Body changes and new sensations for women
If we say that now mothers are enjoying their position to the fullest, we, of course, are lying.
Women at 30 weeks are very tired, every day it becomes more and more difficult for them to carry a child under their hearts. What to do? Learn to ignore difficulties and prepare yourself for the fact that the third trimester will soon end, and a meeting with your beloved baby awaits you ahead! Continue to monitor your health during the 30th week and follow all the safety measures necessary during this period. In particular, avoid resting on your back. Otherwise, you risk causing yourself compression syndrome by the uterus of the inferior vena cava, which runs along the right side of the spine. This may result in headaches, dizziness, or a feeling of shortness of breath. Another consequence of the syndrome is an increase in blood pressure in the veins of the lower extremities, as well as in the hemorrhoidal veins located under the skin near the anus, which leads, accordingly, to varicose veins of the legs and hemorrhoids. So how to sleep during pregnancy? Remember: the expectant mother can only rest on her side, preferably on the left.
Fetus. Development at 30 weeks
Fetus.
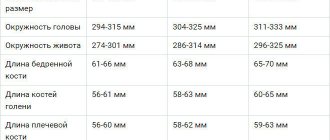
Development at the 30th week At the 30th week of pregnancy, the fetus continues to actively gain weight and height. It can weigh from 1.3 to 1.8 kg, have a body length from 36 to 40 cm. Growth rates and weight gain are individual parameters determined by genetics and the characteristics of pregnancy.
The main parameter for assessing the timeliness of fetal development at this stage is the degree of maturity of its internal organs, the constant increase in key indicators, compliance with the norms of the amount of amniotic fluid, the thickness of the uterine walls, and the maturity of the placenta. The data obtained from the ultrasound results should be assessed by a doctor.
By the 30th week, all major organs and systems have completed their development (with the exception of the pulmonary system). There is a process of maturation, mastering basic functions, and establishing teamwork.
The most striking changes during this period occur in the nervous system. Its main organ, the brain, continues to improve and is reaching the finish line of intrauterine development. The process of neuronal myelination continues (coating nerve cells with myelin to protect and increase the speed of information transfer). New convolutions form and deepen along the entire surface of the cerebral cortex.
In the centers of the brain, the number of neural connections increases, the processes of transmission, processing and storage of information are improved. The baby’s psyche is actively developing. After birth, the process of brain development will continue, but the baby will already be able to perform actions necessary for survival (innate reflexes)
In the areas of the brain responsible for perceiving information from the senses, connections between neurons are strengthened. Thanks to this, the fetus can not only perceive light, sound, taste and smell, but also remember them.
At the 30th week, the baby already has good command of the eye muscles. Eyelids with tiny eyelashes rise and close. The baby is trying to perceive his surroundings. While these are just the first tests, vision still has a lot to learn, but only after birth. At this stage, the baby can only distinguish between light and darkness; color perception is not yet available to him.
The fetus already hears and remembers various sounds. The most pleasant sounds for him are the sound of his mother’s voice and her heart. After birth, these important sounds will calm the baby and create a sense of security. Expectant parents are recommended to strengthen their bond with the baby by talking to him, singing songs, and talking about his anticipation.
The sensitivity of the fetal skin has noticeably improved. Now he has access to sensations over the entire surface of his body, and he reacts to them. The skin has already matured well and is gradually taking on protective functions. Beneath it, a small layer of subcutaneous fat is already noticeable, which is necessary for thermoregulation and providing the newborn baby with the necessary nutrients in the first days of life.
The vernix lubrication covering the entire body of the fetus has practically fulfilled its functions and is beginning to slowly disappear. Its remains will help the baby pass through the birth canal and will disappear in the first days of life outside the mother’s womb.
The hairs (lanugo) that hold the original lubricant on the surface of the skin slowly fall off. By birth, most of them will disappear; they may remain only on the shoulders, arms and forehead. But even these small areas of lanugo will quickly disappear in the first days of life.
