What are atypical lymphocytes and what do they look like:
As is known, when irritated by antigens, as well as during certain diseases (viral diseases, allergies), lymphocyte counts increase. Along with this, some of them change their properties and appearance.
Atypical lymphocytes acquire the following features
They get big. Typically, macrophages are the largest leukocytes, and lymphocytes rarely “grow” to more than 12 microns. When they become atypical, their size can be 30 microns or more.
A normal lymphocyte has a shape close to round. Changed cell shapes acquire an irregular, polygonal shape, and their borders may look “ragged.”
The nucleus of an ordinary cell is round or slightly elongated. In an atypical lymphocyte it may remain this way, but it is often elongated, with “eaten away” contours, constrictions or clefts. It happens to be reduced.
If a blood smear, in which lymphocyte indicators are studied, is stained with standard dyes (hematoxylin and eosin are used for this), then the atypical cells will acquire a brighter color than the “normal” ones. Their nucleus is purple, and the cytoplasm is gray, dark blue or light blue. If atypical lymphocytes appear in a patient infected with cytomegalovirus or Epstein-Barr virus, they are called Downey cells. The fact is that in 1923, an American hematologist with the same name was one of the first to see them under a microscope and describe their properties. Some lymphocytes with atypical properties are also called Reader cells, or amitotic lymphocytes. Their peculiarity is that they have a kidney-shaped shape and nuclei with jagged contours or a constriction in the middle, dividing them into lobules. Also among atypical lymphocytes, Botkin-Klein-Gumprecht cells are distinguished. Three scientists at once described specific cells that occur in lymphadenosis. Actually, these are not living cells, but their remains, which circulate in the blood for some time. Because they are barely visible, these lymphocytes are also called shadow cells.
What causes the appearance of atypical lymphocytes?
When a person is sick and his body needs protection, the immune system must produce a sufficient number of lymphocytes so that together they can cope with the aggressor. Unfortunately, sometimes there are not enough immune resources for this. Cells are produced, but cannot fully mature and prepare to meet a pathogen or allergen. So it turns out that the number of such unusual lymphocytes in the blood increases. They perform the necessary functions, but their “appearance” is not very complete.
As soon as the patient gets better, the blood picture immediately, in just a few days, improves.
Sometimes high lymphocytes in the blood and the appearance of atypical forms are observed not only with ARVI and allergies, but also in more serious situations. Whooping cough, syphilis, tuberculosis, lymphocytic leukemia, brucellosis, toxoplasmosis, and serum sickness can lead to the appearance of large numbers of them.
Why can the level of lymphocytes in the blood change?
Lymphocyte levels can change for several reasons. Firstly, age . In childhood, the number of white blood cells is significantly higher than in adults.
Secondly, the most common occurrence is, of course, diseases . Depending on the problem, as well as its severity, the number of lymphocytes may either increase or decrease.
Either way, in most cases this is a bad sign.
Why is a change in lymphocytes in the blood bad?
Any deviation from the norm is proof that there are foreign bodies : viruses, bacteria, tumors.
They lead to inflammation, infection of the body’s own cells, and so on. All this affects both the increase and decrease in the number of lymphocytes in the blood.
But one way or another, if the number of these cells changes, this indicates that the body is struggling with a problem .
Symptoms and signs of lymphocytosis
Lymphocytosis is an increased number of lymphocytes in the blood. Only a doctor can always give an accurate diagnosis . However, there are a few symptoms that may make you consider visiting a specialist.
Among them:
- Enlarged lymph nodes, spleen and liver;
- External signs – nasal infections, hyperemia of the oral mucosa, relatively low level of general condition;
- Symptoms of respiratory tract disease;
- A sharp decrease or increase in body temperature, accompanied by chills and general exhaustion;
- Bowel dysfunction, nausea, constipation and diarrhea;
- In children - characteristic paroxysmal vomiting;
- General disorder of nervous activity, insomnia, severe enlargement of the tonsils against the background of a rise in temperature to 40 °C.
