Introduction
Ureaplasmas received their name due to the ability to break down urea in urine under the action of the produced enzyme urease (urina - urine, translated from Latin).
In the genus Ureaplasma spp there are two species – Ureaplasma urealyticum and Ureaplasma parvum. Differences between ureaplasmas and obvious pathogens
(sexually transmitted infections)
- found in 50-70% of healthy people
- may be detected in children
- often detected in only one of the two partners
- as a rule, they are very difficult to treat and are often diagnosed again after 2-3 courses of antibiotic therapy
Ureaplasmosis
ECO
18018 October 12
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Ureaplasmosis: causes, symptoms, diagnosis and treatment methods.
Definition
Ureaplasmosis is a disease caused by certain types of ureaplasma (
Ureaplasma urealyticum
and
Ureaplasma parvum
) and affecting the genitourinary system.
WHO annually records an increase in the number of cases of proven sexually transmitted infections around the world. The number of combined infections (when several pathogens are detected in the analysis) is also growing, which significantly complicates the diagnosis, the course of the disease itself, and its treatment. In the case of ureaplasmosis, barrier contraception (use of condoms) is one of the most effective methods of preventing sexually transmitted diseases.
Causes of ureaplasmosis
Ureaplasmas are microorganisms prone to intracellular parasitism, which leads to certain nuances in the treatment of the disease they cause.
Due to their small size, ureaplasmas are in the gradation of microorganisms between viruses and bacteria, and actively multiply on the mucous membranes, especially the reproductive system.
Risk factors for this disease are:
- Promiscuity and unprotected sex.
- Failure to comply with personal hygiene rules.
- Using other people's hygiene products.
- Conditions leading to a decrease in immunity (both local and general): viral diseases, hypothermia, stressful situations, unbalanced nutrition and unfavorable environmental conditions, bad habits, exposure to radiation, uncontrolled use of hormonal drugs or antibiotics.
Routes of transmission of ureaplasma
- Sexual transmission is the most common way of transmitting this infection. In 20–40% of cases, the disease does not manifest itself with any symptoms; in such situations, the person is a carrier and distributor of pathogenic microorganisms.
- The vertical path is from an infected mother to a child, including when microorganisms enter the amniotic fluid or when the fetus passes through the birth canal.
- The least proven is the contact and household route of transmission of infection: in swimming pools, through toilet seats, through common hygiene items.
Classification of the disease
There is no generally accepted classification of this disease. Conventionally, several gradations of ureaplasmosis are distinguished.
By pathogen:
- caused by Ureaplasma urealyticum (an opportunistic microorganism), its presence in the body, not exceeding normal values, does not require treatment;
- caused by Ureaplasma parvum requires therapy.
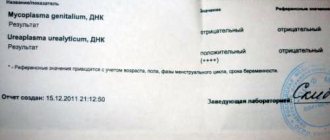
It is possible to clarify the type of pathogen that caused the disease only by performing a polymerase chain reaction (PCR).
By duration:
- spicy;
- chronic.
Symptoms of ureaplasmosis
The incubation period of ureaplasmosis usually lasts about one month. However, the disease may be latent (hidden) in nature and not manifest itself for many years if the patient has a stable immune system and normal microflora of the urogenital tract. Ureaplasma begins to multiply rapidly when the ratio of various microorganisms is disrupted.
In men, ureaplasma causes the following symptoms:
Inflammation of the urethra (urethritis), manifested by discomfort and unpleasant sensations in the urethra, burning and stinging during urination, as well as during sexual intercourse and ejaculation.
Slight mucous discharge from the urethra, more pronounced after a night's sleep or long abstinence from urination.
Orchitis, epididymitis - inflammation of the testicles, manifested by a feeling of fullness and discomfort in them, develops in cases of severe infection.
Prostatitis occurs when the infection tends to become chronic and signals that ureaplasma is actively spreading throughout the genitourinary system. It manifests itself as pain in the perineum, decreased libido, impaired and deteriorating erection.
In the absence of proper treatment, it causes the formation of adhesions in the genitourinary tract, which leads to urination problems and infertility.
In rare cases, a clinical picture of sore throat (pain in the throat when swallowing and at rest) may be observed as a result of ureaplasma entering the pharyngeal mucosa during oral-genital sex.
Women experience the following symptoms of the disease:

Stinging and burning when urinating may indicate the development of urethritis.
Vaginal discharge is scanty, mucous, frequent urge to urinate.
