Spontaneous pneumothorax - symptoms and treatment
Treatment of spontaneous pneumothorax has four goals:
- removing air from the pleural cavity;
- cessation of air flow into the pleural cavity;
- complete expansion of the lung with restoration of its vital functions;
- prevention of recurrent pneumothorax [15][48].
In case of secondary pneumothorax, it is necessary to treat the underlying disease by a pulmonologist, rheumatologist, parasitologist or infectious disease specialist. Spontaneous pneumothorax manifests itself as a complication, so the role of the thoracic surgeon here is more of an auxiliary nature.
Conservative treatment
Conservative treatment is acceptable if two conditions are met:
- If the patient has a small pneumothorax, that is, the distance from the lung to the chest wall is no more than 2 cm at the level of the root of the lung and no more than 3 cm at the level of its apex according to radiography in a standing position in the frontal projection (en face), lung collapse is up to 15%.
- If there are no signs of respiratory failure: shortness of breath, tachycardia, decreased blood oxygen saturation [14].
If there is pain, analgesics are prescribed. Oxygen therapy helps: if on average air from the pleural cavity is absorbed by the pleura at a rate of 2% per day, then when inhaled with an oxygen mixture this process accelerates 4 times.
As a rule, antibiotics are prescribed to prevent infection and the development of pleural empyema, but there is no absolute evidence of the need for antibiotic prophylaxis and in each case the issue is resolved individually [24].
Pleural puncture
In order to more quickly expand the lung, a single puncture of the pleural cavity (puncture of the chest wall to remove air) is acceptable, followed by dynamic observation and conservative treatment [31]. Such tactics may be justified in case of pneumothorax, which occurred for the first time in practically healthy people under 50 years of age. Lung collapse is no more than 15-30% and there are no significant breathing disorders. That is, this is no longer a minor pneumothorax, but the vital functions of the body are still compensated.
It is believed that the safest point to puncture the chest wall for pneumothorax is the space between the second and third ribs at the level of the middle of the collarbone. However, from a surgical and anatomical point of view, safer points for pleural puncture are the spaces between the third and fourth or fourth and fifth ribs along a line in the middle of the armpit. There, the gaps are quite wide, the chest wall is thinnest and there are no large vessels. In addition, in this place the distance from the lung to the chest wall in the presence of pneumothorax is maximum. In any case, before puncture, X-ray images are analyzed and the optimal location for puncture is selected [48].
Pleural puncture is performed under local anesthesia; there is no significant pain during the procedure. Patients usually tolerate this procedure well.
Drainage of the pleural cavity
Currently, there are special systems that combine a small needle into which a soft catheter is inserted. Thanks to this, when the chest wall is punctured, a catheter is immediately installed. After this, the needle is removed and you can safely, without the risk of injuring the lung with the needle, pump out the air from the pleural cavity.
If there is no such system, then when pumping out air using a needle, there is a risk of damaging the lung, as it will straighten out and move closer to the chest wall and, accordingly, to the needle. In addition, after a routine puncture, it is possible to understand whether there is a recurrence of pneumothorax only by performing a control radiograph or by the deterioration of the patient’s condition. Other examination methods are of an auxiliary nature, since after puncture, residual air in the pleural cavity still remains and signs of pneumothorax can be detected. It is also known that with repeated punctures success can be achieved only in one third of cases. Therefore, it is recommended to drain the pleural cavity using a catheter.
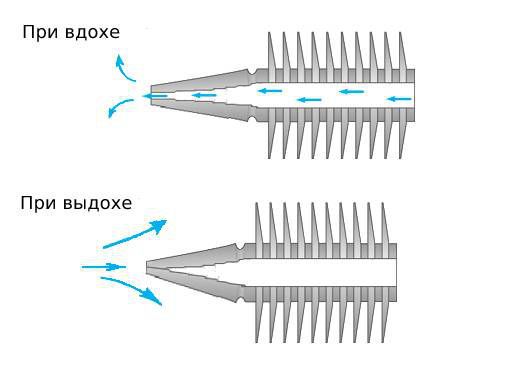
As already described above, through a special needle, which serves as a guide stylet, a catheter with a diameter of less than 3 mm is installed into the pleural cavity and fixed to the skin. A tube is attached to the catheter, which is connected to a jar of water. The end of the tube is lowered under water. Another tube comes out of the jar, which makes the jar leaky, that is, it communicates the cavity of the jar with the environment. This creates a water valve that releases air from the pleural cavity and prevents it from being sucked back in. To speed up the process, the can is connected to an active aspirator-suction, which pumps out air and creates negative pressure in the pleural cavity, due to which the lung expands.
