Sometimes we underestimate such an indicator of health as blood viscosity. Read more about the state of our blood, its structure and the reasons for thick blood...
The state of the blood is the state of the cardiovascular system. Unfortunately, cardiologists go past hematology, go through the blood vessels, through the heart, and all the time try to strengthen the heart muscle. Everyone strives to dilate blood vessels, but in reality another process occurs.
What is thick blood and what can you do about it?
When blood quality is impaired, primarily due to thickening, acidification, increased cholesterol, etc., the main transport function of the blood becomes difficult, which leads to disruption of redox processes in all organs and tissues, including the brain and liver , kidneys, etc. Blood quality must be maintained within optimal homeostasis.
Subscribe to our INSTAGRAM account!
A change in the normal consistency of the blood becomes a “trigger” that starts the process of development (or exacerbation of existing) diseases, such as atherosclerosis, varicose veins and others.
There is no separate disease called “thick blood”, so it would not be correct to clearly name the symptoms of “thick blood”. These same symptoms can also appear with other problems in the body.
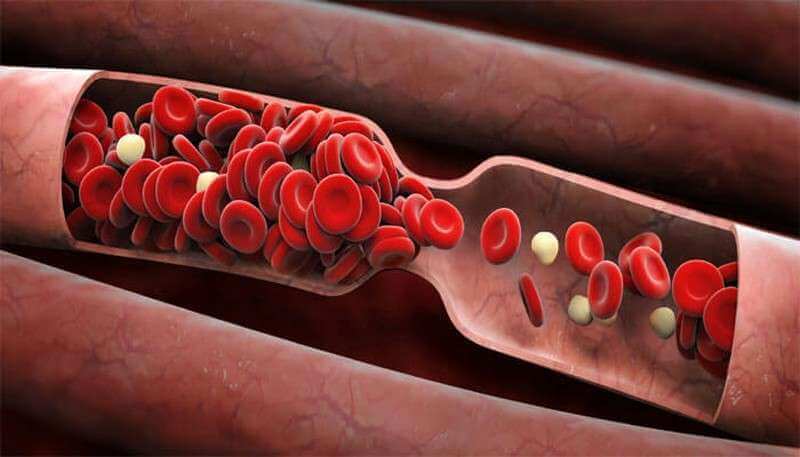
Thick blood has increased viscosity - this causes stagnation of blood in the vessels and increases the risk of blood clots.
Clinical manifestations of thick blood:
- high blood pressure; - drowsiness; — fatigue; - general weakness; - depressive states; - dry mouth; - headache; — absent-mindedness; - constantly cold extremities; - heaviness in the legs; - nodules on the veins.
This list can be continued, but the process sometimes occurs in a hidden form and is revealed only after donating blood for analysis.
A comprehensive blood test for clotting is called a coagulogram. This analysis gives an idea of the general state of hemostasis (shows a complete picture of blood coagulation, as well as the integrity of blood vessels).
Causes of thick blood
Why does blood thicken? There are a number of important factors that influence its consistency.
1. Lack of water. Blood is 85%, and blood plasma is 90-92% water. Therefore, a decrease in this indicator by just a few percent leads to blood thickening.
2. Intensive loss of water occurs not only in summer, but also in winter - dry indoor air “pulls water out of us like a sponge;
3. For athletes , playing sports is accompanied by burning energy, the body increases heat transfer to cool down;
4. For certain diseases, for example, diabetes.
5. Enzymopathy. A pathological condition in which there is insufficient activity of certain food enzymes or their complete absence. As a result, complete breakdown of food components does not occur and under-oxidized breakdown products enter the blood, which leads to its acidification.
6. Poor nutrition. Some food products (legumes, cereals, rice, eggs, etc.) contain heat-stable specific protein inhibitors that form stable complexes with proteinases of the gastrointestinal tract, causing disruption of the digestion and absorption of food protein. Completely digested amino acid residues enter the blood. Another reason lies in the excessive consumption of carbohydrates and sugar, including fructose.
7. Environmental contamination of products. Suppression of enzymatic activity is facilitated by contamination of food products with salts of heavy metals, pesticides, insecticides and mycotoxins, which interact with protein molecules, forming stable compounds.
