Transthoracic lung biopsy - what is it?
Transthoracic biopsy as a diagnostic method has undeniable advantages:
- Simplicity;
- Rapidity;
- High information content.
Using it, the doctor can accurately diagnose diseases of the lungs, as well as other organs of the chest cavity.
In short, the essence of the study is that a needle is inserted into the patient’s lung, into the pathological focus, to take a tissue sample (biopsy), and then send it for histological analysis.
A procedure is performed to take a biopsy using CT or MSCT. Such control increases the already high accuracy of the technique.
Kinds
Today, doctors use three types of transthoracic examination:
- Aspiration;
- Open;
- Video assisted.
The first type is resorted to when the focus of the disease is localized near the chest wall. Indications for use are solitary tumors and disseminated lung lesions.
When conducting an open examination, an incision is made into the chest wall, which is more traumatic and can be considered a full-fledged surgical procedure. The advantages are the possibility of taking a biopsy from a large area of the lung and the fact that the depth of the location of the pathological focus does not matter.
The video-assisted version is used using an endoscope, which is inserted into the pleural cavity. The device is equipped with a video camera and special tools. Compared to the previous option, this approach does not require significant incisions and, accordingly, it is less traumatic.
The choice of one option or another depends on a number of factors, including the general condition of the patient, the type of lung injury, and the depth of the location of the source of the disease.
results
The final histological diagnosis by transthoracic biopsy of the mediastinum under ultrasound control was established in 67 (84%) patients out of the total number of patients.
A malignant tumor was diagnosed in 57 (85%) patients; in 10 (15%) cases the process was benign. The spectrum of nosological units is presented in table. 1.
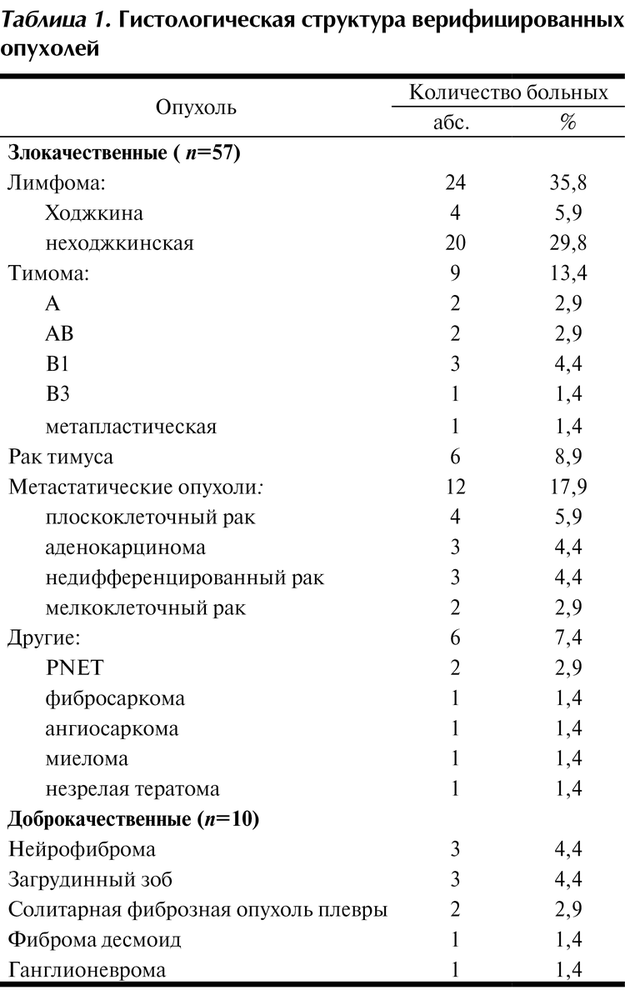
Table 1. Histological structure of verified tumors
5 (56%) biopsies were examined by immunohistochemistry (IHC). The most common indication for performing IHC studies was tumor immunophenotyping in lymphoproliferative diseases and differential diagnosis between metastases of malignant tumors.
In 19 (23.6%) patients in 21 biopsies, the presented material turned out to be uninformative. Among them, the overwhelming majority of differential diagnoses were between thymoma and lymphoma (17 biopsy specimens). In 16 cases, there was not enough material for full immunophenotyping of the tumor.
Repeated biopsies were performed in 7 patients, which made it possible to establish a final diagnosis in 6 cases: 3 patients with lymphoma, 1 with mediastinal neurofibroma, 1 with metastatic lesions of the mediastinal lymph nodes, and 1 with thymoma.
