To determine a large number of bronchopulmonary diseases, a diagnostic method is needed that will allow assessing dysfunction of external respiration. This will allow you to find the area where the problem arose, assess the severity of the disease, and monitor the respiratory tract.
There are several techniques that can be used for this purpose. One of the most informative and at the same time safe methods for the patient is spirography or breathing spirometry. These are similar and interchangeable terms. The only difference is that the procedure itself is called spirometry, and the result (the result obtained) is called spirography. You can have a spirography done in Moscow and get a doctor’s consultation based on its results at the Kutuzovsky Children’s Center, a multidisciplinary medical center at 5 Davydkovskogo Street.
What spirography will show
The purpose of spirography is to estimate the volume of inhaled and exhaled air, to estimate the speed of air passage through the respiratory tract during inhalation and exhalation. A number of indicators obtained during spirography will help with this. The examination is used in medical fields such as therapy and pulmonology.
With the help of lung spirography, a number of important parameters are determined that make it possible to assess the characteristics of the respiratory system of the subject, diagnose diseases and develop optimal treatment tactics in a particular case. These are indicators such as the volume of air in the lungs, the volume of air inhaled per minute, respiratory rate, air remaining after exhalation and other indicators.
Spirography and assessment of pulmonary pulmonary function helps in assessing:
- Airway patency.
- The severity and other characteristics of existing diseases.
- The presence of characteristic signs of diseases such as asthma, COPD, pulmonary spasms.
- The effectiveness of therapy and rehabilitation.
Spirography is a method of graphically recording changes in lung volumes during natural respiratory movements and volitional forced respiratory maneuvers. Spirography allows you to obtain a number of indicators that describe lung ventilation. First of all, these are static volumes and capacities that characterize the elastic properties of the lungs and chest wall, as well as dynamic indicators that determine the amount of air ventilated through the respiratory tract during inhalation and exhalation per unit time. Indicators are determined in the mode of quiet breathing, and some - during forced breathing maneuvers.
In technical terms, all spirographs are divided into open and closed type devices (Fig. 1). In open-type devices, the patient inhales atmospheric air through a valve box, and the exhaled air enters a Douglas bag or a Tiso spirometer (capacity 100-200 l), sometimes to a gas meter, which continuously determines its volume. The air collected in this way is analyzed: the values of oxygen absorption and carbon dioxide release per unit of time are determined. Closed-type devices use the air from the bell of the device, circulating in a closed circuit without communication with the atmosphere. Exhaled carbon dioxide is absorbed by a special absorber.
Indications for spirography are as follows:
1. Determination of the type and degree of pulmonary insufficiency.
2.Monitoring of pulmonary ventilation indicators in order to determine the degree and speed of progression of the disease.
3.Evaluation of the effectiveness of course treatment of diseases with bronchial obstruction with bronchodilators, short- and long-acting β2-agonists, anticholinergics), inhaled corticosteroids and membrane-stabilizing drugs.
4. Carrying out differential diagnosis between pulmonary and heart failure in combination with other research methods.
5. Identification of initial signs of ventilation failure in persons at risk of pulmonary diseases, or in persons working under the influence of harmful production factors.
6.Expertise of performance and military examination based on assessment of pulmonary ventilation function in combination with clinical indicators.
7. Conducting bronchodilation tests to identify the reversibility of bronchial obstruction, as well as provocative inhalation tests to identify bronchial hyperreactivity.
Rice. 1. Schematic representation of a spirograph
Despite its widespread clinical use, spirography is contraindicated in the following diseases and pathological conditions:
- severe general condition of the patient, which makes it impossible to conduct research;
- progressive angina pectoris, myocardial infarction, acute cerebrovascular accident;
- malignant arterial hypertension, hypertensive crisis;
- toxicosis of pregnancy, second half of pregnancy;
- stage III circulatory failure;
- severe pulmonary insufficiency that does not allow breathing maneuvers.
