MRI of the ankle
MRI of the knee joint
MRI of the elbow joint
Shoulder MRI
MRI of the hip joints
Indications
The shoulder joint is one of the most loaded joint systems of the musculoskeletal system. It is not surprising that regular stress on it can lead to degenerative pathologies and inflammatory diseases. If a person puts a lot of physical stress on his shoulder joints, their bone and cartilage structures begin to wear out quickly, and pain occurs. In addition, shoulder injuries are a common reason for visiting an orthopedist or traumatologist. In order to make an accurate diagnosis and identify the causes of shoulder dysfunction, the attending physician usually prescribes an MRI of the shoulder joint. The following symptoms may lead the patient himself to the idea that he urgently needs to undergo magnetic resonance imaging:
- pain and crunch in the shoulder;
- injuries in the shoulder joint, fractures;
- ligament ruptures, periodic dislocations;
- swelling in the shoulder area;
- improperly fused bones, the presence of bone spurs;
- pinched nerves, tendons;
- visually noticeable tumor.
Initial appointment with an ORTHOPEDIST
ONLY 1800 rubles!
(more about prices below)
What will an MRI of the shoulder show?
Magnetic resonance imaging of the shoulder shows infectious diseases, inflammatory processes, tumors and damage to various joint tissues well. MRI of the shoulder joint allows:
- Identify worn-out cartilage, new growths in bones, arthritis, arthrosis, osteoarthritis.
- Find areas of tendon and ligament rupture.
- Diagnose rotator cuff and biceps tendinitis.
- Identify a labral tear, which can be caused by a shoulder injury and can lead to severe pain.
- Find out the causes of unexplained pain in the brachial plexus area.
- Determine the presence of damage to the shoulder cuff.
- Diagnose rare diseases such as Milwaukee shoulder.
- Find signs of the beginning process of muscle tearing.
- Diagnose the condition of the shoulder joint after a fracture of the shoulder bones (in this case, MRI is much more effective than x-ray examination).
Shoulder joint on MRI image
MRI of the shoulder joint, how long does it take?
It takes approximately 10-15 minutes to complete the paperwork, interview and prepare the patient. Magnetic resonance scanning takes about 15-20. Contrasting extends the procedure time to half an hour. Preparing the results by a radiologist takes from 15 to 60 minutes. To undergo an MRI of the shoulder joint, the patient will have to spend 1 to 2 hours in the clinic, which is determined purely on an individual basis.
Shoulder MRI
How is an MRI of the shoulder done?
- MRI
- Ultrasound

MRI tomograph:
Siemens Magnetom C
Type:
Open (expert class)
What's included in the price:
Diagnostics, interpretation of images, written report from a radiologist, recording of tomograms on CD + free consultation with a neurologist or orthopedist after an MRI of the spine or joint

Ultrasound machine
HITACHI HI VISION Avius
Class:
Expert (installation year 2019)
What's included in the price:
Diagnostics, interpretation of images, written diagnostic report
Preparation
During a tomography of the shoulder joint, the patient can wear his own clothes, as long as they do not have brooches, rivets, metal buttons, zippers or other fasteners. In some clinics in St. Petersburg, examinees are given special disposable underwear to minimize the possibility of metal elements getting into the magnetic resonance imaging scanner. The MRI procedure of the shoulder does not particularly regulate food intake, but in the case of MRI diagnostics with contrast, doctors recommend not eating food for several hours before this study. This will help avoid nausea and other unpleasant sensations when a contrast agent is administered. Contrast testing in people with kidney failure will require consultation with a primary care physician or nephrologist and possibly a blood test for creatinine. For young children, MRI examinations are sometimes performed under anesthesia or sedation. The tomography procedure requires the patient to remain completely still, and this is very difficult to achieve in children. If your child is scheduled for an MRI under anesthesia, preparation will include a series of tests, a consultation with a pediatrician or neurologist, and dietary restrictions before the test. As a preventive measure, women are not recommended to undergo tomographic diagnostics during pregnancy in the first trimester. People who are overweight or have large body dimensions should, when scheduling an MRI of the shoulder, clarify the weight and size restrictions that this tomograph model can handle. A closed-type tomograph in a person with phobias can cause a panic attack, so if you suffer from claustrophobia, you can take sedatives an hour before the diagnosis or choose an MRI of the shoulder joint on an open tomograph[/anchor].