8. Lack of vitamins and minerals. Water-soluble vitamins: C, group B and minerals are necessary for the biosynthesis of most enzymes, so their deficiency (vitamins) leads to incomplete digestion of food due to the lack of necessary enzymes.
9. Strong acids. Strong acids are the end product of the breakdown of animal proteins. If the kidneys cannot cope with removing acids, then they remain in the body and acidification of the blood occurs.
10. Damage to blood vessels. A healthy inner wall of blood vessels (intima), which consists of endothelium, has antithrombogenic properties.
11. Liver dysfunction. Every day, 15-20 grams of blood proteins are synthesized in the liver, which perform transport, regulatory and other functions; disruption of biosynthesis in the liver leads to changes in the chemical composition of the blood.
12. Hyperfunction of the spleen. Causes the destruction of blood cells.
13. Presence of parasites in the body.
Blood consists of two parts - formed elements and plasma. Plasma is the liquid part, and the formed elements are blood cells, which, in addition to their main functions, also make the blood thick. When there are more formed elements than plasma, the viscosity of the blood increases and it becomes thick. But, before we talk about how to thin the blood, it is worth examining in detail what thick blood is.
There is no such concept in medicine. There are viscous blood and an increased hematocrit number. Blood viscosity is determined by the amount of fibrinogen and the level of prothrombin, although blood viscosity can also increase due to an increase in other indicators, such as cholesterol, hemoglobin, glucose, and so on.
The hematocrit number is a general indicator of the ratio of plasma and formed substances, which ultimately also means increased viscosity or, conversely, fluidity of the blood.
Is blood clotting dangerous?
Undoubtedly. Blood is not just a fluid in the body that flows through the circulatory system and carries nutrients or waste products, it, together with the nervous system, connects our body into a single whole. Increased blood viscosity means that not all of its cells will be able to perform their function, which means that some tissues will not receive enough nutrients, and some breakdown products will not be excreted.
In addition, pushing through an excessively thick mass requires an extremely powerful motor, which will eventually wear out much faster. That is, you need a healthy, strong heart, the rapid wear and tear of which does not bode well. And this is not to mention the possible formation of blood clots with all the ensuing consequences.
In the presence of viscous blood, nosebleeds are very common. Because of which? And this happens because if the blood is viscous, then the body has little oxygen, and because of this, the cells begin to “starve”, accordingly, the pressure inside the cells begins to rise. If the blood supply to the arms and hands, legs and feet is impaired, reddish spots will appear on the arms and feet, which if you touch, you can feel how cold they are.
What affects blood viscosity
Blood viscosity is affected by vascular damage, distortion of liver function, which affects the chemical composition and increases the viscosity of plasma, negative changes in the condition of the membranes of red blood cells and platelets, leading to vigorous adhesion of these cells.
The viscosity of blood is also affected by the ratio of cell mass to the liquid part of the blood. Like all indicators of the body, this one should not be high, not low, but normal.
The danger of high blood viscosity is the increased risk of blood clots in the heart and blood vessels.
The cause of a blood clot is viscous blood
Due to problems with the thyroid gland, the stomach malfunctions: bile and pancreatic enzymes enter the duodenum late, when all the food has already moved to the intestines. At this time, the pressure in the empty stomach drops, and in the intestines into which the food has gone, it rises. Due to the difference in pressure, bile and pancreatic enzymes (this is a very powerful alkali in quality) enter the stomach, where hydrochloric acid is contained. As a result of the reaction between them, hydrochloric acid is neutralized, which is produced after eating only to dissolve the blood.
If this happens after each meal, then the concentration of chlorine in the blood is not restored and the blood increases its viscosity. This causes the formation of blood clots (thrombophlebitis - lack of chlorine in the blood). When thrombophlebitis appears, viscous blood begins to “glue” small vessels - capillaries, which are most abundant on the extremities: arms, legs, and head. Blood circulation is disrupted: hands become numb, cold, and sweaty.
The most serious is a violation of the microcirculation of the blood vessels of the head, since the head is a microprocessor responsible for all other organs and unconditioned reflexes. As a result, memory deteriorates, fatigue increases, drowsiness and lethargy appear.