Due to mechanical irritation of the inflamed vaginal mucosa, sexual intercourse becomes painful, and bleeding may occur after it.
In cases of infection penetration into the uterus and fallopian tubes, painful sensations appear in the lower abdomen.
A sore throat, reminiscent of a sore throat, occurs when an infection penetrates the mucous membrane of the throat through oral-genital contact.
Diagnosis of ureaplasmosis
To make a diagnosis, it is necessary to determine the DNA of ureaplasmas in various biological media: in urine, prostate secretion.
Story
Microorganisms of this genus were discovered in the mid-20th century while studying bacteria living in the genitourinary tract. At the same time, it was suggested that they might be involved in the development of inflammation in this area in some cases. Then nothing was heard about them for several decades. This is due to the fact that, being small in size and unable to grow on nutrient media, there was no possibility of diagnosing them in practical medicine. And only with the advent of the PCR (polymerase chain reaction) diagnostic method in the 80s, they began to be identified and treated abroad. This was convenient for doctors, since sometimes not understanding the true cause of inflammation in the genitourinary organs, ureaplasma was almost always detected and was the basis for prescribing antibacterial therapy.
However, over time, their frequent detection and repeated presence in control tests after treatment made scientists think about the true pathogenicity of these microorganisms. Articles of that time talking about possible involvement in infertility, miscarriage, fetal pathology, inflammation in the genital organs did not have scientific validity and statistical evidence. Since approximately 2000, most progressive countries in Europe and North America have not carried out examination and treatment of ureaplasmas, considering them to be normal endogenous (internal) flora, which is often detected even in children.
Treatment of ureaplasmosis
It’s worth mentioning one important point right away - treatment of ureaplasmosis should be carried out according to the following rules:
- Treatment is prescribed to both partners at the same time, and the appointment of treatment should be preceded by a full diagnosis.
- If concomitant infectious diseases are detected, treatment is prescribed according to an individual scheme depending on the identified spectrum of infections.
- During the treatment period, any sexual contact is prohibited, including using barrier methods of protection.
- The treatment carried out requires a follow-up examination to diagnose cure within the time frame established by the doctor.
Immune stimulation
In order to effectively fight ureaplasma infection, antibiotics alone are not enough. After all, antibacterial agents only help the immune system cope with bacteria that harm the body. Therefore, whether a complete cure will occur depends largely on the state of the immune system. To stimulate the immune system, it is necessary to adhere to a rational regime of work and rest, the diet must be balanced and contain easily digestible protein, vegetable fats and vitamins A, B, C and E. Also, to stimulate the immune system, medications are often used - such as Immunal or St. John's wort tincture .
Adequate treatment of infectious and inflammatory diseases is possible only under the supervision of a specialist attending physician!
Official information
Below, I quote verbatim excerpts from the fundamental document that should guide doctors (dermatovenereologists, gynecologists, urologists) in matters of diagnosis and treatment of ureaplasma. (Author's note - this document is in the public domain and can be easily found on the Internet)
“Federal clinical guidelines for the management of patients with urogenital diseases caused by Ureaplasma spp, Mycoplasma hominis”, Moscow, 2015.
Recommendations were developed by the Russian Society of Dermatovenereologists and Cosmetologists and the Russian Society of Obstetricians and Gynecologists.
Code according to the International Classification of Diseases (ICD-10) – A63.8 – Other specified diseases transmitted predominantly
sexually. (Author's note - the operative word here is "primarily")
Cause and epidemiology
Mycoplasma hominis and Ureaplasma spp. – opportunistic microorganisms that, when realizing their pathogenic properties, can cause urethritis (U.urealyticum), cervicitis (inflammation of the cervix), cystitis, pelvic inflammatory disease (PID), as well as complications during pregnancy and post-abortion complications.
For me personally, the big question is how to reliably determine that a pregnancy complication is caused by the presence of ureaplasmas, if statistically they occur in 50-70% of people.
The frequency of detection of Ureaplasma varies widely in different population groups, ranging from 10% to 50% (according to some authors - up to 80%, while usually true pathology does not exceed 10%). (Author's note - usually true pathology does not exceed 10%)
WHO experts (World Health Organization, 2006) identified U.urealyticum as a potential causative agent of urethritis in men, and possibly PID in women. At the same time, experts from the US Centers for Disease Control and Prevention (CDC, 2010) do not consider the presence of ureaplasma to be proven as a cause of the development of inflammatory processes in the genitourinary system.