Computed tomography of the shoulder joint: what does it show?
The procedure involves performing a layer-by-layer scan of the shoulder joint. The computer then processes the received data and reproduces a two-dimensional or three-dimensional image. A CT scan of the shoulder joint shows in detail the condition of all structures of the joint capsule. Most often it is prescribed for a final diagnosis. Often, tomography is prescribed after conventional radiography, since it does not provide the amount of data and detail needed to identify the causes of the disease. During a CT scan, specialists can also assess the condition of soft tissues. However, MRI is many hundreds of times more detailed than CT.
CT scan of the shoulder joint: preparation for the procedure
Before performing a CT scan of the shoulder joint, the patient must get rid of all metal accessories and jewelry. All this can spoil the image and negatively affect the further treatment of the patient. If cancer is suspected, a contrast agent must be administered. Before the procedure itself, you should not eat for 6 hours.
Procedure
The tomography procedure of the shoulder joint takes on average 20-40 minutes. The duration of the scan depends on the tomograph model. In the diagnostic room, the patient is placed on a tomography table. Then a special coil is placed over the examination area. The table is moved into the scanning part of the device and the screening procedure is started.
The main task of the patient during the examination is to remain completely still. This is largely a guarantee of quality research. The fact is that the tomograph is very sensitive to any movement. If the patient moves the shoulder during the scan, motion artifacts appear on the tomograms. They reduce the effectiveness of the study and the overall quality of diagnosis.
Questions about diagnostics
Dress code
You can enter the MRI room in any clothing that does not contain metal. When going to the clinic, it is best to wear loose, non-restrictive clothing without metal elements (zippers, rivets, hooks), in which you can lie comfortably. For women, we recommend bringing a T-shirt or not wearing a bra with metal wires or hooks.
Preparation
This tomography does not require any preparatory steps from the patient.
Is MRI harmful to health?
MRI is a completely harmless diagnostic method for the human body. This method of examination can be carried out at any age and for any disease an unlimited number of times, unless you have contraindications.
Contraindications
Some pacemakers and foreign objects in the body may pose serious limitations to tomography. In particular, cochlear implants, vascular clips, stents, heart valves and insulin pumps, pacemakers, neurostimulators, steel screws, staples, pins, plates, joint endoprostheses may be a contraindication to diagnosis. The patient must notify the radiologist about all implanted objects in the body. The diagnostician will be able, based on information about the composition and model of the implant, to assess the possibility of conducting diagnostics.
If you are having an MRI with contrast, be sure to report any allergies to medications or kidney problems. It is also necessary to inform the radiologist about a possible pregnancy.
Is it possible to do an MRI with braces and dental implants?
Dental implants and crowns are not a contraindication to magnetic resonance imaging. The magnetic field does not have any negative effect on them. Fixed brace systems can produce artifacts on tomograms during MRI of the head. If the light effect is too strong, the doctor will stop the study and offer the patient alternative diagnostic methods.
Is the device noisy?
Any MRI machine in working condition makes noises reminiscent of tapping. The open tomograph is one of the quietest installations. The noise from its operation is significantly lower compared to closed tomographs. If the sounds of the operating unit cause you anxiety, you will definitely be offered special noise-canceling headphones.
What should I do if I have claustrophobia?
An open tomograph is the optimal solution for patients suffering from panic attacks in a closed space. It is open on the sides on three sides and does not create a claustrophobic feeling.
Can I take sedatives before an MRI?
If you are a little nervous, before the tomography you can take mild sedatives, for example, valerian, motherwort infusion or afobazole. Taking sedatives does not have a negative impact on the quality of MRI.
Why is it important not to move during the test?
Any movement during the examination reduces the quality of the resulting images. Multiple motion artifacts may appear on the images, and the MRI results will be uninformative.
Can I do the research with an accompanying person?
Absolutely yes. You can invite any accompanying person from among your family and friends to the MRI room. It is important that your companion does not have metal implants or artificial pacemakers in his body.
How is a CT scan of the shoulder joints done?

Patient position during examination
You can get a CT scan of the humerus in St. Petersburg in one of the diagnostic centers, in the radiology department of a hospital or clinic, where there is a computed tomograph. You must first make an appointment by contacting the operator through the website form or by phone. It is possible to undergo an emergency examination on the day of treatment.
How is the CT scan of the humerus performed?