The hair on the head, on the contrary, continues to grow. By this week they have already acquired the color with which the baby will be born. Their length may vary. Some children are born with quite thick hair, others almost bald. Both of these options are normal. During the first year of life, your baby's hair will change. In areas most often exposed to friction (the back of the head, temples) they will be erased, and in their place, closer to a year of life, new, stronger hairs will appear.
Important processes occur in the respiratory system this week. Alveoli (tiny bubbles responsible for gas exchange) in the lungs continue to form. By birth there should be about 24 million of them in each lung. To prevent the walls of the alveoli from sticking together during the first breath, the fetal body is already accumulating surfactant.
If born early this week, the baby may well begin to breathe on his own, but he will still need medical attention.
So that after birth the lungs can expand and receive a sufficient amount of oxygen, an active process of preparing the respiratory system is already underway. Amniotic fluid enters the lungs through the nose, in which the mucous plug has disappeared. The glottis is still closed. Don't worry about there being some water in your lungs. For now, he receives oxygen from his mother, through the umbilical cord, and at the moment of birth, everything unnecessary will go away.
If you observe the fetal chest during an ultrasound, you can see how it rises and falls. This trains the muscles of the sternum, which are necessary for breathing. The baby is actively preparing for life outside of his mother.
All internal organs learn to work together. The gastrointestinal, urinary, cardiovascular, immune and other systems have studied their tasks well and cope with them successfully. Amniotic fluid swallowed by the fetus is successfully processed: useful substances are sent to the development of the body, unnecessary substances are excreted through the kidneys or stored in the intestines.
The baby's reproductive system has completed its intrauterine development. Minor changes will still occur, but the main reproductive organs have already been formed. When studying a fetus on an ultrasound, it is almost impossible to make a mistake about the gender. The only obstacle to obtaining this information may be the baby’s position: he can lie sideways and cover his genitals with his hands.
Weight gain
The optimal weight gain for women of normal build in the second half of pregnancy is about 250–300 g per week. Total weight gain at the end of week 30 is approximately 9.3 kg. Did you score more? Don’t worry, don’t try to lose weight on your own and don’t go on a diet (this can harm your baby!), but be sure to consult with your doctor - he may prescribe special fasting days for you during pregnancy. Did you score less? Don’t be upset either - as a rule, this is typical for women who are overweight to the point of “interesting position”. This state of affairs, however, does not exclude the need to consult with a good specialist as soon as possible and, if necessary, take the necessary measures to improve your condition.
Condition of the uterus at 30 obstetric weeks
The uterus has not yet reached its maximum size, but is already quite large. Its bottom is located approximately 30 cm from the area of the pubic joint and at a distance of approximately 10 cm above the navel. During this period, the walls of the uterus become thinner due to stretching, the weight of the uterus increases, the cervix is completely closed, and in its pharynx there is a lump of persistent mucus (mucus plug), which protects the fetus and membranes from infection. During this period, Braxton-Higgs training contractions, painless and irregular tension of the walls of the uterus to prepare muscle fibers for childbirth, become more frequent. These contractions do not lead to dilatation of the cervix, do not cause severe discomfort, and may occur more often when tired and in the evening. They go away when changing body position, resting in a supine position.
Rhythmic and painful contractions of the uterus, accompanied by vaginal discharge, pain and heaviness in the lower back, the appearance of blood on the underwear or the discharge of amniotic fluid, can be dangerous. In this case, the onset of premature labor is assumed and you need to immediately go to the maternity hospital.
Due to the growth of the uterus, the abdomen has increased significantly; it protrudes forward, the navel is everted, and a pronounced dark pigment stripe runs down from it. A change in the center of gravity due to the abdomen affects the mother’s gait; she walks slowly and waddles, which is facilitated by the relaxation of the ligaments of the hip joint. With such a belly, you need to be more careful getting out of bed on your side, climbing stairs and walking down the street. Due to stretching of the skin, itching and stretch marks may occur; prevention should be carried out using moisturizers or oils.
