Thoracic aortic aneurysm
A thoracic aortic aneurysm is a weakening of the vessel wall, its expansion and protrusion. The aorta is the main blood vessel that supplies the body with blood, extends from the heart and is located in the middle of the chest and abdominal cavity. A large amount of blood flows through the thoracic aorta under high pressure, and therefore any damage (rupture) to this vessel can cause life-threatening bleeding. Aneurysm of the thoracic aorta is most often asymptomatic and is often discovered by chance during routine examinations for other diseases.
Most small, slow-growing thoracic aortic aneurysms do not rupture, but large, fast-growing aneurysms are at great risk of rupturing. The size and growth rate of the thoracic aortic aneurysm determines the treatment tactics, which range from watchful waiting to urgent surgery. Once a diagnosis of thoracic aortic aneurysm is made, patients should be monitored until symptoms develop or the aneurysm becomes significantly larger. This will allow the necessary planned surgical treatment to be carried out in a timely manner. Since emergency surgical intervention for rupture of the thoracic aorta is associated with a high risk of death.
Causes
The exact causes of the formation of a thoracic aortic aneurysm are currently unknown, but factors that may contribute to the formation and development of an aneurysm include:
- Marfan syndrome.
People who were born with Marfan syndrome, a genetic disorder that affects the connective tissue in the body, are at high risk of developing a thoracic aortic aneurysm. Marfan syndrome causes weakness of the aortic stack, which in turn leads to the formation of an aneurysm. People with Marfa cider often have certain physical characteristics, such as being tall, long arms, breast bone deformities, and vision problems. Other connective tissue diseases. In addition to Marfan syndrome, there are other connective tissue diseases, such as Ehlers-Danlos syndrome, which can also contribute to the development of aortic aneurysm. This disease usually affects the skin, joints and connective tissue. The skin becomes fragile, easily damaged, and very elastic. - Problems with your heart valves.
Those patients who have problems with the aortic valve have an increased risk of developing a thoracic aortic aneurysm. This is especially true for people who have a bicuspid aortic valve, meaning their valve has two leaflets instead of three. - Previous injuries to the aorta.
An aortic aneurysm is more likely to occur in people who have previously had problems with the aorta, such as a tear in the aortic wall (aortic dissection). - Injury.
People injured in car accidents are at high risk of developing a thoracic aortic aneurysm.
Thoracic aortic dissection
An aortic aneurysm should not be confused with an aortic dissection. Aortic dissection most often occurs in the location where the aneurysm was previously located. Delamination begins with a tear in the wall. This causes bleeding along the aortic wall, creating a false lumen. And in some cases there is a complete rupture. Aortic dissection is a life-threatening situation.
Aortic sclerosis: etiology and pathogenesis
The development of pathology can be triggered by the following factors:
- unhealthy diet;
- chronic infectious diseases - tuberculosis, syphilis, etc.;
- endocrine diseases - diabetes, obesity;
- stress and high levels of adrenaline in the blood;
- hypertension;
- autoimmune diseases;
- smoking and alcohol abuse;
- gout;
- sedentary lifestyle - physical inactivity;
- lack of physical activity;
- hereditary predisposition.
Alleviation of the patient's condition is achieved by eliminating provoking factors or reducing their impact.
The pathogenesis of aortic sclerosis consists of two main mechanisms: vascular-platelet and dyslipidemic. In the place where platelets accumulate (on a damaged vessel wall), microthrombi form. Due to lipid metabolism disorders, hypercholesterolemia develops. On the vascular walls there is an accumulation of fats, held together by connective tissue fibers, thus the formation of atherosclerotic plaques occurs, as they grow, the lumen of the vessels is deformed and narrowed. Sclerosis of the aorta of the heart leads to disruption of its blood supply and the development of dysfunction.
Symptoms
Thoracic aortic aneurysms grow slowly and are usually asymptomatic, making them difficult to identify. Some aneurysms will never rupture. Most small aneurysms do not progress or increase slowly in size, less than 1.2 centimeters per year. It is important to note that some aneurysms show a steady increase in diameter, which increases the risk of rupture. It is difficult to predict how quickly an aortic aneurysm will increase in diameter.
Some patients with an aortic aneurysm experience:
- soreness or pain in the abdomen or chest;
- backache;
Any part of the aorta that extends from the heart and runs in the abdomen can undergo aneurysmal change. If this occurs in the upper part of the aorta, it is called a thoracic aortic aneurysm. Most often, an aneurysm forms in the lower part of the aorta and is called an abdominal aortic aneurysm. Rarely, aneurysmal change can affect both the thoracic and abdominal aortas; this type of aneurysm is called thoracoabdominal.
You should see your doctor if you have symptoms of a thoracic aortic aneurysm.