Technique for performing spirography . The study is carried out in the morning on an empty stomach. Before the study, the patient is recommended to remain calm for 30 minutes, and also stop taking bronchodilators no later than 12 hours before the start of the study. The spirographic curve and pulmonary ventilation indicators are shown in Fig. 2. Static indicators are determined during quiet breathing. Tidal volume ( TI is measured - the average volume of air that the patient inhales and exhales during normal breathing at rest. Normally it is 500-800 ml. The part of the DO that takes part in gas exchange is called alveolar volume ( AO ) and on average equals 2/3 of the DO value. The remainder (1/3 of the DO value) is the volume of functional dead space ( FSD ). After a calm exhalation, the patient exhales as deeply as possible - the expiratory reserve volume ( ERV ) is measured, which normally amounts to IOOO-1500 ml. After a calm inhalation, the deepest possible breath is taken - the inspiratory reserve volume ( IRV ) is measured. When analyzing static indicators, the inspiratory capacity (Evd) is calculated - the sum of DO and ROvd, which characterizes the ability of lung tissue to stretch, as well as vital capacity of the lungs ( VC ) - the maximum volume that can be inhaled after the deepest exhalation (the sum of DO, ERVd and ROvd normally ranges from 3000 to 5000 ml). After normal quiet breathing, a breathing maneuver is performed: the deepest possible breath is taken, and then the deepest, sharpest and longest (at least 6 s) exhalation is taken. the forced vital capacity of the lungs ( FVC is determined - the volume of air that can be exhaled during forced exhalation after maximum inspiration (normally 70-80% of VC). , maximum pulmonary ventilation ( MVL is recorded - the maximum volume of air that can be ventilated by the lungs in 1 minute. MVL characterizes the functional capacity of the external respiration apparatus and is normally 50-180 liters. A decrease in MVL is observed with a decrease in pulmonary volumes due to restrictive (limiting) and obstructive disorders of pulmonary ventilation.
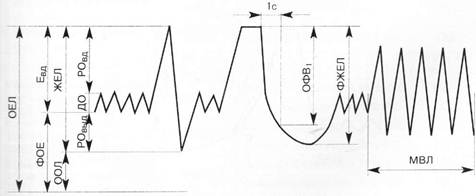
Rice. 2. Spirographic curve and pulmonary ventilation indicators
When analyzing the spirographic curve obtained in a maneuver with forced exhalation, certain speed indicators are measured (Fig. 3):
1) forced expiratory volume in the first second ( FEV1 ) - the volume of air that is exhaled in the first second when exhaling as quickly as possible; it is measured in ml and calculated as a percentage of FVC; healthy people exhale at least 70% of FVC in the first second;
Tiffno test or - the ratio of FEV1 (ml)/VC (ml), multiplied by 100%; normally it is at least 70-75%;
3) maximum volumetric air velocity at the expiratory level of 75% FVC ( MOC75 ) remaining in the lungs; 4) maximum volumetric air velocity at the expiratory level of 50% FVC (MOC50) remaining in the lungs; 5) maximum volumetric air velocity at the expiratory level of 25% FVC ( MOC25 ) remaining in the lungs; 6) average forced expiratory volumetric flow rate, calculated in the measurement interval from 25 to 75% FVC ( SOS25-75 ).
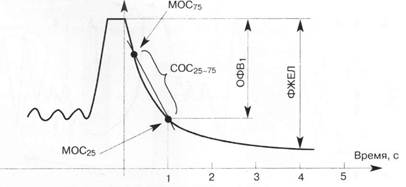
Rice. 3. Spirographic curve obtained in the forced expiratory maneuver. Calculation of FEV1 and SOS25-75 indicators
Calculation of speed indicators is of great importance in identifying signs of bronchial obstruction. A decrease in the Tiffno index and FEV1 is a characteristic sign of diseases that are accompanied by a decrease in bronchial patency - bronchial asthma, chronic obstructive pulmonary disease, bronchiectasis, etc. MOS indicators are of the greatest value in diagnosing the initial manifestations of bronchial obstruction. SOS25-75 displays the state of patency of small bronchi and bronchioles. The latter indicator is more informative than FEV1 for identifying early obstructive disorders. The indicators PSV and MSV 75 reflect the patency of large bronchi, and MSV 50 and MSV 25 reflect the patency of small bronchi.