Mom's belly
The belly continues to increase at 30 weeks, which is associated with active growth of the fetus. Because of her belly, mom becomes clumsy, not only her figure changes, but also her gait. Moving (walking, sitting down, climbing stairs, bending over, getting out of bed) now needs to be done with great caution - sudden movements can cause painful sensations. It is difficult to say exactly what size the belly should be at 30 weeks: the concept of “normal” in this matter is very relative; for a doctor in a antenatal clinic, the main indicator is the growth of the abdomen over time.
Tests and studies during pregnancy
Visiting a doctor monitoring your pregnancy: once every two weeks. Weighing, measuring blood pressure, measuring the height of the uterine fundus, listening to the fetal heartbeat.
General urine test - before each visit to the doctor. Indicates the quality of kidney function.
Receive an exchange card with the results of tests and examinations - 30 weeks after the first day of the last menstruation. It is recommended that you always carry this document with you, which is required for admission to the maternity hospital.
Registration of maternity leave for workers - 30 weeks after the first day of the last menstruation.
Tests and ultrasound
At week 30, it is time for the third planned ultrasound scan during pregnancy. Ultrasound at this stage allows you to examine parts of the baby’s body and its organs, assess the condition of the placenta, trace the possible entanglement of the umbilical cord of the fetus, determine low or polyhydramnios, and the position of the child in the uterus. Additionally, at this time, doctors can prescribe Doppler ultrasound (lately it has been recommended to almost all mothers) - this is a type of ultrasound diagnostics, a method that allows you to assess the state of blood flow in the vessels of the child, uterus and placenta. At week 30, the now “traditional” general urine test for a pregnant woman is also maintained.
What do they look for on an ultrasound?
What do they look for on an ultrasound at 30 weeks of pregnancy? This diagnostic method allows you to estimate the size and weight of the child. Together with data on the size of the mother’s pelvis, the issue of labor management tactics is resolved. It is possible to conduct childbirth through the natural birth canal or by surgical intervention - caesarean section.
Mother's condition
This diagnostic technique makes it possible to visually determine the condition of the mother’s internal organs, in particular the uterus and its appendages. In some situations, various diseases and pathological processes are identified that can interfere with physiological labor (for example, tumors).
A preventive examination of the pelvic organs is also carried out to determine inflammatory processes and other pathologies, if any.
Child's condition
Ultrasound of the fetus at 32 weeks of pregnancy aims to determine the final position of the fetus in the womb. This, as well as fetometry data, allows you to choose the optimal option for managing childbirth. The fetal heartbeat is also assessed - the frequency and rhythm of heart contractions are analyzed. It is clarified whether there is any entanglement in the umbilical cord.
It is possible to detect congenital developmental pathologies in the third trimester. They develop as a result of the mother’s exposure to various viral diseases, injuries received during pregnancy, or for other reasons (for example, genetically determined).
Also an important point of screening during the third trimester
is to determine and clarify the location of the placenta.
Baby's weight at 32 weeks
Normally, the weight of the fetus at the beginning of the third trimester ranges from 1300 to 1500 g. Slight deviations from these indicators are possible. If the child’s weight is 2500 g or more, then they speak of a tendency for the development of a large fetus. At the time of birth, its weight can reach more than 4 kg. It is also possible that the body weight indicator may deviate downward. At the same time, during an ultrasound examination, all body systems are carefully checked to determine whether the child is underdeveloped.
Fetal development
During the third trimester, ultrasound clearly shows high fetal motor activity. At this stage, most systems are already practically formed. The specialist studies in detail the state of the cardiovascular, nervous, gastrointestinal and other systems of the fetus.
Sex at 30 weeks pregnant
In the third trimester, special attention should be paid to intimate perineal massage, which will reduce the likelihood of ruptures during childbirth. Of course, the expectant mother is able to perform such a procedure on her own, but it is much more pleasant when a partner does it for the woman. Intimate massage for pregnant women, in the absence of medical contraindications, will be an excellent prelude to sex. But remember: love games at 30 weeks should not be particularly passionate and too “violent” imagination - you don’t want to give birth ahead of time! You need to massage the intimate area (your fingers at this moment should be at a depth of about 3 cm in the vagina) for about 2 minutes. Before starting the procedure, mix several oils, in particular, St. John's wort and wheat germ oils - this will make the touch more sensual (you can also use olive oil and even sunflower oil). In this matter, it is unnecessary to recall the rules of personal hygiene that both a man and a pregnant woman must observe.