The technician will ask you to take a certain position; For additional fixation of the limb, pillows or straps can be used - this will help maintain the correct position and obtain high-quality images. You may also need to hold your breath for a few seconds during short, individual scans to prevent blurry images. From the next room, a technician will use a remote control to move you deep into the tomograph, and the procedure itself will begin, during which special sensors will rotate around the body. For emergency situations during scanning, there is a button at hand to contact the staff. After completion, you need to wait some time for the technician to be convinced of the quality of the tomograms obtained: they must be clear so that the doctor can read them correctly in the future. A typical CT scan takes 5-10 minutes, which is important in the diagnosis of acute traumatic injuries.
Preparing for a shoulder examination
Native CT scan of the humerus is one of the non-invasive imaging tests and does not require special preparation. It is enough to choose loose, comfortable clothes without zippers or metal fasteners, remove jewelry: hairpins, chains, watches, etc. Bra underwire can also lead to the appearance of artifacts in images, so it is better to take care of this in advance. You need to take with you the results of previous examinations and discharge from the hospital, if any. After diagnosis, you can go about your usual activities.
Contraindications
Despite the fact that MRI of the shoulder is a safe diagnostic method, it is contraindicated in persons who have:
- metal objects in the body (shards, bullets, plates, staples);
- pacemakers, hearing aids and other electronic implants, the passport of which does not indicate o;
- Signs of inappropriate behavior of the subject (severe agitation, strange psychomotor reactions, panic);
- metal joint prostheses made of ferromagnetic alloys, such as steel;
- metal clips on vessels.
Metal elements used in modern orthopedics and surgery, in most cases, do not pose a danger during an MRI of the shoulder joint, but the patient must warn the doctor performing the procedure about the presence of any foreign objects in his body. The strong magnetic field of the tomograph can move them out of place and thereby damage surrounding tissue. Therefore, before a tomography, the radiologist may ask to see a certificate for a metal structure located in the patient’s body. After studying the data, he will assess the risks and make a decision about the safety of the study. If such documents are not available, it is recommended to undergo an X-ray examination before magnetic resonance imaging. It will show the presence of fragments, bullets or any other inclusions made of magnetic alloys in the body. Fillings and braces do not have a significant effect on the magnetic field of the tomograph and are not a contraindication to MRI of the shoulder joint. Previous Next
Decoding
Based on the results of the scan, the radiologist receives a series of images. Then, during the interpretation procedure, he compares the patient's shoulder anatomy with the standards and notes all identified anomalies in his conclusion. The process of decoding images takes on average 40-60 minutes. Based on the results of the scan, the patient receives the following package of documents - images recorded on film or electronic media, a doctor’s x-ray report and recommendations for further steps. With the results of the diagnosis, the person should go to his doctor. After interpreting the images obtained during the study, the attending physician can make a final diagnosis and prescribe effective treatment.
An example of an MRI transcript of the shoulder joint
On a series of MRIs of the right knee joint, the relationships in the joint are not disturbed.
A series of T1-weighted, T2-weighted, and proton density-weighted MR images using fat-suppression mode in the axial, oblique coronal, and oblique sagittal planes identifies the structures of the right shoulder joint. The relationship in the joint at the time of the study was not disturbed. The subacromial space is 6 mm (narrowed). The articular cavity of the scapula is flattened, its contours are smooth, with signs of subcortical osteosclerosis. There are small osteophytes along the edges of the glenoid cavity of the scapula. The head of the humerus is round in shape and not deformed. The articular cartilage has a heterogeneous structure, is unevenly thinned, its integrity is not compromised. The labrum can be traced along its entire length, degeneratively changed, without clear signs of a violation of integrity. The middle articular-brachial ligament is unevenly thickened, without breaking the integrity, but there is a small amount of effusion around it. The tendon of the supraspinatus muscle for 24 mm (mainly in the area of the muscle belly) is thickened, fibered with signs of edema and areas of calcification, changes are mainly observed in the anterior portion of the fibers - damage to the tendon of degenerative origin. There is slight swelling of the intermuscular tissue around the muscle belly of the supraspinatus muscle. The tendon of the subscapularis muscle in the area of attachment to the lesser tubercle of the humerus is thickened, minimally fibered, its overall integrity and tension are preserved (tendinosis-type changes). The tendons of the infraspinatus muscle in the area of attachment to the humerus have a heterogeneous MR structure, due to degenerative changes, the integrity is not broken. The tendon of the teres minor muscle is not changed. A moderate accumulation of free fluid is visualized in the cavity of the shoulder joint, moderate in the subcoracoid bursa. The tendon of the long head of the biceps brachii muscle is intact and there is minimal effusion along it. The right acromioclavicular joint is degeneratively changed: the articular surfaces have uneven contours with the presence of marginal bone growths, the articular ends themselves have subcortical osteosclerosis. The joint capsule is moderately thickened. CONCLUSION: MR picture of grade I-II osteoarthritis of the right shoulder and acromioclavicular joint, signs of impingement syndrome with partial damage to the supraspinatus tendon, moderately pronounced degenerative changes in the subscapularis tendon like tendinosis. Synovitis. Moderate tenosynovitis.