Due to the ineffectiveness of transthoracic biopsy, 13 patients underwent diagnostic parasternal mediastinotomy and open tumor biopsy. In all cases, a final diagnosis was made (Table 2).
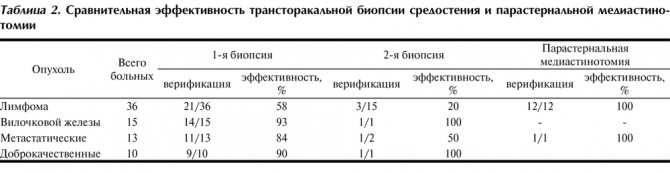
Table 2. Comparative effectiveness of transthoracic mediastinal biopsy and parasternal mediastinotomy
In the group of patients with an established morphological diagnosis by ultrasound-guided transthoracic biopsy ( n
=67) the average number of biopsy cores obtained was 1.59 (from 1 to 4), the average core size was 11 mm (from 1 to 33 mm), whereas in the group of patients whose biopsy was uninformative (
n
= 21), the average number of columns obtained was 1.36 (range 1 to 3), the average column size was 6 mm (range 4 to 14 mm).
significant statistical differences were found in the number of cores obtained ( p
= 0.36) and the total size of biopsy specimens (
p
= 0.1).
Of the 35 patients with an echographic picture of damage to the mediastinal lymph nodes due to lymphoma, the final diagnosis of lymphoproliferative disease was made in 29 cases, in 6 patients other diseases were verified. Of the 45 patients in whom a different diagnosis was clinically suggested, lymphoma was verified in 7 cases. The sensitivity of transthoracic ultrasound-guided mediastinal biopsy for lymphoma was 81%, the specificity was 86%, and the diagnostic accuracy of the method was 84%. Among 22 patients with an echographic picture of a tumor of the thymus, a true diagnosis was made in 12 cases, in 10 another disease was verified. Of the 45 patients examined for another disease, 5 were diagnosed with thymoma or thymic cancer. The sensitivity of transthoracic ultrasound-guided biopsy for thymoma and thymic cancer was 70%, the specificity was 80%, and the diagnostic accuracy of the method was 77% (Table 3).
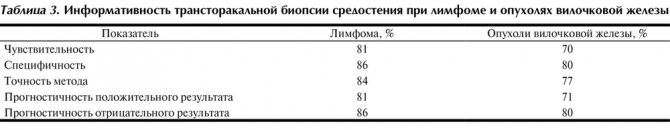
Table 3. Information content of transthoracic mediastinal biopsy for lymphoma and tumors of the thymus
No complications were noted after transthoracic ultrasound-guided biopsy of the mediastinal tumor.
Contraindications
Contraindications to the study are:
- Uncontrollable cough;
- Significant cardiovascular diseases;
- Decompensated respiratory failure;
- Damage to the lungs by metastases;
- Inability of the patient to maintain a static position throughout the procedure
- The final stage of diffuse lung disease, some others.

Radiography
What after?
The patient receives doctor's recommendations regarding the recovery period. Usually this period proceeds quickly and easily and does not require serious restrictions.
The results of the study are ready a week to ten days after the procedure. This is quite long because the process of preparing sections is labor-intensive. In addition, sometimes there is a need to clarify the diagnosis using immunohistochemistry.
Having received the conclusion from the laboratory, the doctor makes a final diagnosis and prescribes the necessary treatment.
Preparation and execution
Before conducting the study, the doctor must explain to the patient what risks and complications may occur.
The doctor needs to know the full picture of the patient’s health – whether there are blood diseases, prostheses and implants, allergies, etc.
The patient himself must prepare for the procedure in advance. He needs to not eat food 6-8 hours before, stop taking certain medications, such as Aspirin, and remove lenses and jewelry.
If the patient has a chronic cough and bloody sputum, the procedure is performed through a bronchoscope, which is inserted either through the mouth or nose.
Local anesthesia is used for pain relief; general anesthesia is used for open and video thoracoscopy.
In the case of sarcoidosis, the study plays the role of the main diagnostic procedure. The doctor, having the results of histological analysis in hand, is able to assess the degree of tumor development and prescribe appropriate treatment.
If a lung tumor is suspected, the doctor prescribes bronchoscopy and a percutaneous puncture biopsy. CT control is used.