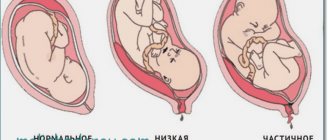
Head presentation of the fetus
In obstetrics, births that occur with an anterior occipital cephalic presentation (the back of the head is facing anteriorly) are considered correct and prognostically favorable, which helps create an optimal relationship between the size and shape of the head and pelvis of the woman in labor.
In this case, at the entrance to the pelvis, the fetal head is bent, the chin is close to the chest. When moving through the birth canal, the small fontanelle is the leading conducting point. Bending the head somewhat reduces the presenting part of the fetus, so the head passes through the small pelvis in its smaller size. Simultaneously with the movement forward, the head makes an internal rotation, as a result of which the back of the head turns out to be facing the pubic symphysis (anteriorly), and the face is facing the sacrum (posteriorly). When the head erupts, it is extended, then the shoulders rotate internally and the head externally rotates so that the baby’s face is turned toward the mother’s thigh. Following the birth of the shoulder girdle, the baby's torso and legs appear without difficulty.
In the case of labor progressing in the posterior view of the cephalic occipital presentation of the fetus, the back of the head turns toward the sacral cavity, i.e., posteriorly. The forward advancement of the head with a posterior-occipital cephalic presentation of the fetus is delayed, and therefore there is a possibility of developing secondary weakness of labor or fetal asphyxia. Such births are conducted expectantly; in case of weak labor, stimulation is performed; if asphyxia develops, obstetric forceps are applied.
The mechanism of birth with anterior cephalic presentation of the fetus in its main points coincides with the previous version. The conductive point with such a presentation of the head is the large fontanelle. The tactics of childbirth are expectant; surgical delivery is undertaken in the event of a threat to the health of the mother or fetus.
With frontal cephalic presentation of the fetus, spontaneous labor is extremely rare and takes a long time with a protracted period of expulsion. With independent childbirth, the prognosis is often unfavorable: complications in the form of deep perineal lacerations, uterine ruptures, formation of vesical-vaginal fistulas, asphyxia and fetal death are common. If a frontal cephalic presentation is suspected or determined, the fetus can be rotated even before the head is inserted. If rotation is not possible, a caesarean section is indicated. In case of complicated spontaneous labor, a craniotomy is performed.
The conditions for a successful independent delivery with a facial cephalic presentation of the fetus are the normal size of the mother's pelvis, active labor, a small fetus, and an anterior view of the cephalic presentation (chin facing anteriorly). Childbirth is conducted expectantly, with careful monitoring of the dynamics of labor and the condition of the woman in labor, the fetal heartbeat using cardiotocography and fetal phonocardiography. In the posterior type of facial presentation, when the chin is turned posteriorly, a cesarean section is required; If the fetus is dead, a fetal destruction operation is performed.
Lifestyle
The time has come when you can and should prepare for childbirth. In particular, it is necessary to activate the muscles that make it easier for the baby to move through the birth canal. In this regard, a set of exercises developed by the American gynecologist Arnold Kegel is very effective. The point of Kegel exercises for pregnant women is to alternately tense and relax the muscles of the perineum. First of all, we are talking about the pubococcygeus muscle. Finding it in yourself is quite simple: when you want to go to the toilet “in a small way”, sit on the toilet, spread your legs and begin the “process”. As you go, try to stop the stream without moving your legs. You yourself will feel which muscle will tense the most - you need to work with it. The pubococcygeus muscle should be squeezed and unclenched in any position (about 10 repetitions) at least 5 times a day.