Not only the brain itself suffers, but also the eyes. The eye muscle is constantly in motion and must receive oxygen in a large volume, which is impossible when small vessels are glued together, so it spasms, resulting in myopia, farsightedness or astigmatism. Over time, when large vessels begin to “seal”, a stroke or heart attack occurs.
Let's take a closer look at what human blood is and its functions, what thick blood is and the reasons that contribute to increased blood viscosity.
Human blood is an opaque, red liquid consisting of:
— Pale yellow blood plasma; — Formed elements suspended in it: erythrocytes (red blood cells), leukocytes (white blood cells), platelets (blood platelets)
Blood viscosity test: blood plasma proteins prothrombin and fibrinogen are not critical.
Blood viscosity is a very important blood indicator that determines the maximum service life of the heart and blood vessels. The higher the viscosity of the blood, the faster the heart wears out. And by increasing blood pressure, the heart tests the strength of blood vessels and their resistance to heart attack and stroke.
It is traditionally believed that blood viscosity is determined only by the blood plasma proteins prothrombin and fibrinogen. Those. to assess blood viscosity, they are guided by the level of prothrombin, which should be at the lower limit of the normal range of 70-100%, and the amount of fibrinogen within the range of 2-4 g/l.
However, an equally important indicator is the erythrocyte sedimentation reaction (ERS), or as it was previously called the erythrocyte sedimentation rate (ESR). Those. the ability of blood cells to settle, forming plasma above the blood column. The reaction is assessed within 1 hour. The lower the ESR (ROE), the higher the blood viscosity. And many rejoice when they receive ROE (ESR) of 1-3 mm per hour!
And at the same time, the viscosity of the blood is very high and the heart is forced to pump viscous blood with significant overload!
When a traditional blood viscosity test is performed, they usually only analyze the level of prothrombin and the amount of fibrinogen in the blood - i.e. rely on only part of the blood components, which determine the rheological properties or fluidity of the blood plasma, and not the blood as a whole! ROE (ESR) is also occasionally taken into account.
Prothrombin and fibrinogen are the most abundant proteins in blood plasma. And blood plasma represents approximately 50% of blood volume. And by assessing only these two components, only part of the factors determining blood viscosity is revealed.
The amount of albumin proteins also affects blood viscosity. Although albumins do not take part in the work of the blood coagulation system, they play an important role - they bind various toxins and promote their transfer to the main excretory organs - the liver and kidneys. Those. promote self-cleansing of the body, cleansing the blood of various toxins. The amount of albumin in the blood affects not only blood viscosity, but also the tendency to allergic diseases and the activity of nonspecific immunity.

Effect on blood viscosity of other components of blood plasma
Blood plasma also contains other substances that promote the adhesion (agglutination) of red blood cells and determine blood viscosity. These include cholesterol, glucose, and protein digestion products. The level of cholesterol, the content of which in the blood serum depends on the condition of the liver. As well as the ability of the pancreas to control blood sugar levels by moving glucose into cells for metabolism. And also the ability of the liver to process the products of protein digestion and transform them into protein molecules that are unique to you.
The remaining 50% of the blood is occupied by blood cells themselves - red blood cells (approximately 99% of the volume of all blood cells), as well as platelets and leukocytes.
The cellular composition of the blood also affects the rheological (fluidity) properties of the blood. In assessing blood viscosity, both the number of red blood cells (increases in professional athletes, with regular fitness classes, in the gym, in pathologies of the respiratory system, heart and circulatory system) and the degree of red blood cell agglutination and platelet aggregation are important. Those. the ability of the most numerous blood cells to stick together.
Environmental influence on blood viscosity
In recent years, the human ecological environment has changed significantly, and the amount of natural food products has decreased. This significantly affected the balance of the body’s antioxidant system and the amount of free radicals that are formed in the body of modern humans. Blood, occupying a strategically important position in the body, connects a system of barrier organs through which various xenobiotics from the environment enter, along with inhaled air, food and drinks. And the work area (the cell itself), where during any work the formation of waste products (“waste”) and the production of free radicals occur.