The following types of needles are used to take a biopsy:
- Aspiration (diameter 21G). Using it, a cell biopsy is taken, which is necessary for cytological analysis.
- Trephination (diameter 14G). There is a plug inside the needle. When a needle is inserted into the swollen tissue, the plug is removed and a stylet is inserted into the resulting lumen. They use it to pinch off a biopsy sample necessary for histological examination.
After removing the needle, the puncture is covered with a bandage. In addition, the patient is given a chest x-ray to rule out pneumothorax.
The open version of the study is carried out under general anesthesia. An incision up to 8 centimeters long is required in the 3rd-4th intercostal space.
A suture or staples are placed on the incision area, and then the lung tissue is cut off. After the manipulation, a drainage is installed, the incision site is closed with a suture and a sterile bandage.
The intervention is quite traumatic, but it is possible to visualize the process, as well as take a significant fragment for research.
The qualifications and experience of the doctor play an important role in conducting the study.
Sarcoidosis - inflammation of the respiratory system
05.08.2020
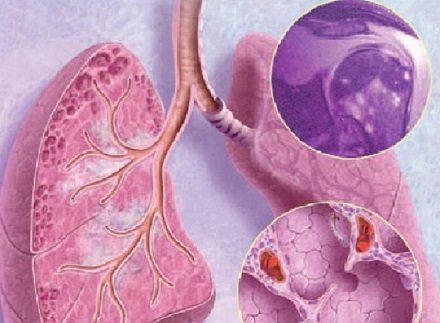
Sarcoidosis is an uncommon systemic disease that affects structures located in the chest cavity: lymph nodes and lungs, in which clusters of granulomas form. These neoplasms can subsequently either disappear or turn into scar tissue. Due to the localization of pathological changes, sarcoidosis is most often seen by TB specialists and pulmonologists .
The conditions and causes of the disease are unknown, which causes difficulties in investigating patterns of spread, diagnosis and treatment. Usually two versions of the appearance of sarcoidosis :
- multifactorial nature of the disease;
- relationship between sarcoidosis and tuberculosis.
The disease can be provoked by infections caused by fungi, bacteria and viruses in individuals predisposed to developing an inflammatory reaction to them.
Symptoms of sarcoidosis
As a rule, the disease proceeds with the gradual appearance of symptoms and clinical manifestations that occur at different stages, depending on the form, phase, and duration of the disease. to distinguish sarcoidosis from other diseases and can only be detected on an x-ray. To confirm the disease, in difficult cases, it is possible to use lung biopsy examination methods. Symptoms can be general (weakness, increased body temperature, weight loss) or associated with damage to organ tissue. Often the disease affects the skin . In 70% of patients, accumulations of inflammatory cells form in the liver . in the blood and urine increases. Visible symptoms appear in later stages:
- chest pain;
- pulmonary fibrosis and other respiratory disorders;
- coughing up blood ;
- fast fatiguability;
- dyspnea;
- dry cough;
- joint pain .
Diagnosis of the disease
The diagnostic stage is important because pulmonary sarcoidosis sarcoidosis of the intrathoracic lymph nodes must be distinguished from other diseases. Therefore, each case is considered separately.
When diagnosing sarcoidosis, the following types of examination are used:
- bronchoscopy;
- CT scan;
- MRI of the lungs;
- radiography;
- general blood ;
- biopsy.
At the stage of diagnostic measures, the patient is observed for six months or more. During this period, the diagnosis is clarified and a decision is made on treatment.
Methods and methods of treatment
To combat the disease, the patient is prescribed to take antioxidants, immunosuppressants, steroids and anti-inflammatory drugs. The use of hormonal therapy . Vitamin preparations play an important role in treatment to normalize metabolic processes. During the treatment period, the patient is under dispensary observation by a phthisiatrician for two to five years, depending on the complexity of the disease. Statistics show that 81% of those who fall ill recover completely, 12% recover only partially, and the disease continues in 7%. Relapses occur.
Preventative methods for preventing sarcoidosis have not been identified, and the prognosis depends on early detection of the disease during clinical examinations.
Published in Diseases of the respiratory tract and lungs Premium Clinic
Treatment
This disease is interesting because the patient almost plays the lottery. The fact is that about 30% of cases of the disease resolve on their own and without any additional intervention. And one could say that there is no need to rush, you can wait until everything gets better on its own. But the problem is that the same 30% of patients face serious complications of sarcoidosis - even death, if help is not started on time. So in this case, you definitely shouldn’t refuse treatment or delay visiting a doctor. No one knows what percentage of patients it will fall into, and delaying time can be truly dangerous.