When air bubbles stop appearing in the jar, it means the defect in the pleura has closed and air no longer flows in. That is, the doctor can directly control the treatment process, which cannot be done with a conventional puncture [40].
If within 72 hours, with a control radiograph, the lung is completely expanded, there are no signs of pneumothorax, and there is no air blowing in the jar for 24 hours, then treatment at this stage can be considered complete. The drainage is removed. A day later, a control X-ray of the chest organs is performed. If there is no recurrence of pneumothorax, the patient is discharged [48].
If, after three days, air enters, then surgical treatment is indicated.
Surgery
In rare cases, if the patient is weakened, has many severe concomitant diseases, and the lungs themselves are greatly altered (for example, with chronic obstructive pulmonary disease), the issue of using minimally invasive care is decided - installing a bronchial blocker.
A bronchial blocker is a valve that is inserted into the bronchus during bronchoscopy. The operation is performed under local anesthesia and is well tolerated by patients. The valve allows air to escape from the pleural cavity back through the upper respiratory tract to the outside and prevents its penetration inside [48].
The disadvantage of this treatment is that the valve can only be installed for 10-14 days, sometimes it moves, and it is not always possible to find the bronchus from which the air is leaking.
Radical treatment of spontaneous pneumothorax is considered to be atypical lung resection and subtotal pleurectomy.
An atypical resection is the cutting off of a small portion of the lung. Typically this is the apex of the lung because it often contains bullae. Resection is carried out with special staplers with titanium clips, which carefully and hermetically cut off the pathological area bloodlessly and without air leakage. This procedure further helps to fix the lung to the chest wall, which prevents displacement of the lung in case of a possible relapse. But, as already noted, the cause of spontaneous pneumothorax is most often damage to the entire lung, so removal of only one area cannot prevent the occurrence of a new pleural rupture in another place. The solution may be an operation - pleurodesis , as a result of which fusion occurs between the layers of the pleura due to which the lung is fixed to the chest [37][48].
Pleurodesis can be mechanical or chemical. With mechanical pleurodesis, the pleura is coagulated with an electrocoagulator, which creates burns on the pleura. It is also possible to scratch it with an abrasive material [7].
In chemical pleurodesis, the pleura is fixed to the chest wall by spraying sclerosing agents such as talc, doxycycline, bleomycin, etc. into the pleural cavity. These substances are often used abroad [53].
Increasing clinical evidence shows that chemical pleurodesis is a simple and safe treatment for spontaneous pneumothorax. Talc sometimes causes systemic inflammation and respiratory failure, but such side effects are usually associated with high doses of sclerosant and small particle size.
When treating patients who suffer from interstitial pneumonia and are taking corticosteroids, talc should be used with caution to avoid complications [54].
As already noted, the optimal and internationally recognized method of surgical pleurodesis is subtotal pleurectomy [13]. The operation consists of removing that part of the pleura that is located on the ribs. At this point, the lung is subsequently fixed to the chest wall. Even if a new rupture of the pleura occurs in some area not fixed to the chest wall, the lung is sufficiently fixed to prevent its collapse.
Three main methods for performing atypical lung resection and pleurectomy:
- Thoracotomy - through a large incision in the chest wall. Such operations have been performed before, after which there were the fewest relapses, but they were accompanied by significant trauma and pain.
- Through three thoracoports, which are installed in incisions of 5-15 mm. The technique appeared with the development of endosurgical technologies. A video camera is inserted into the pleural cavity, and all manipulations on the pleura and lung are performed using special instruments.
- Through a single incision no larger than 3 cm. Recently, this method of surgical intervention has been gaining popularity. Its advantage is that only one area in one intercostal space is injured, so pain after surgery is not as pronounced and the risk of chronic pain is less compared to a technique that uses three ports [4].