If someone in your family has been diagnosed with an aortic aneurysm, Marfan syndrome, other connective tissue diseases, or a bicuspid aortic valve. Your doctor may recommend an ultrasound to detect an aortic aneurysm.
What symptoms indicate aortic sclerosis?
The clinical picture directly depends on the cause and location of the lesion, the degree of compression of adjacent internal organs by the dilated aorta or aneurysm. For example, with infectious aortitis, an increase in body temperature and a deterioration in general health are often observed. If inflammation of the aorta develops against the background of rheumatological diseases or systemic vasculitis, then, in addition to fever, the patient will begin to lose weight and complain of pain in the muscles and joints.
Since sclerosis of the vessel wall causes an increase in blood pressure, many patients experience symptoms of hypertension - headache, heaviness in the back of the head, dizziness. But most often, thickening of the aorta is asymptomatic until serious complications (stroke, heart attack, ruptured aneurysm).
Root compaction
Since the coronary arteries depart from the aortic root, changes in its functional properties affect the blood supply to the myocardium. Lack of oxygen is manifested by attacks of angina - pressing, burning or squeezing pain behind the sternum, radiating to the left arm, neck, and lower jaw. Compaction of the aortic root is often accompanied by aortic valve defects, so symptoms such as dizziness, lightheadedness, and loss of consciousness may appear.
When the process is started, signs of chronic heart failure (CHF) appear - swelling in the legs, shortness of breath, heaviness in the right side. Sometimes I am able to see such specific symptoms of aortic heart defects as visible pulsation of the carotid arteries in the neck or shaking of the head back and forth in time with the pulse.
Atherosclerosis of the ascending limb and arch
Atherosclerotic lesion of the ascending vessel is clinically very similar to root compaction. The carotid arteries, which supply blood to the brain, depart from the aortic arch, so when this section is damaged, patients experience signs of deterioration in cerebral circulation - headache, tinnitus, sleep disturbances, rapid mood swings.
Atherosclerosis of these areas is very dangerous, as there is a high probability of stroke. A blood clot that forms in the area of the aortic arch can break off and clog the cerebral arteries. Patients experience a feeling of strong pulsation in the upper chest. The enlarged and thickened aortic arch puts pressure on neighboring organs. For example, when the recurrent laryngeal nerve (the nerve of the vocal cords) is compressed, the voice becomes hoarse. When the trachea is compressed, a feeling of lack of air, dry cough, and attacks of suffocation occur.
Descending division lesion
The descending section has 2 parts: thoracic and abdominal. With sclerosis, the first to appear is burning pain in the chest, radiating to the back and upper abdomen. Compression of the esophagus causes difficulty swallowing. You can read about the symptoms of atherosclerosis of the abdominal aorta here.
Risk factors
- Age.
Thoracic aortic aneurysm most often occurs in people over 60 years of age. - Tobacco smoking.
Smoking is one of the main risk factors for the formation of thoracic aortic aneurysm. With increasing smoking experience, the risk of aneurysm formation increases. - Arterial hypertension.
High blood pressure damages the blood vessels in the body and thereby increases the risk of developing an aortic aneurysm. - Atherosclerosis.
Increased levels of cholesterol and other substances that can damage the lining of blood vessels also increase the risk of aneurysms. - Floor.
Aortic aneurysms occur more often in men than in women. However, women with an aortic aneurysm have a higher risk of rupture than men. - Race.
Aortic aneurysm occurs more often in white people than in people of other races. - Family history.
If someone in the family has had cases of aortic aneurysm, then his blood relatives have an increased risk of developing an aneurysm. These people tend to form aneurysms at a younger age and have a higher risk of rupture.
Why can the aorta become sclerotic?
Sclerosis or hardening of the aorta can develop for many reasons, which include:
- Atherosclerotic lesion. This is the most common cause of aortic hardening, especially in older people.
- Heart defects. In case of aortic valve defects of rheumatic or degenerative origin, the aorta, in particular its root, is also involved in the pathological process.
- Various infectious diseases (syphilis, brucellosis, tuberculosis).
- Rheumatological pathologies (rheumatoid arthritis, ankylosing spondylitis, reactive arthritis).
- Inflammatory bowel diseases (Crohn's disease, ulcerative colitis).
- Systemic vasculitis (nonspecific aortoarteritis Takayasu and giant cell (temporal) arteritis Horton.
Atherosclerosis of the aorta
The most common cause of hardening of the aorta is atherosclerotic lesion, which is the deposition of cholesterol in its wall. The main sources of aortic atherosclerosis are:
- high blood cholesterol levels;
- hypertonic disease;
- smoking;
- diabetes;
- obesity.
In men, atherosclerosis occurs more often and begins earlier than in women. Almost always, atherosclerosis of the aorta is combined with atherosclerosis of the carotid and coronary arteries (vessels that supply the heart). Blood clots quite often form on cholesterol plaques, which can clog the vessels of the brain, kidneys, intestines, etc. and cause a heart attack of these organs.