It is possible and it is not possible
At week 30, a woman should continue to treat herself carefully and carefully. There are some recommendations that, if followed, can avoid many negative consequences:
- strict adherence to the gynecologist’s prescriptions, timely completion of the necessary tests;
- complete abstinence from alcohol, nicotine, and drugs;
- minimal contact with household and construction chemicals;
- compliance with food and drinking regimes;
- refusal of harmful products and semi-finished products;
- control over the daily routine: sleep - 8 hours at night, during the day as needed, meals - 5-6 times a day in fractional portions, physical activity and walks outside - daily;
- change body position every 20 minutes when working while sitting, rest during physical activity - every 60 minutes;
- control of body hygiene;
- maintaining order and cleanliness at home;
- performing household tasks allowed for pregnant women. Do not hang curtains on your own, do not move furniture, do not come into contact with complex chemical compounds;
- minimal contact with sick people;
- maintaining calm and good mood.
From the 30th week it is recommended to begin the process of preparing for childbirth. Recommended:
- train your pelvic floor muscles with Kegel exercises;
- study breathing exercises necessary during childbirth;
- attend special courses for expectant mothers at the clinic.
Sex
Sex at 30 weeks is an important element of a marital relationship. If the doctor has not issued a direct ban on intimate life, then if you feel well, communication is not only possible, but also useful.
It is recommended to follow some safety precautions:
- choose positions that are comfortable for a pregnant woman, eliminating pressure on the abdomen and severe tension;
- avoid too active movements and deep penetrations;
- try to use a condom to avoid early cervical ripening.
Beauty and accessories
During pregnancy, the legs suffer greatly, as they bear a “double load”! Special compression tights for expectant mothers will help your legs - wearing them is rightfully considered one of the most effective ways to prevent varicose veins, as well as heaviness in the legs and swelling while waiting for the baby. Compression tights are made from medical knitwear; they do not compress the stomach and waist and are perfect for everyday wear. You can buy them at the pharmacy. However, before purchasing, we recommend that you consult with a specialist.
Recommendations for the expectant mother
Despite the fact that the child is already fully formed, premature birth at this stage can result in developmental disorders in the future. Therefore, a pregnant woman needs to follow a number of recommendations:
- Regularly visit the residential complex and take the necessary tests. Based on urine and blood tests, you can notice the first signs of gestosis, as well as anemia, which can result in fetal hypoxia.
- Follow your doctor's instructions carefully. You should not self-medicate or use traditional medicine, as this may lead to negative consequences.
- Take care of your body. The use of special moisturizers will help prevent the appearance of stretch marks. When releasing colostrum, you can use special breast pads.
- Don't ignore visiting specialists. If you have a toothache, visit the dentist. If you have vision problems, be sure to undergo a re-examination by an ophthalmologist.
- Avoid long trips. Prolonged sitting puts stress on the cervix, which can begin to shorten ahead of schedule. Air travel can cause a drop in pressure, which can trigger premature birth.
- Limit fluid intake before bed. This will help reduce the amount of swelling in the morning.
- Perform drainage exercises. They help relieve the load of the growing uterus on the kidneys and blood vessels of the lower extremities.
- It is better to sleep on your left side. This reduces the load of the uterus on the spine, inferior vena cava, and internal organs.
For all questions regarding future trips and workloads, you should definitely consult a gynecologist.
Registration of maternity leave
With the onset of the 30th week of pregnancy, the mother is entitled to maternity leave, which lasts 140 days (70 days before childbirth and 70 days after childbirth), then leave to care for a child up to 1.5 years and 3 years is issued. If you are expecting one baby, your vacation will begin from the 30th week of pregnancy. If you are expecting twins, you are entitled to leave from 28 weeks. But there is no need to wait for these deadlines in order to notify the employer about going on vacation, since you still need to find a replacement for you. It is better to notify him 2-3 weeks in advance.
What is needed to apply for maternity leave?