It is important to understand that when the disease progresses without complications, doctors often leave time for observation. They analyze the condition of patients and understand that in some cases it is necessary to wait and see how the disease develops. And only in a situation where it is clear that the body cannot cope on its own, treatment is prescribed.
Treatment of sarcoidosis includes steroid hormones, anti-inflammatory drugs, immunosuppressants, antioxidants, and vitamins. The patient is also prescribed a protein diet (when taking hormonal medications) and is recommended to reduce the amount of salt. An important point for recovery is the complete cessation of such a bad habit as smoking.
After the onset of remission, the patient remains registered for several years and is observed by his attending physician.
If you have already been diagnosed or suspect that you have pulmonary sarcoidosis, contact the Meditsina JSC clinic in Moscow: our pulmonologists and therapists are always happy to help, advise, prescribe additional examinations and adjust or develop a treatment plan for you.
Causes
The origin of the disease is not fully understood. Doctors are still arguing about what can cause this disease. One theory suggests that the disease is inherited, another suggests that it is caused by infection. Moreover, the pathogens can be fungi, protozoa and other variants of pathogenic flora - there is no consensus here either.
Instead of clear causes, experts identify factors that contribute to the development of the disease. For example, this is the effect of various irritants on lung tissue - the same strong chemicals in hazardous industries or abundant dust. Pathological processes inside the body, including autoimmune diseases, also contribute to the development of the disease.
Since it has not yet been possible to detect one cause of sarcoidosis, professionals agree that we are talking about a group of factors: biochemical, immune, genetic and others.
Smokers are at risk because their lungs are already weakened.
Lymph Node Biopsy Options
An open biopsy is the complete or partial removal of a lymph node through an incision. When choosing this biopsy option, the largest lymph node is examined. Unlike puncture examination, open biopsy of lymph nodes is carried out with the possibility of visual control, which makes it more informative and reliable.
Fine needle biopsy of lymph nodes is performed using different types of needles. A fine-needle biopsy involves inserting a needle with a diameter of less than 2 mm into the node and aspirating its contents into a syringe for subsequent examination. The progress of the procedure is controlled using ultrasound. Soft tissues are first infiltrated with an anesthetic.
A puncture biopsy involves taking biomaterial for histological examination of tissue. Puncture sampling of biomaterial is similar to a fine-needle biopsy and allows you to extract a column of living tissue. A contraindication for a puncture biopsy is a malignant process, since in this case there is a possible risk of malignant cells spreading from an isolated focus throughout the body through the lymphatic and circulatory systems. The disadvantage of the needle biopsy option is the risk of false readings (both positive and negative).
Symptoms of pulmonary sarcoidosis
The disease can occur without pronounced symptoms for a long time, up to large volumes of affected tissue.
Frequent symptoms are:
- increased fatigue,
- cough,
- slight increase in body temperature
- the appearance of red itchy spots on the skin of the legs (erythema nodosum)
Surprisingly, patients with sarcoidosis often come to the doctor not with the listed symptoms, but with complaints of discomfort in the eyes (conjunctivitis, dryness), skin lesions (brown, yellow plaques appear), based on these and other indirect signs, an experienced specialist will be able to diagnose sarcoidosis even in the early stages.
Diagnostics
The following examinations are used to diagnose sarcoidosis and identify organ damage.
General blood and urine tests, biochemical blood test, including the level of calcium, phosphorus, alkaline phosphatase activity, angiotensin-converting enzyme in the blood serum.
Computed tomography of the chest (CT CT): allows to detect enlarged intrathoracic lymph nodes, interstitial (reticulonodular) changes in the lung parenchyma, signs of pulmonary fibrosis.
Pulmonary function tests, diffusion capacity test (DLCO) - the most characteristic of sarcoidosis are restrictive ventilation disorders (decreased lung volumes), often in combination with a decrease in lung diffusion capacity.
Electrocardiography (ECG) is performed on all patients as a screening test; Holter ECG monitoring - according to indications.
Echocardiography (EchoCG) is performed to exclude pulmonary hypertension (PH), as one of the complications of pulmonary sarcoidosis, and to assess global and local myocardial contractility.
To morphologically verify the diagnosis and exclude infectious and oncological pathologies with a similar clinical and laboratory-instrumental picture, a biopsy of the lung, intrathoracic or peripheral lymph nodes, and skin is performed.