Due to the fact that in Ukraine, Europe and the USA there is some difference in the designation of lung volumes, capacities and speed indicators that characterize pulmonary ventilation, we present the designations of these indicators in Russian and English (Table 1). It should also be emphasized that there is identity in the indicators of volumetric expiratory flow rates in different countries (Table 2).
Table 1. Name of pulmonary ventilation indicators in Russian and English
| Name of the indicator in Russian | Accepted abbreviation | Indicator name in English | Accepted abbreviation |
| Vital capacity of the lungs | vital capacity | Vital capacity | V.C. |
| Tidal volume | BEFORE | Tidal volume | TV |
| Inspiratory reserve volume | District Department of Internal Affairs | Inspiratory reserve volume | IRV |
| Expiratory reserve volume | ROvyd | Expiratory reserve volume | ERV |
| Maximum ventilation | MVL | Maximum voluntary ventilation | M.W. |
| Forced vital capacity | FVC | Forced vital capacity | FVC |
| Forced expiratory volume in the first second | FEV1 | Forced expiratory volume 1 sec | FEV1 |
| Tiffno index | IT, or FEV1/VC% | FEV1% = FEV1/VC% | |
| Maximum flow rate at the moment of exhalation 25% FVC remaining in the lungs | MOS25 | Maximum expiratory flow 25% FVC | MEF25 |
| Forced expiratory flow 75% FVC | FEF75 | ||
| Maximum flow rate at the moment of exhalation of 50% FVC remaining in the lungs | MOS50 | Maximum expiratory flow 50% FVC | MEF50 |
| Forced expiratory flow 50% FVC | FEF50 | ||
| Maximum flow rate at the moment of exhalation 75% FVC remaining in the lungs | MOS75 | Maximum expiratory flow 75% FVC | MEF75 |
| Forced expiratory flow 25% FVC | FEF25 | ||
| Average expiratory volumetric flow rate in the range from 25% to 75% FVC | SOS25-75 | Maximum expiratory flow 25-75% FVC | MEF25-75 |
| Forced expiratory flow 25-75% FVC | FEF25-75 |
Closing volume (CV) is the volume of gas remaining in the lungs when the small airways begin to collapse during maximal expiration (Mosby's Medical Dictionary, 8th edition. © 2009, Elsevier.).
Table 2. Name and correspondence of pulmonary ventilation indicators in different countries
| Ukraine | Europe | USA |
| mos25 | MEF25 | FEF75 |
| mos50 | MEF50 | FEF50 |
| mos75 | MEF75 | FEF25 |
| SOS25-75 | MEF25-75 | FEF25-75 |
All indicators of pulmonary ventilation are variable. They depend on gender, age, weight, height, body position, the state of the patient’s nervous system and other factors. Therefore, for a correct assessment of the functional state of pulmonary ventilation, the absolute value of one or another indicator is insufficient. It is necessary to compare the obtained absolute indicators with the corresponding values in a healthy person of the same age, height, weight and gender - the so-called proper indicators. This comparison is expressed as a percentage relative to the proper indicator. Deviations exceeding 15-20% of the expected value are considered pathological.
SPIROGRAPHY WITH REGISTRATION OF THE FLOW-VOLUME LOOP
Spirography with registration of the flow-volume loop is a modern method for studying pulmonary ventilation, which consists in determining the volumetric speed of air flow in the inhalation tract and graphically displaying it in the form of a flow-volume loop during quiet breathing of the patient and when he performs certain breathing maneuvers . Abroad, this method is called spirometry . The purpose of the study is to diagnose the type and degree of pulmonary ventilation disorders based on the analysis of quantitative and qualitative changes in spirographic parameters.
Indications and contraindications for the use of spirometry are similar to those for classical spirography.
Methodology . The study is carried out in the first half of the day, regardless of food intake. The patient is asked to close both nasal passages with a special clamp, take an individual sterilized mouthpiece into his mouth and tightly clasp his lips around it. The patient, in a sitting position, breathes through the tube along an open circuit, experiencing virtually no breathing resistance. The procedure for performing respiratory maneuvers with recording the flow-volume curve of forced breathing is identical to that performed when recording FVC during classical spirography. The patient should be explained that in a test with forced breathing one should exhale into the device as if one were to extinguish the candles on a birthday cake. After a period of quiet breathing, the patient takes a maximally deep breath, resulting in an elliptical curve (AEB curve) being recorded. Then the patient makes the fastest and most intense forced exhalation. In this case, a curve of a characteristic shape is recorded, which in healthy people resembles a triangle (Fig. 4).
