Briefly about the diagnostic method
Echocardiography (EchoCG) is a test that uses high-frequency sound waves (ultrasound) to view the structure and study the function of the heart.
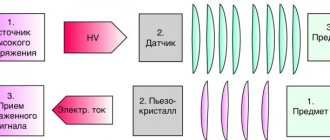
The common non-medical name for this test is cardiac ultrasound. The research is absolutely harmless to humans. Echocardiography uses reflected ultrasound waves to create images of the heart, its chambers, valves, walls and vessels (aorta, pulmonary arteries and veins). The sensor of the ultrasound machine is located on the chest and sends ultrasound waves that are reflected from the heart and again captured by the sensor, after which the signal is transmitted to the device, where it is converted into an image understandable to a specialist. If it is necessary to assess coronary reserve, stress echocardiography methods (stress echocardiography) are used.
Indications and contraindications for diagnosis
Echocardiography is prescribed to detect heart disease and evaluate its function. Most often, an echocardiogram is prescribed by a cardiologist; in preparation for major vascular operations, an ultrasound of the heart can be prescribed by the attending physician or an anesthesiologist-resuscitator.
Echocardiography can reveal:
- The size and shape of your heart, the thickness and movement of the heart walls.
- Assess the pumping function of the heart - ejection fraction
- Check the condition of the heart valves, whether the valves are closed, whether there is a narrowing in the valve area.
- The presence of cardiac aneurysms, blood clots in the cavities of the heart.
- Abnormal openings between the atria or ventricles.
- Identify the presence of an infectious process on the valves.
- During echocardiography, you can evaluate the pressure in the pulmonary artery and its size
- Identify aneurysms of the ascending aorta.
- Fluid accumulation or disease in the outer lining of the heart (pericardium).
- Heart tumors.
Echocardiography is a safe study and has no contraindications.
2D echocardiography
Using two-dimensional echocardiography, you can obtain any cross-section of the heart and great vessels. Because the heart is a three-dimensional organ, and real-time echocardiography can only image in a two-dimensional plane, a detailed understanding of the structure of the heart can be obtained using multiple sections. Each specific structure in the heart can be studied using two mutually perpendicular (longitudinal and transverse) sections and several intermediate ones. Depending on the position of the sensor, the angle of inclination and its rotation, it is possible to obtain a continuous spectrum of sections of the anatomical structures of the organ, which makes their identification difficult. In this regard, when studying the ultrasound anatomy of the heart, standard sensor positions, as well as standard projections, are proposed. Standard projections (sections) were selected in order to select from the entire variety the most informative structures that are easily accessible for identification.
Typically, cardiac examination is carried out in projections along the long and short scanning axes, as well as from non-standard (subxiphoidal, suprasternal) approaches.
Parasternal projections
Fig.5
Parasternal long axis view of the left ventricle in diastole (left) and systole (right).
RV - right ventricle; IVS—interventricular septum; LV - left ventricle; LA - left atrium; Ao - aorta.
The projection of the long axis of the left ventricle (Fig. 5) with a parasternal placement of the sensor corresponds to a sagittal section along the long axis of the heart. To obtain this projection, the sensor is installed in the III-IV intercostal space to the left of the sternum, the beam is directed along the long axis of the heart (approximately parallel to the line connecting the right shoulder and left thigh of the subject). In this projection, the inflow and outflow tracts of the left ventricle are visible. An oval contour of the left atrium is visualized under the aortic root. The anterior and posterior mitral leaflets separate the atrium from the ventricle. The anterior mitral leaflet is larger than the posterior one, the anterior and posterior papillary muscles can be observed by slightly tilting the sensor to the left and right. In the parasternal long axis view, the position of the mitral valve and interventricular septum and their relationship to the aortic root are determined. Normally, the anterior mitral valve at the same depth passes into the posterior wall of the aorta (mitral-aortic fibrous continuation), the interventricular septum passes into the anterior wall of the aorta (septal-aortic contact). The projection allows us to identify the relationship of the great vessels with the left atrioventricular valve and the interventricular septum, and to detect a violation of the outflow from the left ventricle. The great vessel is connected to the ventricle if more than 50% of the lumen of the vessel is in this ventricle.