Symptoms of ureaplasma
Among women:
- mucopurulent discharge from the genital tract
- itching, burning, pain when urinating
- pain during sexual intercourse
- discomfort and pain in the lower abdomen
- swelling and redness of the vaginal and cervical mucosa
Classic signs of inflammation of the external genitalia and pelvic organs are described!
For men:
- mucopurulent discharge from the external opening of the urethra
- itching and burning in the urethra when urinating
- pain during intercourse
- frequent urination
- pain in the perineum
- swelling and redness of the external opening of the urethra
Classic symptoms of urethritis and prostatitis are described. In 18 years of my practice, I have never seen a patient have these symptoms and during the examination only ureaplasma was detected!!!
Analysis for ureaplasma parvum in women
Now you know how to test for ureaplasma in men. It remains to be seen how this procedure works in female patients.
Read also: How to make a smear
There are no particular differences in the collection of clinical material from the urethra.
You can also take PCR tests for ureaplasma from the vagina. To do this, the doctor inserts a gynecological speculum moistened with warm water. Then, using a swab or disposable loop, collects material from the side and back walls.
A smear is also taken from the cervix. To do this, a probe is inserted into the cervical canal. Before this, it is cleared of vaginal secretions.
Diagnosis of ureaplasma
Indications for examination for Ureaplasma spp.
is the presence of clinical and laboratory signs of an inflammatory process in the area of the urogenital tract and reproductive system, vaginal dysbiosis in the absence of pathogenic pathogens.
I translate into Russian - if there are no complaints and no signs of inflammation in the genitourinary organs, there is no need to be examined for ureaplasma.
If there are complaints and signs of inflammation, then men are first examined for STIs (sexually transmitted infections - chlamydia, mycoplasma genitalium, gonorrhea, trichomonas), women - STIs, thrush, bacterial vaginosis, aerobic vaginitis. And if only after this examination it is not possible to identify the cause of the inflammation, then by the method of exclusion we can assume that this inflammation is caused precisely by ureaplasmas and suggest being examined for them.
In the absence of clinical and laboratory signs of the inflammatory process, the following are subject to examination:
- sperm donors
- patients diagnosed with infertility
- patients with a history of miscarriage and perinatal losses
Considering the difficulty of identifying the true causes of infertility and miscarriage, the wariness of doctors around the world in prescribing antibiotics in cases where there are no absolute indications for this, in this case I consider the prescribing of antibacterial drugs to be a greater evil than a benefit.
Features of ureaplasmosis during pregnancy:
- A pregnant woman has a reduced immune system. Even if ureaplasma is present in the body in small quantities, it can cause an infection.
- Antibiotics should not be taken in early pregnancy. Antibacterial drugs have side effects and can negatively affect the fetus.
- Against the background of reduced immunity, ureaplasmosis opens the gates to sexually transmitted infections. If a woman becomes infected with an STD, this will have an even more negative impact on the course of pregnancy.
Possible complications of ureaplasmosis during pregnancy:
- Miscarriage. In the early stages, the disease can lead to miscarriage.
- Premature birth. The child is born premature and weakened. This occurs due to the fact that with ureaplasmosis the cervix loosens. It can be sutured, but this can also negatively affect the child’s condition.
- Violation of uteroplacental blood flow.
- Hypoxia (oxygen starvation) of the fetus.
- Intrauterine developmental delay.
Features of treatment of ureaplasmosis during pregnancy:
If pregnancy proceeds without complications against the background of infection, and there is no threat of miscarriage, then treatment is prescribed from the 22nd week. At earlier stages, there is a high risk of negative effects of antibiotics on fetal development. Antibacterial drugs from the macrolide group (erythromycin) are usually used in combination with immunotherapy (thymalin, T-activin) and probiotics (lactusan, colibacterin, bifidumbacterin). Treatment is selected individually. Your doctor may also prescribe other medications.
If the infection develops early in pregnancy, it can lead to serious damage to the fetus, missed abortion, and miscarriage.
At later stages, fetoplacental insufficiency and fetal hypoxia develop. The child is born prematurely, underweight, and weakened. If the fetus experiences severe oxygen starvation, then the child may subsequently develop mental disorders.
There is evidence that ureaplasma can disrupt the development of the nervous system. Because of this, in the past, doctors often recommended induced termination of pregnancy for infected women. Today the tactics have changed.