Treatment of catamenial (menstrual) pneumothorax
A special category consists of patients with catamenial pneumothorax . They must be treated by a gynecologist. It is believed that radical treatment of catamenial pneumothorax is possible only with suppression of menstrual function. If a woman does not plan a pregnancy in the future, then the issue of tubal ligation is decided.
If there are defects in the diaphragm, there are several methods of surgical intervention.
- If there are few defects and they are of relatively small diameter, then suturing them is possible.
- For widespread lesions, the area with defects is excised with a linear stapler, as is done in atypical lung resection [33].
- Another option for eliminating diaphragm defects is to cover them with a special “patch”, which can consist of synthetic and natural materials [17][48].
There are no large studies confirming the advantage of one or another treatment method for catamenial pneumothorax, so the decision in each specific case is made individually [25].
All operations are performed under general anesthesia using separate intubation, which allows you to turn off the lung on the side where the intervention is performed.
Upon completion of the operation, one or two drains are installed in the pleural cavity, which are connected to an active suction system. Depending on the situation, drains are left in place for up to 5-7 days, which ensures complete expansion of the lung, evacuation of fluid that arises in response to surgical trauma, as well as reliable fixation of the lung to the chest wall [46].
If the control radiograph shows no signs of pneumothorax and fluid in the pleural cavity, the drains are removed and the patient is discharged home.
Postoperative period
The sutures are removed 5 days after the last drainage is removed. It is necessary to limit physical activity for at least a month after surgery. A special protective regime is recommended for the same period. You can't get too cold and catch a cold.
After three months, it is recommended to conduct a control CT scan of the chest, followed by consultation with a thoracic surgeon and determination of further treatment tactics.
Possible postoperative complications
As a rule, the operation proceeds without early and late complications. In isolated cases, subcutaneous emphysema in the area of surgical approaches, which does not require additional treatment, since emphysema goes away on its own [37][48].
Using modern technologies, surgical approaches have minimal dimensions. Patients with bleeding disorders sometimes experience hematomas , which, as a rule, resolve on their own and do not require surgical intervention.
Suppuration from surgical wounds also occurs rarely, usually in weakened patients with immunodeficiency and diabetes. This is a special category of patients that requires a different approach to treatment.
In patients who have suffered many recurrences of pneumothorax and have pronounced adhesions and scar changes in the pleura, increased bleeding during surgery . After surgery, sometimes the amount of wound discharge is greater than in patients with a short history of the disease. To prevent the accumulation of wound discharge and the formation of blood clots in the pleural cavity, these patients undergo long-term (up to a week) active aspiration, which ensures sanitation of the pleural cavity and reliable fixation of the lung to the chest wall.
As a rule, infectious complications from the pleural cavity do not occur with primary spontaneous pneumothorax. Exceptions include patients with diabetes mellitus and severe immunodeficiency.
Complications associated with pleural puncture are the same as those associated with radical surgery. Suppuration and empyema of the pleura occur in 1-3% of cases, lung injury - in 0.2-0.6%, injury to the diaphragm - in 0.4% [37].
Diagnostics
Photo: twitter.com
Pathology is determined based on external examination data and the results of imaging techniques.
- Physical examination . The patient takes a forced position to facilitate breathing. The skin is moist, cool, pale or cyanotic. Excursions of the chest on the affected side are limited, the intercostal spaces are widened. Dyspnea, tachypnea, and tachycardia are observed.
- Radiography . The best conditions for confirming pneumothorax are created when the patient is in an upright position and using a direct projection. The images visualize an area of clearing without a pulmonary pattern, a displacement of the mediastinum, and a low dome of the diaphragm.
- CT scan . A more sensitive and informative test used when radiographic findings are ambiguous. Detects small limited pneumothorax, allows you to differentiate between gas in the pleural cavity and large air cysts in emphysema, and is carried out to clarify the cause of spontaneous pneumothorax.
Laboratory tests for diagnosis are not informative. Determination of the blood gas composition and acid-base balance is carried out to assess the severity of the patient’s condition, to determine the need and scope of resuscitation measures in the presence of extensive lesions and chronic background lung diseases.
Folk remedies
Pneumothorax is a serious pathological condition that poses a danger to the life and health of the patient. Attempts at self-treatment using folk remedies and pharmaceutical drugs can lead to the death of the patient or the development of serious complications. If you suspect the development of this disease, you should immediately call an ambulance or take the victim to a specialized medical facility.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.