Rice. 4. Normal loop (curve) of the relationship between the volumetric flow rate and air volume during breathing maneuvers. Inhalation begins at point A, exhalation begins at point B. POSV is recorded at point C. The maximum expiratory flow in the middle of the FVC corresponds to point D, the maximum inspiratory flow to point E
The maximum expiratory volumetric air flow rate is displayed by the initial part of the curve (point C, where the peak expiratory volumetric flow rate is recorded - POSP) - After this, the volumetric flow rate decreases (point D, where MOC50 is recorded), and the curve returns to its original position (point A). In this case, the flow-volume curve describes the relationship between the volumetric air flow rate and the pulmonary volume (lung capacity) during respiratory movements. Data on speeds and volumes of air flow are processed by a personal computer thanks to adapted software. The flow-volume curve is displayed on the monitor screen and can be printed on paper, saved on magnetic media or in the memory of a personal computer. Modern devices work with spirographic sensors in an open system with subsequent integration of the air flow signal to obtain synchronous values of lung volumes. The computer-calculated research results are printed together with the flow-volume curve on paper in absolute values and as a percentage of the required values. In this case, FVC (air volume) is plotted on the abscissa axis, and air flow, measured in liters per second (l/s), is plotted on the ordinate axis (Fig. 5).
Fiow-voiume Last name: Ident. number: 4132 Name: Date of birth: 01/11/1957 Age: 47 Years Gender: female Weight: 70 kg Height: 165.0 cm
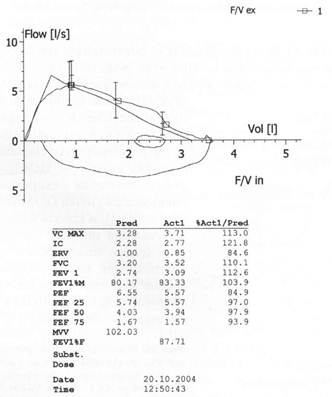
Rice. 5. Forced breathing flow-volume curve and pulmonary ventilation indicators in a healthy person
Rice. 6 Scheme of the FVC spirogram and the corresponding forced expiratory curve in “flow-volume” coordinates: V - volume axis; V' - flow axis
The flow-volume loop is the first derivative of the classical spirogram. Although the flow-volume curve contains essentially the same information as the classic spirogram, the visualization of the relationship between flow and volume allows deeper insight into the functional characteristics of both the upper and lower airways (Fig. 6). Calculation of highly informative indicators MOS25, MOS50, MOS75 using a classical spirogram has a number of technical difficulties when performing graphic images. Therefore, its results are not highly accurate. In this regard, it is better to determine the indicated indicators using the flow-volume curve. Assessment of changes in speed spirographic indicators is carried out according to the degree of their deviation from the proper value. As a rule, the value of the flow indicator is taken as the lower limit of the norm, which is 60% of the proper level.
Indications
Spirometry for adults is prescribed for:
- Protracted cough (longer than 20-30 days) with unknown causes or after suffering from acute respiratory viral infections or bronchitis.
- Diagnosis of diseases of the respiratory system and their differentiation from other diseases with similar symptoms (for example, to distinguish between heart and pulmonary failure, in which shortness of breath appears).
- The patient complains of a feeling of tightness in the chest, shortness of breath.
- Difficulty breathing (with whistling, wheezing).
- Constantly recurrent bronchitis and other diseases, when it is necessary to understand the rate of disease progression.
- The need to correct the prescribed course of treatment with bronchodilators, their selection, and evaluation of effectiveness.
- Planning surgical interventions on the lungs.
Spirometry with determination of lung volume is also used during preventive examinations for patients from risk groups for respiratory diseases: experienced smokers, workers in industries with harmful production factors (dusty working conditions), allergy sufferers (with manifestations of bronchospasms).