Complications
Aortic wall dissection (dissection) and rupture are the main complications of thoracic aortic aneurysm. A ruptured aneurysm can lead to life-threatening internal bleeding. The larger the aneurysm, the higher the risk of it rupturing.
Signs and symptoms of a ruptured aortic aneurysm:
- sudden, intense and constant pain in the abdomen, chest, back;
- pain that radiates (gives) to the back or legs;
- sweating;
- dizziness;
- low blood pressure;
- rapid pulse;
- loss of consciousness;
- dyspnea;
- weakness or paralysis of one side, difficulty pronouncing words, and other signs of a stroke.
Thrombosis.
Another complication of an aortic aneurysm is thrombosis. Small thrombotic masses can form in the area of the aortic aneurysm. If a clot breaks off from the inside wall of the aortic aneurysm and closes blood vessels in another part of your body, it can cause pain or block blood flow to the brain, toes, legs, or abdominal organs.
Diagnostic methods
A thoracic aortic aneurysm is often discovered incidentally during medical tests such as a chest x-ray, ultrasound of the heart or abdomen, performed for other conditions.
If your doctor suspects that you have an aneurysmal dilatation of the thoracic aorta, he may recommend special research methods, such as: Chest X-ray. Your doctor may first suspect a thoracic aortic aneurysm when performing a chest x-ray. The doctor may also prescribe a chest x-ray as the first study to determine whether there are changes in the thoracic aorta. However, X-rays of the chest organs will not allow you to determine the size of the aorta and its length, so the doctor recommends additional research methods.
- Echocardiographic examination (EchoCG). Thoracic aortic aneurysm can be diagnosed by echocardiography. This test method is often used to evaluate family members who have been diagnosed with a thoracic aortic aneurysm. Echocardiography is often used to detect aneurysms in people with Marfan syndrome.
- An echocardiographic study is based on recording sound waves reflected from the structures of the heart. An echocardiogram shows how well your heart beats and how your valves work. Sometimes your doctor may recommend transesophageal echocardiography to better visualize the aorta.
- Computed tomography (CT). This is a painless test that produces very clear images of the aorta. During a CT scan, you must lie on a donut-shaped table called a gantry. X-rays shine through the human body, followed by image processing. One disadvantage of CT is the exposure to radiation, especially in those patients who require frequent monitoring, such as those with Marfan syndrome.
- Magnetic resonance imaging (MRI). MRI is another method of painlessly examining patients. Most MRI machines consist of a large magnet shaped like a donut or tunnel. You lie down on a movable table that goes into a tunnel. The magnet produces signals that vary depending on the type of tissue scanned. The doctor will obtain an image that will reveal the presence of an aortic aneurysm.
Treatment
The main goal of treating patients with thoracic aortic aneurysm is to prevent such a serious complication as aortic rupture. Treatment depends on the size of the aneurysm and how quickly it grows and can range from watchful waiting to surgery.
Medical observation
If you have a small thoracic aortic aneurysm, your doctor may recommend watchful waiting, which includes regular examination and monitoring of the aneurysm. Treatment of other diseases that may worsen aneurysmal disease.
The doctor recommends regular examinations to monitor the size of the aneurysm. If you have been diagnosed with an aortic aneurysm, you should undergo examination at least 2 times a year.
If you have high blood pressure, your doctor will recommend antihypertensive therapy (drugs that lower blood pressure), which will reduce the risk of aortic rupture.
These drugs may include:
- Beta blockers.
Beta blockers lower blood pressure and slow the heart rate. These include: metoprolol (Egilok, Betalloc ZOK), Bisoprolol (Concor), atenolol. - Angiotensin II receptor blockers.
Your doctor may recommend angiotensin II receptor blockers if beta blockers are not enough to lower your blood pressure. These drugs are recommended for patients with Marfan syndrome, even if they do not have high blood pressure. Examples of angiotensin II receptor blockers: losartan, valsartan, olmesartan. - Statins.
These drugs reduce the level of cholesterol in the blood, as a result, atherosclerotic plaques do not form in the arteries and thereby reduce the risk of forming a thoracic aortic aneurysm. Examples of these drugs: atorvostatin, rosuvostatin, simvastatin.
If you smoke, it is very important to quit smoking, as smoking increases the risk of developing an aneurysm.
Surgery
Transplant installation
Surgery is recommended if your aneurysm is 5.6 cm or larger. If you have Marfan syndrome, another connective tissue disease, or someone in your family has been diagnosed with aneurysmal disease, then your doctor will recommend surgical treatment for a smaller aneurysm. Also, depending on your condition of the localization of the thoracic aortic aneurysm, the Doctor may recommend:
- Open surgical treatment.
