GEF in pregnant women and newborns. What should parents do?
Most often, a hyperechoic focus is harmless.
A dense area of the myocardium may be associated with an abnormal chord; a newborn baby with a similar problem should be under medical supervision to avoid problems with impaired blood flow and arrhythmia. The short accessory chord also requires attention, as it interferes with the functioning of the ventricle. An extra chord in the right ventricle is considered more dangerous; in some cases, parents are informed that surgical intervention may be required.
To prevent problems, parents who have hereditary problems in the family are referred to a geneticist for consultation. A geneticist collects a family history to confirm or exclude genetic, occupational and household risk factors. In addition, the geneticist evaluates the level of health of the parents, spermatogenesis, data on andrological and genealogical hereditary burden.
A geneticist, having identified a pathology in a married couple planning parenthood, takes measures aimed at eliminating mutagenic factors that can lead to GEF. The greatest effect is achieved by measures taken two or three months before pregnancy.
If an echogenic focus is nevertheless detected, then the reasons may be:
- mineralization of blood vessels in the myocardium;
- additional septum in the heart;
- chromosome pathology.
The detection of a chromosomal pathology most often confronts a woman with the possibility of terminating her pregnancy. In other cases, GEF is considered normal, and its signs completely disappear by the age of four years of the child’s life. Before this period, the child should be observed by a cardiologist.
Like any procedure associated with interference with the body, aspiration carries the risk of miscarriage. But in the case of diagnosing genetic abnormalities, such interventions are necessary, as they help exclude Down syndrome and other severe hereditary diseases.
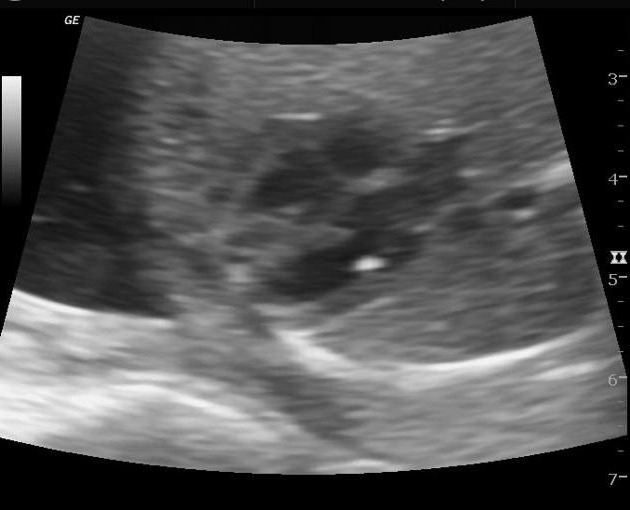
During a second routine ultrasound, a hyperechoic focus is often detected in the left ventricle of the fetal heart. This inclusion is a small point - an additional chord, which does not cause any harm to the child, but provided that the presence of chromosomal pathologies is excluded.
What to do next
Genetic blood test
If an ultrasound examination reveals a hyperechoic focus in the left ventricle of the fetal heart, further examination is necessary. What and how to do next will be determined by your attending physician. If necessary, a number of additional examination methods may include:
- A genetic blood test aimed at identifying chromosomal abnormalities in the fetus.
- Echocardioscopy is a diagnostic method performed from 18 to 25 weeks. Important parameters of the fetal heart are assessed. There are certain indications for this method: age over 35 years, diabetes mellitus (DM), infections of the pregnant woman in the early stages, detection of pathology of the heart muscle (myocardium) of the fetus in the early stages, delay in fetal development according to the timing, there is a heart defect in the pregnant woman or relatives relatives.
In more rare cases, the following diagnostic methods may be prescribed:
- Study of placental cells for the genetic characteristics of the fetus. This method (placentocentesis) allows you to determine the diagnosis as early as possible.
- Fetoscopy is an examination of the amniotic sac. Amniocentesis - analysis of the composition of amniotic fluid. The level of hormones, biochemical and immunological parameters is studied. It is possible to assess the risk of a chromosomal abnormality.
Hyperechoic focus in the left ventricle of the fetal heart: what is it, is it dangerous?
An additional chord in the heart of a child.
chord in the left ventricle. false chord At an early stage of pregnancy, during a repeated ultrasound examination, the expectant mother may be puzzled by the news about the presence of such a diagnosis as a hyperechoic focus in the left ventricle of the fetal heart.
Such an incomprehensible combination of words, undoubtedly, can plunge one into a state of shock and cause the most sincere worry and anxiety in any woman who is not experienced in the subtleties and specifics of medical terminology.
A similar diagnosis is currently found in almost every fourth fetus. It is worth highlighting that there is no unanimous opinion among scientists and doctors regarding this formation in the heart of the fetus.