Spirometry is also mandatory for patients with the following diseases:
- Bronchial asthma.
- Pulmonary failure
- Chronic bronchitis.
- COPD and some others.
Spirometry: indications for performance
Spirometry is used mainly in pulmonology, less often in such areas of medicine as allergology and cardiology.
This study is indicated for patients in the following cases:
- if there are complaints from the respiratory system: chronic cough, shortness of breath, etc.);
- in case of changes in the organs of the respiratory system identified using other diagnostic methods;
- when gas exchange in the body is disrupted (with a decrease in oxygen content in the blood and an increase in carbon dioxide content);
- as a preparatory measure for other studies and surgical interventions (such as bronchoscopy, thoracotomy, etc.).
Spirometry also plays a key role in the diagnosis and differential diagnosis of COPD (chronic obstructive pulmonary disease) and bronchial asthma. The study is used to evaluate the effectiveness of their therapy.
Patients suffering from these pathologies should regularly (at least once a year) undergo spirometry in a medical facility, and at home monitor external respiration indicators with a special device - a peak flow meter.
In addition, spirometry is recommended for people whose work activities are associated with hazardous conditions, heavy smokers and allergy sufferers.
Contraindications
Spirography is a painless and harmless procedure. However, to carry it out, the participation of the subject is required - he needs to follow the doctor’s instructions, inhale, exhale at a certain speed and other actions. Therefore, the examination will be difficult for young children (under five years old) or patients with mental disorders.
Other contraindications for spirometry:
- Acute form of cardiovascular diseases (heart attack, stroke, angina).
- Significantly elevated blood pressure.
- Third trimester of pregnancy (the study may not be very informative due to compression of the internal organs by the growing uterus).
- A severe form of pulmonary failure, in which it will be difficult for the patient to follow the doctor’s instructions and perform functional tests (quick exhalation and other maneuvers).
Interpretation of results
Upon completion of data collection, they are analyzed in order to draw up a diagnostic conclusion. In the process of interpreting all the obtained indicators, an electronic spirogram is generated by a computer program. The following values are interpreted.
Respiratory rate (RR)
The number of respiratory movements in one minute is recorded. Its normal values do not exceed 16–17 times.
Tidal volume (TO)
The volume of air filling the lungs with one breath is determined. Its normal values have a fairly wide range. The limits for healthy men can fluctuate between 300–1200 ml, and for healthy females values within the range of 250–800 ml are typical.
Minute respiration volume (MRV)
Shows the volume of air absorbed by the lungs in 1 minute. It also has a relatively large interval and ranges between 4–10 liters.
Vital capacity of the lungs (VC)
This value is studied when determining the maximum volume of air exhaled by the subject during a quiet exhalation after the deepest inhalation.
Forced vital capacity (FVC)
The maximum volume of air exhaled by the patient during the deepest (forced) exhalation after the same inhalation is diagnosed. Normally, for individuals this figure ranges from 2.5 to 7.5 liters.
Forced expiratory volume in 1 second (FEV1)
The maximum volume of air exhaled by a person in 1 second during a deep exhalation after an extremely deep inhalation is determined. Its value is significantly influenced by the gender and age of the subject.
Tiffno Index (IT)
Its value is the ratio FEV1/FVC, and is expressed as a percentage.
Maximum ventilation (MVV)
This value is obtained by multiplying the average amplitude of extreme respiratory excursions and their frequency in 1 minute.
Air velocity indicator (ASMV)
This value looks like MVL/VC, and is indicated as a percentage.
Preparation
It is necessary to obtain more accurate data when assessing external respiratory function; preparation is recommended. Here's what the doctor will advise:
- Come for examination on an empty stomach or 2-4 hours after eating (preferably a light snack rather than a heavy lunch or dinner). Avoid strong tea, coffee and other caffeine-containing drinks, alcohol, and smoking. If you are thirsty, the patient can drink a glass of water at room temperature no later than an hour before the procedure.
- Stop taking bronchodilators on the day of the test or the day before. Taking other medications should be discussed with your doctor.
- It is better not to do morning exercises and limit other physical activities.
- Wear loose clothing that does not constrict the body and does not interfere with free breathing.