To obtain a parasternal projection of the long axis of the left ventricle during cardiac dextraposition, the sensor is placed parasternally in the 3-4 intercostal space on the right and oriented in the direction between the right shoulder and left thigh.
Projection of the inflow tract of the right ventricle.
This section is obtained from the parasternal position of the long axis of the left ventricle by tilting the sensor to the right. The cavities of the right atrium and ventricle, as well as the anterior and posterior leaflets of the tricuspid valve, are visualized. By directing the section towards the sternum, the septal cusp of the tricuspid valve can be visualized. The section is used to assess the anatomical relationships of the right structures of the heart.
Projection of the right ventricular outflow tract
Fig.6
Parasternal view of the right ventricular outflow tract in systole (left) and diastole (right).
LV - left ventricle; RVOT—right ventricular outflow tract; LA - pulmonary artery; MV - mitral valve.
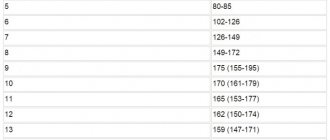
This section (Fig. 6) is obtained by rotating the sensor clockwise, approximately 50-60o from the longitudinal axis of the left ventricle. The echocardiogram visualizes the pulmonary artery to the level of the bifurcation, the pulmonary valve and the right ventricular outflow tract. The section also includes a portion of the left ventricle, the anterior and posterior mitral leaflets. Normal values of the inflow and outflow tracts of the right ventricle in children, depending on age, are shown in Table 5.
Short axis projections with a parasternal position of the sensor.
To obtain these projections, it is necessary to rotate the sensor 90o from the long axis projection. In this case, it is possible to obtain several sections along the short axis by tilting the sensor from the base to the apex of the heart.
At the level of the base of the heart, a cross-section of the aortic root is revealed in the form of a rounded shadow with thin semilunar valves (Fig. 7). The right ventricular outflow tract and pulmonary artery are located anteriorly and surround the aorta. Below the aorta is the left atrium; elements of the tricuspid valve are visualized on the right. If the probe is tilted above the aortic valve, the ostia of the left and right coronary arteries can be visualized. The location of the mouth of each coronary artery varies individually both in height and in circumference of the aorta.
Typically, the right coronary artery arises at 10 o'clock from the right coronary sinus, the left at 3 o'clock from the left coronary sinus. The venomless (posterior) sinus does not have a coronary artery ostium.
By assessing the relationship of the great vessels, it is possible to identify anomalies in their position. In order to reliably determine which vessel is the aorta and which is the pulmonary artery in the case of an abnormal position of the vessels, it is necessary to trace the course of the vessels along their length (along the longitudinal and cross sections) and identify either the aortic arch with the vessels originating from it, or the bifurcation of the pulmonary artery. The short axis projection at the level of the great vessels makes it possible to establish the condition of the semilunar valve leaflets, identify stenosis or insufficiency, and indirectly assess the presence of pulmonary hypertension.
Fig.7
Parasternal cross-sectional projection at the level of the great vessels in diastole (left) and systole (right).
RVOT—right ventricular outflow tract; PV—pulmonary valve; Ao - aorta; AS - interatrial septum.
Fig.8
Parasternal cross-sectional view at the level of the mitral valve in diastole (left) and systole (right).
RV - right ventricle; LV - left ventricle; MV - mitral valve.
At the level of the mitral valve, a cross-section of the left ventricle is revealed, with the mitral valve leaflets located one above the other, during ventricular systole the leaflets are closed in the form of a single line, and during diastole they limit the contour of the left atrioventricular opening (Fig. 8). In front and to the right is the right ventricle, separated from the left by the interventricular septum, its muscular part. This projection is used to assess the condition of the mitral valve leaflets, commissures, left atrioventricular fibrous ring, ventricular septal defects, the size of the ventricular cavities and other anomalies.
At the level of the papillary muscles, a cross-section of the left ventricle is revealed, and the lateral and medial groups of papillary muscles are visualized (Fig. 9).
A cross-section of the left ventricle at the level of the apex is obtained from the parasternal position by maximally deflecting the sensor from previous positions to the apex of the heart. A rounded shadow of the apex without contours from the papillary muscles is visualized. The projection is used to visualize apical hypertrophy as well as apical ventricular septal defects.
Fig.9
Parasternal cross-sectional view at the level of the papillary muscles of the mitral valve in diastole (left) and systole (right).