Symptoms and signs of lymphopenia
Most often, the lack of lymphocytes in the blood does not manifest itself in any way. And it is almost impossible to detect this problem in yourself without a blood test. However, there are several symptoms that may prompt you to see a doctor.
Among them:
- Absence or reduction of tonsils or lymph nodes indicate cellular immunodeficiency;
- Skin diseases (such as alopecia, eczema, pyoderma, telangiectasia);
- Signs of hematological diseases (such as pallor, petechiae, jaundice, ulceration of the oral mucosa);
- Generalized lymphadenopathy and splenomegaly, which may indicate the presence of HIV infection or Hodgkin lymphoma.
The basic laboratory method for determining the number of lymphocytes in the blood is a clinical (general) blood test with a leukocyte count.
In modern general blood tests, lymphocytes are designated by the Latin abbreviation LYM .
For adult men and women, there is not much difference in the number of lymphocytes in the blood. However, the immune system of women is more active and adaptive , so the number of lymphocytes in the blood of women during analysis may be higher compared to a blood test in men.
;For men; For women; For children
Norm; from 1000 to 4800/µl; from 1000 to 4800/µl; from 2000-11000x10/9/l to 1250-7000x10/9/l
Diagnostics: how is the level of lymphocytes determined?
The level of lymphocytes is determined by a routine general (clinical) blood test. To obtain the most accurate results, a general blood test is taken in the morning on an empty stomach (children under 1 year old - at least 2-3 hours, over a year old - 8 hours fasting). You can drink water as usual.
It should be remembered that physical overexertion, stress, taking certain medications, and conducting a number of studies (for example, X-ray) can affect the results of the analysis . On the other hand, in an emergency situation, it is permissible to conduct a general blood test during the day, 1 hour after eating.
The data obtained, as well as the plan for further examination and treatment, must be discussed with the pediatrician, since all changes in blood tests must be compared with the clinical picture of the disease .
A clinical blood test may reveal a change in the number of lymphocytes: an increase (lymphocytosis) or a decrease (lymphopenia).
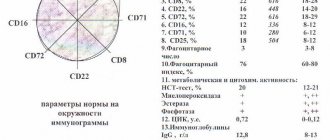
To correctly interpret the results, it is also necessary to evaluate the total number of leukocytes, the ratio of other components of the leukocyte formula (neutrophils, monocytes, eosinophils), and the values of other indicators (red blood cells, hemoglobin, platelets). Changes in the content of lymphocytes do not have independent clinical significance and are a reflection of the current infectious or autoimmune process.
An increase in the content of peripheral blood lymphocytes is most often observed during viral infections. Severe lymphocytosis accompanies the following infections :
- Epstein-Barr infection
- cytomegalovirus infection
- herpes virus infection type 6
- viral hepatitis
- adenovirus infection
- childhood infections (measles, chicken pox, rubella, mumps)
With some bacterial infections (whooping cough, syphilis, tuberculosis) and protozoal invasions (toxoplasmosis, malaria), the level of lymphocytes may also increase.
A general blood test may reveal atypical mononuclear cells (B-lymphocytes affected by the virus) or plasma cells. Their appearance in the peripheral blood indicates an acute course of the infectious process and the need for antibody synthesis.
Also, with an acute viral infection, a decrease in the number of lymphocytes (lymphopenia) is possible. Most often it is observed with ARVI , especially with influenza , and goes away on its own after recovery.
In rare cases, the cause of significant change in the number of lymphocytes, both an increase and a decrease, may be:
- autoimmune or hematological disease,
- congenital or acquired immunodeficiency condition,
- taking certain medications,
- toxic effects of harmful substances
, additional studies may be carried out in a clinic to clarify the diagnosis :
- Blood chemistry
- Serological studies (determining the level of IgG, IgM antibodies to infectious agents, PCR diagnostics)
- Ultrasound examination of the abdominal organs, radiography of the chest cavity
If congenital or acquired immunodeficiency , an immunogram is performed, which reflects the ratio of different types of lymphocytes and their ability to carry out an immune response.