It is difficult for an ordinary person to independently understand and interpret the results that, after an MRI, will be given to him on a digital medium. Therefore, with the conclusion of the radiologist and the photographs, he should go for a consultation with the attending physician, who will make a final diagnosis based on the summary data of the examination, medical history and tomography data. In our clinic , after an MRI, you can have a free consultation with a neurologist or orthopedist . Doctor
- will answer all questions based on the results of the research and the conclusion received
- Helps explain tomography results without using complex radiological terminology
- will conduct an examination and, if necessary, offer treatment.
Author: Usenko Nikita Sergeevich
Orthopedist-traumatologist with 8 years of experience
Magnetic resonance imaging (MRI) in St. Petersburg
MRI of the shoulder joint. T2-weighted coronal MRI. Rotator cuff tear. Color processing of the image.
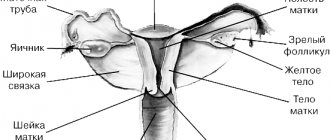
Brief information on the anatomy of the shoulder joint
Movement in the shoulder girdle is provided by the shoulder joint, acromioclavicular joint and sternoclavicular joint. In addition, between the chest and the scapula there is a false joint - the scapulothoracic joint. The shoulder joint is a synovial hinge joint. It consists of a hemispherical head of the humerus and a shallow glenoid socket in the scapula. Since the cavity is 4 times smaller than the head, a large range of movements in different directions is possible. The joint is protected from above by an arch formed by the coracoid process, the acromial process of the scapula and the coracoacromial ligament. The cartilage covering the head of the humerus is thicker in the center than at the periphery. The cartilage of the glenoid cavity, on the contrary, is thicker at the periphery than in the center. The joint is supported by soft tissue structures: the joint capsule, the coracohumeral ligament, the three glenohumeral ligaments, as well as the anterior pectoral muscle tendon bundles, the transverse humeral ligament and the labrum. The joint capsule completely surrounds the joint. The capsule is attached above to the circumference of the glenoid cavity behind the articular labrum, below to the anatomical neck of the humerus, with the greater and lesser tubercles of the humerus remaining outside the joint cavity, and the capsule spreads in the form of a bridge over the upper part of the intertubercular groove. The capsule is loose and thin so as not to reduce the range of motion. Additionally, it is reinforced with rotator cuff ligaments. The rotator cuff is formed by the tendons of 4 muscles. The labrum is located along the edge of the glenoid cavity. It performs stabilizing and shock-absorbing functions.
Diagram of the bony structures that form the shoulder joint.
Bony structures of the shoulder joint.

Anatomy of the shoulder joint. T1-dependent MRI in the coronal plane. Designations: 1 – articular (glenoid) cavity, 2 – clavicle, 3 – head of the humerus, 4 – subscapularis muscle, 5 – deltoid muscle, 6 – long head of the biceps brachii tendon, 7 – supraspinatus muscle, 8 – trapezius muscle, 9 – tendon of the supraspinatus muscle, 10 – upper lip.
Typical shoulder injuries
Injuries to the shoulder joint are relatively common. Causes include excessive range of motion in a joint or falling on an outstretched arm. There is also a non-traumatic etiology of instability in connective tissue diseases. MRI of the shoulder joint, along with radiography, are the main methods for detecting injury. The most typical (about 85% of anterior displacements of traumatic etiology) is a Bankart injury - separation of a fibrous or fibrocartilaginous fragment from the edge of the glenoid cavity at the site of attachment of the ligament to the glenoid cavity with damage to the articular labrum. In addition, the injury can also lead to bone injuries - anterior glenoid ring fracture, bony Bankart injury (that is, a Bankart injury combined with a fracture), and a fracture of the greater tuberosity.