- Come to the clinic 15-30 minutes in advance to restore your breathing rate and normalize the functioning of your respiratory and cardiovascular systems.
The patient also needs to know his height and weight for calculations and analysis of results.
Research methodology
To take a spirogram, the patient must be seated as comfortably as possible. His clothing should not compress the chest and interfere with free breathing. The seat on which the subject sits and the oral tube are installed in accordance with his height, so that he does not have to bend over or stretch his neck upward. You also need to control the position of your torso when exhaling - do not let your body lean forward.

When performing spirography, it is necessary to sit the patient so that it is comfortable for him to perform breathing tests
The test analyzes oral airflow measurements and requires the patient to use a nose clip and hold the mouthpiece tightly to prevent air leakage. If the subject has dentures installed, they cannot be removed, as this will disrupt the quality fixation of the mouthpiece.
First, several primary tests are carried out - measuring tidal volume (TI), which is calculated based on the average of six or more respiratory cycles at rest. Then, in a calm state, the respiratory rate (RR) is determined. The product of these values will give the minute volume of breathing. A new type of spirograph, equipped with software, automatically provides all calculations.
The spirograph processes information immediately during the study and produces a tape with recorded results. At the signal from the diagnostician, the examinee inhales as completely as possible, and then exhales as sharply and as long as possible. The exhalation time should take at least 6 seconds and the patient should maintain maximum effort throughout the exhalation until completion.
Often, individuals undergoing testing are unable to inhale and exhale properly the first time, so the test is carried out using several attempts under the control of a recorded curve. Then the subject needs to breathe with maximum depth and frequency for 12 seconds. In certain cases, in some patients, such tests can cause dizziness, “floaters” before the eyes or darkening and even fainting, but the latter conditions are diagnosed quite rarely.
How is pulmonary function assessed?
In diagnostic and treatment spirometry is carried out using special equipment - a spirograph. This is a digital device that allows you to determine the required indicators in different modes and automatically calculates the necessary ratios. The use of such a device makes the procedure faster and easier compared to examinations using mechanical spirographs that were once used. The program takes into account the weight, height, gender, and age of the patient in the calculations.
During the procedure, the patient needs to breathe calmly and measuredly, and when performing functional tests, the doctor will ask you to make strong and quick exhalations to determine the volume of the lungs.
Spirometry is performed as follows:
- The patient sits comfortably, his nose is closed with a soft clamp to limit nasal breathing.
- A disposable attachment is placed on the device - a mouthpiece, which the person being examined needs to tightly clasp his lips.
- Breathing passes through the mouth. It is necessary to breathe at a calm pace for 10-15 seconds - 3-4 breathing cycles (inhale-exhale). In this case, the correct posture of the patient is important - sit upright, without straining or stretching the head and neck.
- During testing, the doctor will ask you to take deep, and later frequent, inhalations and exhalations.
Breathing indicators (air volume, air flow speed, number of movements) are recorded, and measurements are taken several times to eliminate errors due to loose contact of the mouth with the mouthpiece and other reasons.
If diagnostics with a bronchodilator drug is necessary, then after completing standard spirometry, the patient is inhaled with a special device using a special device. 20-30 minutes after this, repeated spirography is performed.
To examine lung function in athletes or when patients complain of shortness of breath during exercise, functional exercise tests are performed. The test procedure is similar to standard spirometry, the difference being that the patient exercises on an exercise bike or treadmill during testing.
If necessary, functional tests can be done during spirometry. It can be:
- Spirometry with a bronchodilator makes it possible to more accurately identify hidden bronchospasms and is used to assess the effectiveness of the course of therapy.
- A test with methacholine, which will help to definitively confirm or refute bronchial asthma by identifying the predisposition of the bronchi to spasms.
The study lasts from 15 minutes to an hour (the duration varies with different research methods). When all the data is received, the program prepares the result in the form of a graph (spirogram). If some indicators are not normal, the procedure may be repeated or spirography with a bronchodilator may be prescribed.