To clarify the diagnosis, it may be necessary to consult with specialized specialists : infectious disease specialist, hematologist, rheumatologist.
The human immunodeficiency virus is dangerous precisely because it affects human white blood cells - lymphocytes of the T-cell category.
What to do if there are elevated levels of atypical lymphocytes in the blood?
There is only one option: to be treated by taking therapy prescribed by the doctor. This, depending on the nature of the disease, can be a variety of medications and techniques. In addition, in consultation with your doctor, you can take Transfer Factor.
The presence of atypical lymphocytes indicates that the human immune system is working under strain. This tool allows her to help. It is created on the basis of information molecules extracted from cow colostrum and egg yolks. Molecules “train” lymphocytes to function properly, which accelerates their formation, maturation and improves performance. Regular use of the drug helps to quickly restore health and return normal blood counts.
Pain and heaviness in the left hypochondrium
Gastritis
Ulcer
16716 May 27
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Pain and heaviness in the left hypochondrium: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
The left hypochondrium is the area of the anterior abdominal wall located below the left costal arch. To understand the reasons for the development of pain in the left hypochondrium, it is necessary to know which organs are projected onto the area of the anterior abdominal wall.
The stomach is a section of the gastrointestinal tract, which is a muscular sac. Gastric juice is produced here, the main components of which are hydrochloric acid, pepsin (an enzyme that breaks down proteins) and mucin (mucus that protects the walls of the stomach from the aggressive effects of hydrochloric acid). Once in the stomach, protein food undergoes denaturation (a process of structure change, which can be represented as a change in egg white during heat treatment - thickening, as a result of which proteins become insoluble in water) due to the presence of hydrochloric acid, and the denatured protein, in turn, is digested under the action of pepsin. From the stomach, food enters the duodenum, where digestion continues.
The spleen is an organ of the immune system. The content of lymphocytes in the spleen reaches 85% of the total number of cells, which is almost 25% of all lymphocytes in the body. About 50% of spleen lymphocytes are represented by B-cells - humoral immunity depends on them. Thus, it is the spleen, along with the lymph nodes, that is the organ that provides humoral immunity. In addition, the destruction of old and abnormal red blood cells and platelets occurs in the spleen, which helps to renew the cellular composition of the blood.
In newborns, in addition to the stomach and spleen, the left lobe of the liver can be projected into the area of the left hypochondrium.
This is due to the fact that the liver occupies almost the entire epigastrium in infants. Types of pain and heaviness in the left hypochondrium
Pain and heaviness in the left hypochondrium can be acute or chronic. The pains are drawing, dull, bursting, spastic, “dagger”, shooting.
Depending on the presence of a provoking factor, pain can be spontaneous, or it can develop during meals or as a result of hunger, physical activity, or emotional stress.
According to the mechanism of development, pain is classified into spastic, distensional, peritoneal and vascular.
Possible causes of pain and heaviness in the left hypochondrium
The cause of pain is irritation of pain receptors located in the abdominal organs, in the peritoneum (the serous membrane that lines the abdominal cavity from the inside and passes to the abdominal organs), in the wall of the abdominal cavity. Spasmodic pain occurs due to uncontrolled persistent tension in the smooth muscles of the wall of a hollow organ, such as the stomach.
Muscle spasm can be triggered by the influence of the aggressive environment of gastric contents on the wall of the organ, activation of the structures of the autonomic nervous system.
The cause of the development of distension pain is excessive stretching of a hollow organ from the inside by its contents, which can happen when consuming an excess amount of food or impaired evacuation of contents from the stomach due to impaired motility or some mechanical obstruction in the outlet section of the stomach.
Peritoneal pain occurs due to irritation of the peritoneum. The peritoneum is a thin film that covers the inside of the abdominal wall and the organs located in it (some completely, others on several sides). As a result of the inflammatory process in the wall of the organ, local peritonitis develops - inflammation of the peritoneum, which is accompanied by pain.