To apply for leave, you first need to come to the antenatal clinic at 30 weeks (or 28 weeks). After the examination, you will be given a certificate of incapacity for work and a certificate of registration in the early stages of pregnancy. On the day the certificate of incapacity for work is issued, you need to come to work with documents to the HR department. The HR department, on the basis of the application and certificate of incapacity for work, issues an order for granting leave under the BiR. The day indicated on the certificate of incapacity for work is the first day of vacation! To apply for a vacation, you will need to collect some documents:
List of documents for maternity leave
- A completed certificate of incapacity for work. The date from which you go on maternity leave must also be the date from which sick leave is opened.
- Certificate of early registration. This certificate is issued at the antenatal clinic for registration for up to 12 weeks. She is entitled to an allowance of 680 rubles.
- Application for leave. The application form is available at the organization. It’s worth immediately adding a clause about the request to accrue the corresponding benefits, otherwise they will have to be processed separately.
- Passport and its copy.
- If the length of service in the organization is less than 2 years, then it is necessary to provide a certificate of income from the previous organization in Form 182-to calculate payments.
Having received the relevant documents from the pregnant woman, the employer is obliged to assign benefits within 10 days and pay wages on the next day after the appointment (Article 15 of Law No. 255-FZ). The Labor Code enshrines the right to go on maternity leave and receive benefits for a pregnant woman of any social status, for example:
- Pregnant women who have signed an employment contract (work experience does not matter);
- Full-time students;
- Women in military service;
- Women who work for an individual entrepreneur or are themselves individual entrepreneurs.
If a pregnant woman is temporarily unemployed, she is also entitled to payments. For this purpose, the social authorities. Protection for a pregnant woman must be provided:
- Statement;
- Certificate of incapacity for work issued by the antenatal clinic;
- A certificate confirming that the woman is unemployed.
However, it is worth considering that some types of paid maternity benefits are available to everyone, and some - only to officially employed pregnant women. And also, do not forget to make a copy of the certificate of incapacity for work for the maternity hospital. A copy may be needed to extend leave in case of complicated childbirth.
Dangers and complications
The thirtieth week of pregnancy is generally a calm and safe period. The main threats are behind us, and if the pregnancy is not complicated by oligohydramnios, polyhydramnios, or pathologies of the placenta, the expectant mother only needs to monitor her body weight and edema.
1.5% of pregnant women experience polyhydramnios and oligohydramnios. To a moderate extent, both conditions are treatable, but require careful monitoring and special tactics for managing pregnancy and childbirth.
Placental pathologies are a complex of abnormalities in the development of the placenta that affect the viability and health of the child. The main causes of pathological development of the placenta are considered to be infectious and viral diseases suffered in the first or second trimester, extragenital pathologies of the mother (diabetes mellitus, hypertension, non-obstructive chronic bronchitis, etc.). Deviations in the development of the placenta are determined during an ultrasound examination. For some pathologies, the diagnosis is clear already at the second planned ultrasound. To clarify others, several ultrasound scans will be required over time.
The normal increase at 30 weeks is 7-8 kg. Slightly less than half of this weight is the weight of the uterus, fetus and the volume of amniotic fluid. The rest is subcutaneous fat, gained by the mother’s body, and... edema. These are the ones that need to be carefully monitored. Obvious swelling is visible to the naked eye:
- Rings cannot be removed from fingers;
- the usual shoes are tight;
- when pressing on the shin, a slightly lighter pit is formed, disappearing within 40-60 seconds.
Not all obvious swelling is a classic sign of gestosis. But in the presence of chronic heart and kidney diseases, and excess weight, they become the first danger signals.
Hidden edema is dangerous because the legs, arms and face look completely normal, not swollen, and at this time gestosis is gaining strength.
There are only two ways to control hidden edema: weigh yourself regularly and compare the amount of fluid you drink with the volume of urine excreted. Weighing is the easiest and most accessible way. According to him, an increase of more than 450-500 grams per week is a symptom of hidden edema.
Report your measurements to your obstetrician-gynecologist and be sure to take a urine test. If the results show the presence of protein, hospitalization is required!