MRI of the shoulder joint. Coronal T1-weighted MRI. Hill-Sachs and Bankart fractures.
A rotator cuff tear, also a characteristic injury to the shoulder area, can be associated with both trauma and degenerative processes. Rotator cuff tears can be complete or incomplete. In addition, according to MRI of the shoulder joint, 3 gradations are distinguished, which are based not only on signal changes on T2-dependent tomograms, but also on morphological changes in the tendon.

MRI. Coronal T2-dependent tomogram with fat suppression. Complete rupture of the supraspinatus tendon.
The injury easily leads to dislocations. The term “joint instability” refers to the condition of a joint when there are persistent problems in it that predispose it to dislocation. Chronic instability leads to frequent repeated dislocations and subluxations in the shoulder joint, which is complicated by its degeneration, the development of glenohumeral periarthritis, and deforming arthrosis. Instability is manifested by joint pain, discomfort, clicking in the joint and shoulder displacement. The patient is “stiff” in the shoulder and tries to avoid active and sudden movements.
Also, impingement syndrome can develop in the shoulder joint, which we described in the section “What causes pain in the joints and their diagnosis.” Along with the rotator cuff, adjacent structures may be damaged; MRI of the acromioclavicular joint is performed together with MRI of the shoulder joint.
Diagnosis of shoulder joint injuries
The role of radiodiagnosis in identifying and staging pathologies of the shoulder joint cannot be overestimated. In most cases, the correct use of radiation diagnostic methods provides complete information for the traumatologist and allows one to avoid arthroscopy. X-ray, although it does not allow to detect ruptures of the ligaments and labrum, remains a mandatory diagnostic method for injury to the shoulder joint. It allows you to detect fractures and bone defects, displacements, and free fragments.
Bone defects and defects in the hyaline cartilage of the glenoid cavity are clearly visible. The hyaline cartilage covering the head of the humerus is much less visible.
CT scan of the shoulder joint, Bankart and Hill-Sachs fractures.
MRI of the shoulder joint with fat suppression. T2-weighted coronal MRI. Fracture of the greater tuberosity (arrow).
Indications for MRI of the shoulder joint
Suspected tear of the rotator cuff or proximal portion of the long head of the biceps brachii Injury in which a labral tear is suspected Traumatic changes in the shoulder joint leading to instability and typical humeral head fractures or impingement syndrome
In MRI of the shoulder, an indirect sign of a rotator cuff tear is a high T2-weighted signal from the surface of the joint to the subacromial (subdeltoid) bursa. Partial ruptures are most often along the anterior surface of the supraspinatus tendon, less often adjacent to the greater tuberosity or infraspinatus tendon.
MRI of the shoulder joint. T2-weighted coronal MRI. Subacromial fluid collection is an indirect sign of a rotator cuff tear.
MRI of the shoulder joint. T1-weighted coronal MRI. Partial tear of the rotator cuff.
MRI of the shoulder joint. T2-weighted coronal MRI. Anterior rotator cuff tear
MRI St. Petersburg allows you to choose the MRI location. MRI of the shoulder joint in St. Petersburg, Professor Kholin A.V. is carried out mainly on an open-type device in the CMR clinic. This provides high comfort for the patient, reasonable prices and the opportunity to consult a traumatologist.
Leave feedback.
MRI in St. Petersburg USA
What determines the price of a shoulder tomography?
The price of an MRI of the shoulder joint is largely determined by three factors: the power of the tomograph, the qualifications of the personnel and the need to use contrast. A good way to reduce diagnostic costs without losing the quality of the examination would be to use the MRI service at night, when the maximum discounts apply.
| Service | Price according to Price | Discount Price at Night | Discount Price During the Day |
| Shoulder MRI | 4000 rub. | 2990 rub. | 3690 rub. |
| Appointment with an orthopedist | 1800 rub. | free after MRI | free after MRI |
| First aid program for joints (8 studies + appointment with an orthopedist + MRI of the joint) | 13000 rub. | 7500 rub. | 7500 rub. |
What determines the cost of tomography?
![]()
Tomograph power
![]()
Applying Contrast
Personnel qualifications
![]()
Promotions and discounts