What contributes to the formation of pathology
The quality of plasma depends on many factors - nutrition, functioning of internal organs, daily routine. Stress and addictions almost always cause the development of hyperviscosity syndrome. Let's take a closer look at the causes and treatment of thick blood. What causes blood to thicken - errors in nutrition:
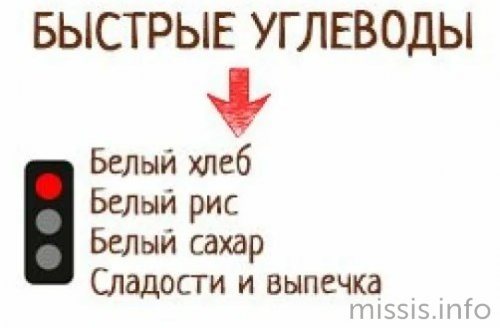
- Passion for fast carbohydrates and protein foods. Sweets increase the amount of glucose, and protein foods contain many amino acids that enter the blood undigested - all these factors contribute to the development of hyperviscosity syndrome.
- Increased cholesterol levels with regular consumption of alcohol, fast food, fatty and other junk foods.
- Poisoning of the body with heavy metals and pesticides that accumulate in vegetables and fruits when treated with potent chemicals.
- Avitaminosis - an increase in thickness is observed when there is a lack of ascorbic acid and B vitamins in the body.

- The main reason for increased viscosity is dehydration, non-compliance with the water regime, and the use of low-quality tap water.
But thick blood is always a sign of poor nutrition or lifestyle; often the pathological condition develops against the background of serious illnesses. The main reason is vascular diseases, varicose veins, chronic heart failure.
Why does blood viscosity change?
Being at the intersection of two powerful flows of toxins (ecology on the one hand and work intensity on the other), the state of the blood reflects the contribution of each component to the rheological properties of the blood. Or rather, the individual characteristics of the human body, the ability to withstand the environment around it.
If your body’s antioxidant potential (the ability to produce and accumulate antioxidants) is high, the blood will be more fluid and such a person is prone to longevity. And the most numerous blood cells in this case, when analyzing a living drop of blood, are located separately.
If the body's antioxidant potential is low, the most numerous blood cells, erythrocytes, agglutinate among themselves, forming bizarre structures resembling coin columns or tiles. Blood viscosity increases and many risks increase.
Increase or decrease in the number of red blood cells in tests. ESR
Red blood cells and their significance in tests: decrease and increase in the number of red blood cells in a general blood test and in urine analysis. Erythrocyte sedimentation rate (ESR) and its meaning.
Erythrocytes (red blood cells, rbc) are the most numerous blood cells that perform the function of transporting oxygen and nutrients to tissues and organs. Red blood cells contain large amounts of the red pigment hemoglobin, which is able to bind oxygen in the lungs and release it in the body tissues.
- A decrease in the number of red blood cells in the blood is a sign of anemia.
- An increase in the number of red blood cells in the blood can be observed with severe dehydration, as well as with erythremia.
- The appearance of red blood cells in the urine can occur with inflammation of the urinary system (kidneys, bladder).
What are red blood cells?
Erythrocytes, or red blood cells, are the most numerous blood cells. Red blood cells have a regular disc-shaped shape. At the edges of the red blood cell, it is slightly thicker than in the center, and on a section it looks like a biconcave lens, or dumbbell. This structure of the red blood cell helps it to be maximally saturated with oxygen and carbon dioxide when passing through the human bloodstream.
The formation of red blood cells occurs in the red bone marrow, under the influence of a special kidney hormone - erythropoietin. Mature red blood cells circulating in the blood do not contain a nucleus or organelles, and cannot synthesize hemoglobin and nucleic acids.
Red blood cells are characterized by a low level of metabolism, which determines their long lifespan, on average 120 days. Over the course of 120 days from the moment red blood cells leave the red bone marrow and enter the bloodstream, they gradually wear out. At the end of this period, “old” red blood cells are deposited and destroyed in the spleen and liver.
The process of formation of new red blood cells in the red bone marrow is ongoing, therefore, despite the destruction of old red blood cells, the total number of red blood cells in the blood remains constant.
Red blood cells consist mainly (2/3) of hemoglobin - a special protein containing iron, the main function of which is the transport of oxygen and carbon dioxide. Hemoglobin is red, which determines the characteristic color of red blood cells and blood.