Most are inclined to argue that the hyperechoic focus is a unique, slightly modified version of the norm. The exception is those cases when the focus of increased echogenicity is detected against the background of symptoms and signs indicating pathological abnormalities at the genetic level.
If all of the above is translated into simple language, the conclusion will be quite optimistic. Diagnosing a hyperechoic focus in the left ventricle of the heart in a fetus does not pose any danger to the child’s health; the only exceptions are those cases when there are abnormalities in the chromosomes.
GEF in the ventricles of the fetal heart
The frequency of occurrence is about 7%. GEF in the ventricles of the fetal heart is a small formation inside the heart cavity, which, when performing ultrasound, is comparable in echostructure to bone tissue. The main ultrasound criteria for pathology include:
- Size from 1 to 6 mm;
- Location – on the papillary cardiac muscle or on the chordae tendineus;
- Most often detected in the left ventricle (94% of cases);
- Does not produce a specific sound shadow during ultrasound;
- Moves in sync with the heart valves.
Alternative names for GEF in the ventricles of the fetal heart are “golf ball”, “pea”. An ultrasound diagnostic doctor will not always be able to detect changes in the cavities of the fetal heart, but in any case, if a “pea” is detected, there is no need to panic. Possible outcomes of the GEF include:
- Reduction in size and disappearance during pregnancy (about 30%);
- Preservation throughout the entire period of gestation and absence of problems after the birth of the child (about 60%);
- Detection of changes in the heart of a newborn baby (3-5%), which do not require surgery and disappear on their own by the age of 4 years of the child’s life.
In rare cases, when GEF is combined with other signs of congenital anomalies, it can be expected that additional examination using invasive diagnostic methods will reveal chromosomal abnormalities or malformations in the child.
Echocardioscopy
Features of blood circulation in the fetus. fetal blood circulation. anatomical and physiological features of the fetal cardiovascular system
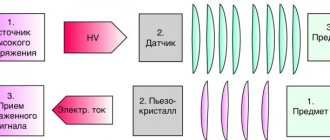
When diagnosing a focus of increased echogenicity of the left ventricle in a fetus, the use of echocardioscopy for detailed monitoring of the functioning of the heart muscle will be an effective step. This procedure allows you to monitor the main parameters of the fetal heart (atrial filling, ventricular contraction, etc.) in real time using ultrasound and detect possible deviations from the norm.

Cardiac echocardioscopy is the study of the structure of the heart and its functioning using ultrasound.
The main indications for examination using echocardioscopy are:
- the age of the pregnant woman exceeds 36 years;
- the presence of diabetes mellitus in the expectant mother or immediate relatives;
- recent infectious or viral disease in the early stages of pregnancy;
- the woman has a congenital heart defect, taking into account immediate relatives;
- the presence of markers of hereditary pathology in the blood of the expectant mother.
Echocardioscopy is an appropriate and effective method only up to the 25th week of pregnancy. At later stages, the procedure will be ineffective due to the large size of the fetus and the small amount of amniotic fluid.
Materials and methods
Observation 1
. A 39-year-old pregnant woman applied to the Regional Perinatal Center for a routine ultrasound examination at 18-19 weeks. Second pregnancy. The first pregnancy ended in the birth of a child with Down syndrome and a congenital heart defect: atrioventricular septal defect. The parents are somatically healthy, there is no family history, and no exposure to teratogenic factors has been noted. An ultrasound examination in the first trimester of pregnancy did not reveal any abnormalities. Combined screening low risk of trisomy. Ultrasound examination was performed on an Accuvix XG device (Samsung Medison) using a 2-6 MHz transabdominal probe.
Observation 2
. A 32-year-old primigravida came to our center for a routine ultrasound examination at 19-20 weeks. The family history of both parents is not burdened. The patient is somatically healthy and has been registered with the antenatal clinic since 8 weeks of pregnancy. Combined prenatal screening at 12 weeks did not reveal any pathology. Ultrasound examination was performed on a Voluson E8 Expert device (GE Heathcare) using a multifrequency transabdominal sensor 4.0-8.5 MHz.
What is a hyperechoic focus?
Pyeelectasia in the fetus. pyeelectasis of the kidneys in the fetus: treatment and causes
Hyperechoic focus or HEF is an incidental finding during ultrasound examination of a pregnant woman
Ultrasound of the fetal heart is a mandatory component of any perinatal screening, so the doctor always pays attention to the structure and functioning of the child’s heart
The woman regularly, without any complaints or worries, comes for an ultrasound scan, where the doctor discovers such an interesting feature of the structure of the fetal heart. We hasten to reassure expectant mothers that GEF is only an “interesting feature” and not an anomaly or pathology. The hyperechoic focus itself does not in any way affect the functioning of the heart of the fetus or an already born child, which has been confirmed in numerous studies.