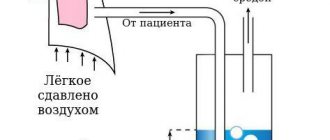
Open surgery involves resection (removal) of the damaged section of the aorta and replacing it with a synthetic tube (prosthesis). After this operation, recovery will take several months. - Endovascular treatment.
The doctor, using special devices, implants an aortic endoprosthesis through the femoral artery. The prosthesis is covered with a metal mesh and is attached to the aorta using small hooks. The prosthesis strengthens weakened areas in the aorta and thereby prevents its rupture. - Other heart surgeries.
If you have damage to the heart valves, then your doctor may recommend additional surgical intervention aimed at correcting the heart valve apparatus, this will stop the worsening of the aortic aneurysm.
Emergency surgical treatment
Emergency surgery is performed when an aortic aneurysm ruptures; unfortunately, with such interventions there is a high risk of death in the perioperative period. Many patients who have aortic rupture die before reaching the hospital.
Treatment methods
I strongly recommend that all patients with atherosclerotic lesions of the aorta quit smoking if such a problem exists. It is important to change your diet by increasing the amount of fish, vegetables and fruits and reducing the amount of fatty meat, lard, and butter. Patients suffering from diabetes need to significantly limit the amount of carbohydrates consumed and control blood glucose levels.
Medicines: what and for how long
Depending on what caused aortic sclerosis, I use different medications:
- Treatment of atherosclerosis requires reducing the concentration of cholesterol in the blood with the help of statins (Rosuvastatin, Atorvastatin). In order to reduce the risk of thrombosis, I prescribe antiplatelet agents (Acetylsalicylic acid, Clopidogrel).
- Infectious diseases may be a reason to prescribe antibiotics. For syphilis - Penicillin, for brucellosis - Doxycycline. Tuberculosis requires the use of special anti-tuberculosis drugs - Isoniazid, Ethambutol.
- Rheumatological diseases and systemic vasculitis. In the case of autoimmune pathologies, to suppress severe inflammation in the aortic wall, I use glucocorticosteroids (Methylprednisolone) or more powerful immunosuppressants (Cyclophosphamide, Methotrexate).
I would like to note that, regardless of the cause of aortic sclerosis, I prescribe antihypertensive medications for high blood pressure:
- for isolated systolic arterial hypertension (high pulse pressure) - calcium channel blockers (Amlodipine) or diuretics (Indapamide, Hydrochlorothiazide);
- in the presence of CHF - ACE inhibitors (Perindopril, Ramipril) or sartans (Losartan, Valsartan);
- in the presence of coronary heart disease - beta-blockers (Metoprolol, Bisoprolol).
Surgical interventions
Surgical treatment methods are used only when an aneurysm has developed. This is necessary to prevent its further growth and its worst consequence - rupture.
The operation is indicated if the aortic diameter exceeds 55 mm.
There are 2 methods of surgical treatment of aortic aneurysm:
- Installation of a stent graft (a metal wire cylinder), which allows to level blood pressure on the weakened walls of the aneurysm, thereby preventing its rupture. The operation is performed under local or general anesthesia. The device is inserted through the femoral vessel and, under X-ray control, reaches the affected area.
- Prosthetics with a conduit (a special tube made of pericardial tissue or synthetic material). When replacing the root and ascending portion, the aortic valve is often also replaced. The operation is performed under general anesthesia on an open chest.
Are folk remedies effective?
On the Internet, by searching “folk remedies for treatment of atherosclerosis of the aorta of the heart,” you can find a lot of alternative medicine recipes that promise not only an improvement in the patient’s condition, but also a complete cleansing of all the vessels of the body. Unfortunately, none of them has an evidence base. Their use, at best, will be simply useless, and at worst, harmful and even life-threatening.
Many components of herbs can interact with medications prescribed by a doctor (for hypertension, to lower blood cholesterol, etc.). This leads to the fact that either the therapeutic effect of the drug will worsen, or the likelihood of adverse reactions, sometimes very severe, will increase.
Lifestyle and taking medications at home
There are no medications that can prevent the formation of a thoracic aortic aneurysm, but medications that lower blood pressure and cholesterol levels can reduce the risk of developing complications of a thoracic aortic aneurysm.
In order to prevent the formation and growth of a thoracic aortic aneurysm, keep your blood vessels as healthy as possible. The following is required:
- Quit smoking.
- Monitor blood pressure.
- Exercise regularly.
- Reduce cholesterol and fat levels in your diet.
If you have risk factors for developing an aortic aneurysm, talk to your doctor. If necessary, the Doctor will recommend medications to you, including medications that lower blood pressure, thereby reducing the load on weakened arterial vessels. You should also undergo screening examination (EchoCG) for several years.