The main functions of red blood cells are the transfer of oxygen from the lungs to the tissues of the body and carbon dioxide from the tissues to the lungs; they also perform nutritional and protective functions and maintain the acid-base balance in the blood.

Red blood cells
The total number of red blood cells in human blood is enormous. For example, in the blood of a person weighing 60 kg, the total number of red blood cells is 25 trillion. If such a number of red blood cells are stacked one on top of the other, you will get a column more than 60 km high!
However, it is much more convenient and practical to determine not the total number of red blood cells in the human body, but their content in a small volume of blood (for example, 1 cubic millimeter, µl). The content of red blood cells in 1 cubic mm (µl) is an important indicator that is used in determining the general condition of the patient and in the diagnosis of many diseases.
In healthy people, the normal total content of red blood cells in one volume unit of blood (norm) fluctuates within rather narrow limits. We also add that the norms for the content of red blood cells depend on the person’s age, gender, and place of residence.
Normal level of red blood cells in the blood
Determination of the number of red blood cells is carried out using a general (clinical) blood test.
Normally, the number of red blood cells in the blood of men is from 4 to 5.1 million per 1 μl (from 4 to 5.1 × 10¹² in 1 liter), in women - from 3.7 to 4.7 million per μl (from 3.7 to 4.7 × 10¹² in 1 l).
The number of red blood cells in a child depends on age:
- On the first day of life, in a newborn child - from 4.3 to 7.6 × 10¹²/l
- At 1 month from 3.8 to 5.6×10¹²/l
- At 6 months – from 3.5 to 4.8×10¹² /l
- At 12 months from 3.6 to 4.9 × 10¹² / l,
- From 1 year to 12 years from 3.5 to 4.7×10¹² /l
- The content of erythrocytes in the blood of children over 13 years of age corresponds to that of adults and ranges from 3.6 to 5.1 × 10¹² / l.
The high content of red blood cells in the blood of newborns is explained by the fact that during intrauterine development the child’s body needs more red blood cells to ensure a normal supply of oxygen to tissues in conditions of relatively low oxygen concentrations in the mother’s blood. Immediately after birth, the newborn baby's red blood cells begin to break down and are replaced by new red blood cells. Increased breakdown of red blood cells in the first days after birth is the cause of the development of jaundice in newborns.
Red blood cell levels during pregnancy
The number of red blood cells during pregnancy can decrease to 3.5 and even 3.0 x10¹² / l, and many researchers consider this to be the norm.
The decrease in the number of red blood cells in the blood during pregnancy (compared to the levels of red blood cells in the blood of non-pregnant women) is explained, on the one hand, by dilution of the blood due to water retention in the body of a pregnant woman, and on the other hand, by a slight decrease in the formation of red blood cells due to iron deficiency, which occurs in almost all pregnant women.
Changes in the content of red blood cells in the blood and their interpretation
The content of red blood cells in the blood can change in two directions: a decrease and an increase in the content of red blood cells in the blood relative to the norm.
What does an increase in the number of red blood cells in the blood mean?
An increase in the number of red blood cells per unit volume of blood is called erythrocytosis. In general, an increase in the content of red blood cells in the blood is observed quite rarely.
A physiological increase in red blood cells occurs in people living in the mountains, during prolonged physical activity in athletes, under stress, or with significant dehydration.
A pathological increase in the number of red blood cells in the blood occurs when:
- Increased production of red blood cells in the red bone marrow (in blood diseases such as erythremia); In patients with erythremia, a bright red discoloration of the skin of the face and neck can usually be seen.
- As a result of increased synthesis of erythropoietin in the kidneys with insufficient oxygen in the blood in diseases of the respiratory and cardiovascular systems (for example, in patients with heart failure or COPD). In such cases, an increase in the number of red blood cells in the blood is preceded by a long history of heart or lung disease.

Decreased number of red blood cells in the blood
A decrease in the number of red blood cells per unit volume of blood is called erythropenia.
The main reason for the decrease in the number of red blood cells in the blood is various types of anemia (anemia), which can develop as a result of impaired formation of red blood cells in the red bone marrow, as a result of their increased destruction of red blood cells, for example, with hemolytic anemia, as well as with blood loss.