RV - right ventricle; IVS—interventricular septum; PM - medial and lateral groups of papillary muscles.
Projection of four cameras from the top
Fig.10
Apical projection of the 4 chambers of the heart in diastole (left) and systole (right).
IVS—interventricular septum; LV - left ventricle; RV - right ventricle; LA - left atrium; RA - right atrium;
To obtain this projection, the sensor is placed in the area of the apex of the heart and directed slightly upward and to the right until an image of the four chambers is obtained (Fig. 10), while achieving a position at which the maximum excursion of the mitral and tricuspid valves is visible. In this projection, all chambers of the heart, the interventricular and interatrial septa, and the central fibrous body, where the atrioventricular valves are attached, are visible. If you deflect the sensor towards the xiphoid process, the initial portion of the ascending aorta and the outflow tract of the right ventricle enter the section.
This projection is more often used in the diagnosis of septal defects, the relative position of the atria and ventricles, as well as anomalies of the atrioventricular valves.
Subcostal projections
To obtain a two-dimensional image from a subcostal approach, the sensor is installed under the xiphoid process, tilting it towards the heart to achieve a clear image of it. Depending on the depth of the probe, the cutting planes can pass through different structures. The deep plane passes through all 4 chambers, while the inflow portion of the interventricular septum, the interatrial septum and atrioventricular valves are visualized. With less deep penetration of the slice plane, a projection of the long axis of the left ventricle is formed. When the sensor is directed superficially, the cutting plane passes through the right ventricular outflow tract.
Suprasternal projections
To obtain suprasternal access, the sensor is installed in the area of the jugular fossa. The subject is in a lying position with a cushion placed under his shoulders and his head thrown back.
This approach is used to visualize the aortic arch, aortic isthmus and descending aorta. The aortic arch bends around the right branch of the pulmonary artery (Fig. 11).
Fig.11
Suprasternal projection of the aortic arch.
Ao arc - aortic arch; PA - right branch of the pulmonary artery.
How is the diagnosis carried out?
When performing an ultrasound of the heart, the patient is placed on his back or left side. During echocardiography, the sensor can be positioned in different planes for better visualization of the heart chambers. The sensor and the patient's skin are moistened with a special water-soluble gel, which ensures tight contact between the sensor plane and the body.
Our cardiac ultrasound machines allow us to perform various types of echocardiography. One-dimensional echocardiography in M-mode allows you to reproduce the movement of the heart walls and valves in the form of a graph, which allows you to evaluate the function of the ventricles.
Two-dimensional echocardiography shows a section of the heart in a certain projection and allows you to determine the size of the cavities of the ventricles and atria, the thickness of their walls, evaluate the movements of the valves and walls of the ventricles, and identify thrombosis of the cavities of the heart.
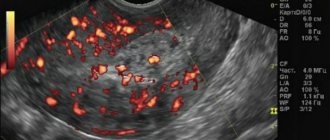
Using Doppler mapping, it is possible to identify the speed and direction of blood flow in the cavities of the heart, which makes it possible to determine valve insufficiency or stenosis, defects of the interatrial and interventricular septa.
The usual procedure for echocardiography involves first identifying the heart valves; heart septum. Next, the pattern of movement of the valve leaflets is revealed, the thickness of the walls and the size of the cavities of the heart are measured. Finally, Doppler echocardiography is performed to detect stenosis or insufficiency of the heart valves and pathological holes in the heart septa.
Interventional echocardiography
Echocardiography is increasingly used in minimally invasive and transcatheter procedures. This primarily concerns three-dimensional echocardiography and transesophageal echocardiography in 3D/4D modes. Lang notes that these techniques allow the surgeon to “see into the chest,” making procedures much easier to control. 3D/4D echocardiography is used in complex procedures such as transcatheter aortic valve replacement (TAVR), transcatheter left atrial appendage closure with Watchman device, closure of atrial septal defect (ASD), closure of ventricular septal defect (VSD), closure of patent foramen ovale (PFO) , transcatheter occlusion of transvalvular regurgitation. It plays an even more important role in transcatheter mitral valve replacement (TMVR) and mitral valve reconstruction using the MitraClip. During these interventions, it is used for navigation, device sizing, and monitoring correct valve placement.