Finally, the cause of vascular pain is cell death due to insufficient blood flow in any organ. Impaired blood flow is most often caused by blockage of a vessel (artery or vein) with a blood clot (thrombus).
Diseases leading to pain and heaviness in the left hypochondrium
One of the most common causes of pain in the left hypochondrium is stomach pathology. Gastritis
is an inflammation of the mucous membrane lining the stomach from the inside.
Gastritis can be associated with the entry of any aggressive chemicals into the stomach, with autoimmune inflammation, but most often the disease is associated with an infection caused by Helicobacter pylori
.
Helicobacter pylori bacterium
, being present in the body for a long time, can lead to more serious diseases - peptic ulcer of the stomach and duodenum, and in some cases - to tumor damage to the stomach.
Heaviness and pain in the left hypochondrium, often combined with pain behind the sternum, may indicate the presence of gastroesophageal reflux
(reflux of gastric contents back into the overlying esophagus).
Impaired evacuation of food from the stomach is more common in children in the first year of life due to pyloric spasm
and
pyloric stenosis
(transient or permanent organic disturbance of the patency of the pyloric - outlet - section of the stomach). In adults, this condition can be caused by neoplasms that become a mechanical obstacle to food in both the stomach and intestines.
Among the pathological conditions of the spleen that can lead to pain in the left hypochondrium, it is worth highlighting its enlargement (splenomegaly) and impaired blood supply (splenic infarction).
Splenomegaly
develops in various infectious diseases, diseases of the blood system, incl.
leukemia, as well as cirrhosis of the liver. The cause of splenic infarction
is thrombosis of its vessels, which occurs against the background of conditions characterized by increased blood clotting.
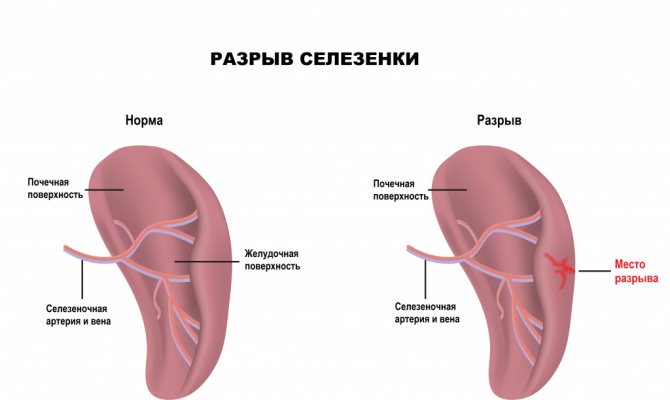
Separately, it is worth mentioning traumatic ruptures of the spleen
, which also lead to the development of pain, but the doctor will primarily be concerned about massive life-threatening intra-abdominal bleeding from the damaged organ.
It is important to remember that due to the proximity of the heart to this area, pain in the left hypochondrium can develop due to damage to the heart muscle - myocardial infarction
.
Which doctors should you contact if you have pain and heaviness in the left hypochondrium?
If you experience pain and a feeling of heaviness in the left hypochondrium, you should contact or. After a survey, clinical examination and the appointment of a number of laboratory and instrumental studies, the patient can be referred to specialized specialists - a hematologist, a nutritionist.
It should be remembered that acute intense pain in the left hypochondrium, especially in the presence of a previous injury or peptic ulcer, can be a symptom of acute surgical pathology.
In this case, an emergency consultation or calling an ambulance is indicated.
Diagnostics and examinations for pain and heaviness in the left hypochondrium
Identification of the cause of pain and heaviness in the left hypochondrium is based on data from an objective medical examination and auxiliary data from laboratory and instrumental studies. These include:
- clinical blood test with determination of the leukocyte formula, necessary to exclude anemia, blood diseases, as well as inflammatory processes in the body;