Subscribe to our Yandex Zen channel!
Most often, iron deficiency anemia is observed, in which insufficient formation of red blood cells occurs due to iron deficiency due to its insufficient intake from food (vegetarian diet), malabsorption, or an increase in the body's need for iron (often during pregnancy, in children during periods of intensive growth) .
Against the background of iron deficiency anemia, not only a decrease in the number of red blood cells in the blood is observed, but other symptoms of this disease may also be noticed.
Less commonly, a decrease in the number of red blood cells in the blood occurs with a lack of vitamin B12 or folic acid. In such cases, in addition to anemia, patients experience disturbances in gait and sensitivity (tingling and pain in the arms and legs).
Increased destruction of erythrocytes, or hemolysis, as the cause of a decrease in the number of erythrocytes in the blood, occurs in hereditary diseases as a result of a violation of the structure of the erythrocyte membrane (microspherocytosis, ovalocytosis), hemoglobinopathies (thalassemia, sickle cell anemia); acquired causes of hemolysis - Marchiafava-Micheli disease, mechanical damage to the erythrocyte membrane (artificial heart valve, gigantic spleen in patients with cirrhosis), toxic damage to the erythrocyte membrane (poisonous mushrooms, snake bites, heavy metal salts).
A decrease in the number of red blood cells also occurs during acute massive blood loss (as a result of bleeding during injuries, operations, stomach ulcers), chronic blood loss leads to iron deficiency anemia.
The number of red blood cells in the blood is determined during a general (clinical) blood test.
Nutrition for high blood viscosity
Blood thinning is facilitated by diet and a special drinking regimen. You should drink at least 1.5 liters of fluid per day. The healthiest options are green tea or herbal teas (as recommended by your doctor), natural vegetable and fruit juices, and water. It is especially recommended to drink natural red grape juice. Due to its high content of bioflavonoids, it is considered a balm for the cardiovascular system.
An additional source of omega-3 unsaturated fatty acids is flaxseed oil , which can be taken 1 tbsp. spoon a day. Prostaglandins synthesized from these acids reduce cholesterol levels and thin the blood.
Another important source of fat is unrefined, cold-pressed olive oil , which contains a large amount of biologically active substances.
To thin the blood, products containing the amino acid taurine are recommended. When cooked, the amount of taurine in food decreases sharply.
Treatment of "blood thickening"
Treatment of pathology in non-pregnant women begins with finding the cause of “blood thickening” and eliminating it. As a preventative measure, women who have entered menopause are recommended to take low-dose aspirin daily in the absence of contraindications.
Self-medication is unacceptable! Take any medications after consulting a doctor.
In patients with chronic causes of “blood thickening,” metabolic disorders are corrected. In an acute disease accompanied by the appearance of “thick blood”, it is often enough to cope with the main pathogenetic mechanism.
Treatment of “blood thickening” is symptomatic
. When hypercoagulation is detected based on the examination results, drugs with antiplatelet (Aspirin, Curantil and others) and anticoagulant (Heparin, Fraxiparin, Phenilin and others) activity are used. These drugs are prescribed to prevent thrombosis.

If hypocoagulation and a tendency to bleeding are detected in patients, hemorrhagic syndrome is prevented. For this purpose, transfusions of platelet components and donor plasma are used, plasmapheresis and hemosorption are performed. An equally important aspect is the correction of drinking regime and nutrition. Patients are advised to exclude:
- White bread;
- sugar, carbonated drinks;
- fatty, spicy and salty foods;
- canned foods.
In the absence of contraindications, it is necessary to expand the drinking regime: at least 2 liters of clean water per day.

The diet should include:
- sprouted wheat, artichokes;
- ginger, cinnamon or celery;
- lemon and cranberry;
- seafood;
- linseed oil;
- nuts - 30 g/day or sunflower seeds;
- cocoa or dark chocolate.

Possible use of herbal preparations:
- red clover;
- yellow clover;
- meadowsweet;
- fireweed angustifolia;
- red hawthorn;
- horse chestnut;
- ginkgo biloba extract.