrative lung damage. Focal infiltration of lung tissue. Some images show decay cavities.
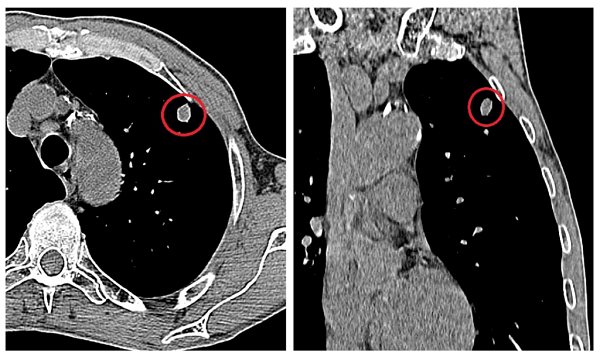
Tuberculoma. A heterogeneous formation on the periphery of the right lung, with a clear calcified contour and less dense contents.
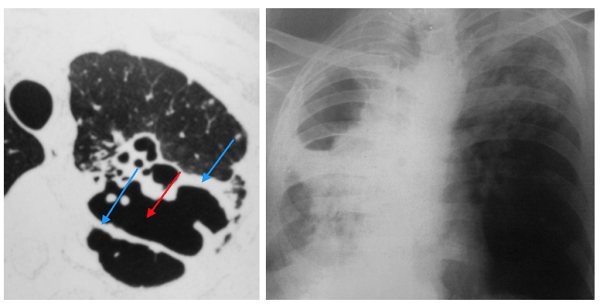
Fibrous-cavernous tuberculosis. Multiple cavities (cavities) with a thick dense contour and areas of compaction around.

Tuberculous pleurisy. The presence of fluid in the pleural cavity.
Why do they take x-rays for tuberculosis?
This disease (be it fibrous-cavernous tuberculosis or any other type of illness) is a dangerous pathology that is quite widespread. This disease means damage to almost all soft tissues, and it develops regardless of age and other factors. If the pathology was identified in the early stages, then its treatment will not be particularly difficult. As you might understand, when discussing a disease such as pulmonary tuberculosis, x-ray is implied as the main diagnostic method, because this procedure allows you to cope with the following tasks:
- This examination method can help establish or, conversely, refute the presence of the disease.
- X-ray allows you to distinguish the signs of tuberculosis from any other diseases that relate to the respiratory system. We are talking about pneumonia, various tumor lesions and other ailments.
- Fluorography allows not only the presence of pulmonary tuberculosis, but also the degree of damage to all tissues of the respiratory organs in this disease. It is also worth noting the existing differences in the nature of the diseases, because fibrous-cavernous tuberculosis has completely different lesions than any other type.
- Even with a previously made diagnosis, it is sometimes necessary to determine the location of the disease in question, as well as its prevalence.
On X-rays, pulmonary tuberculosis is visible as compactions and dark spots.
Sources and reference materials
| # | File | file size |
| 1 | Differential X-ray diagnostics of the respiratory organs and mediastinum T1 1991 | 7 MB |
| 2 | Laboratory research methods in the differential diagnosis of tuberculosis. 2006 | 849 KB |
| 3 | Algorithm laboratory. diagnosis and monitoring of treatment of drug-resistant pulmonary tuberculosis using rapid molecular methods. WHO. 2017 | 2 MB |
| 4 | Article. Pulse oscillometry in the diagnosis of obstructive ventilation disorders in patients with pulmonary tuberculosis.2019 | 269 KB |