Spirometry: contraindications
Spirometry is contraindicated in patients with the following conditions:
- pneumothorax;
- bleeding from the respiratory tract;
- tuberculosis;
- dissecting aortic aneurysm;
- hypertensive crisis;
- previous myocardial infarction;
- ischemic and hemorrhagic stroke;
- in the postoperative period after ophthalmological or intracavitary surgical interventions (in the first 1.5 months);
- mental disorders (if the patient is unable to follow the recommendations of the diagnostician regarding the quality and speed of breathing during the procedure).
The decision on the need and advisability of conducting the study is made solely by the attending physician. He evaluates the safety of spirometry in each specific case, identifies contraindications to the test, and determines whether they are absolute or relative.
Decoding the results of spirography
The doctor sees the results as soon as the study is completed. The data is interpreted depending on the individual characteristics of the patient: gender, age, weight. The obtained parameters are compared with the norm values. A difference from the reference values may indicate that there are bronchopulmonary pathologies, there may be oxygen deficiency in the brain and disruption of its functioning. To exclude cardiovascular diseases as the root cause of dysfunction of the bronchopulmonary system, an ECG, ultrasound of the heart and other examinations can be performed along with spirography.
When should you get tested?
Indications for spirometry may include:
1) subjective respiratory symptoms (shortness of breath, prolonged cough, sputum production, chest pain);
2) objective signs of respiratory pathology (wheezing in the lungs, changes in laboratory parameters, “poor radiograph”);
3) sensitization to various allergens (hay fever, allergic rhinitis, conjunctivitis, atopic dermatitis, etc.), since these nosologies are a risk factor for the development of bronchial asthma;
4) an established diagnosis of bronchopulmonary disease (to select the optimal treatment regimen and monitor the course of the disease);
5) identified cardiovascular, musculoskeletal and neurological pathologies;
6) long-term exposure to unfavorable factors on the body (smoking, poor environmental conditions, work in hazardous industries, etc.);
7) for the purpose of assessing professional suitability (pilots, military personnel, athletes).
Spirometry in Moscow
A study of external respiration function or spirography in Moscow can be done daily at the Kutuzovsky Children's Center by appointment. Our advantages:
- Affordable spirography price.
- A wide range of services - from various diagnostic methods to consultations with doctors of various specialties.
- Comfortable conditions for examinations - no queues, no waiting, in a modern medical center.
Contact our specialists by phone to make an appointment, find out the price of spirometry for adults, assessment of pulmonary function in Moscow or the cost of other procedures and make an appointment at a convenient time.
Executing the procedure
The patient is in a comfortable position, arms are relaxed on the armrests. To ensure only mouth breathing, the nose is blocked with a special clip. A tube with a disposable sterile tip (mouthpiece) is inserted into the mouth. At the beginning of the procedure, the patient breathes naturally and evenly.
The indicator DO is determined - tidal volume. The patient is then asked to take a normal breath and exhale all the air as quickly as possible. This will be the indicator of expiratory reserve volume (ERV).
The duration of exhalation with maximum effort of more than 15 seconds is a reason to diagnose pathology. Then the maximum breathing capacity is measured.
You should inhale as deeply as possible (reserve inspiratory volume - ROVD and vital capacity of the lungs - VC are recorded) and rapidly exhale (FEV and FVC are determined).
The device automatically builds a graph based on the measurement readings. FEV indicators have diagnostic significance.
The shape of the loop shown allows you to diagnose the type of respiratory failure:
- obstructive;
- restrictive;
- mixed.
The reversibility of obstruction is determined by the data of a test with bronchodilators. FEV readings are of primary comparative importance.
Each test is carried out several times (usually 3 times). After this, the most successful ones are selected.
The device produces the result of a spirogram, according to which the doctor evaluates a specific case and makes a conclusion. The procedure takes about 15 minutes. How many times and with what frequency the diagnosis is carried out is determined by the treating pulmonologist according to the indications.
Is it possible to do spirography for children?
Spirography can also be done for children from 5 years old. True, it happens that it is difficult to explain to a child how to breathe correctly, in this case it is better to double-check the results.
By the way, our sanatorium even accepts babies under one year old! There are specially designed children's programs. We have already told you why sanatorium treatment is important even for the little ones.
Now we understand more about the prevention of all kinds of diseases, and about spirography and what kind of procedure it is.