As a rule, such an area is found during the second screening ultrasound - at 18-22 weeks of pregnancy and is observed until the third trimester, sometimes until childbirth. According to statistics from different countries, such a formation is more often found in the left ventricle of the fetus, less often in the right ventricle or other chambers of the heart. On average, in 7% of pregnancies a hyperechoic focus of various locations is detected. In developed countries, there is even evidence that approximately a fifth of such findings are erroneous due to the poor quality of the ultrasound machine or incorrect conduct of the research procedure. Below we will talk in a little more detail about what is associated with the appearance of such heart focuses.
On an ultrasound examination, the doctor sees a bright white spot within 2-3 mm of a rounded shape in the cavity of one of the chambers of the fetal heart. Ultrasound diagnosticians are very fond of all kinds of artistic comparisons, so the hyperechoic focus is also called golf ball or golf ball symptom. In fact, the small round structure that bounces with every heartbeat actually resembles a golf ball.
Only a very dense formation akin to bone tissue can give such a picture on an ultrasound, which causes some surprise to all scientists and doctors. How such a dense formation forms in the heart muscle and then disappears without a trace after birth remains an unsolved mystery.
results
Observation 1
. An ultrasound examination revealed one living fetus. Fetometry indicators corresponded to 18–19 weeks of pregnancy (biparietal size - 41 mm, fronto-occipital size - 56 mm, head circumference - 186 mm, abdominal circumference - 135 mm, femur length - 35 mm, humerus length - 31 mm, transverse size of the cerebellum – 19 mm). When examining the chest organs, pronounced cardiomegaly was noted. A study of the fetal heart in a four-chamber section revealed that the left ventricle was enlarged to 28 mm in diameter due to significant diffuse protrusion of the walls, mainly in the free and diaphragmatic sections (Fig. 1). The contractility of the free and diaphragmatic walls was minimal. In color Doppler mapping mode, normal blood flow was recorded through the right parts of the heart, while in the left ventricle itself and through the aortic valve, blood flow was recorded only at minimal speeds (4 cm/s) (Fig. 2). There was no pericardial effusion. The course of the main arteries and the cut through three vessels are not changed. Considering the severe aneurysm and the poor prognosis, the parents decided to terminate the pregnancy. A pathological autopsy confirmed the diagnosis of a left ventricular aneurysm: cardiomegaly predominantly due to the left ventricle and thinning of the left ventricular wall (Fig. 3).
Observation 2
. Ultrasound examination revealed one living fetus. Fetometry indicators corresponded to 19-20 weeks of pregnancy (biparietal size - 48 mm, fronto-occipital size - 64 mm, head circumference - 177 mm, abdominal circumference - 151 mm, femur length - 34 mm, humerus length - 30 mm, transverse the size of the cerebellum is 20 mm). The fetal liver was moderately enlarged, there was no ascites or hydrothorax. A study of the fetal heart in a four-chamber section revealed an enlarged left ventricle, mainly due to the apical part (the distance from the valve to the apex is 18 mm in diastole). Ventricular contractility was partially preserved. Extrasystoles with poorly recorded blood filling of the aneurysmal sac were periodically recorded. In color Doppler mapping mode, blood flow through the left heart was partially preserved. The parents decided to terminate the pregnancy. A pathological autopsy confirmed the diagnosis of a left ventricular aneurysm: cardiomegaly mainly due to the apical part of the left ventricle and thinning of its posterior wall, hepatomegaly.
What's wrong?
RESULTS µÑдÑа плода - ÑÑо овалÑно-окÑглое обÑазоваР½Ð¸ the RESPONSIBILITY. RESULTS ROOM »ÐµÐ³ÐºÐ° покаÑиваеÑÑÑ Ð¿Ñи биении ÑеÑдÑа. RESULTS ROOM 35 years, аÑакже Ñ Ð°Ð·Ð¸Ð°Ñок.
What is the GEF of the fetal heart?
This conclusion was first found in medical literature at the end of the 19th century in Great Britain, and was described at the same time. Most often, the disorder is diagnosed in women after 35 years of age, and predominantly in Asian women. On ultrasound, the GEF appears on the monitor as a small white dot in the area of the heart, usually in the left ventricle. If the image is enlarged several times, an oval-round formation will become clearly visible, moving slightly with each heartbeat. That is why this violation is often called a “golf ball.”
The formation occurs due to compaction of the elastic structures of the myocardium (heart muscle). Typically, ultrasound specialists find a similar area in women at 18-22 weeks of pregnancy during a repeat (second) screening ultrasound. The lump may remain until the third trimester, and in some cases until the birth of the baby.
The "golf ball" phenomenon

The "golf ball" phenomenon
You come for the second screening, and they tell you that the child has a hyperechoic focus in the left ventricle. “Hyperechoic” means that the area has increased brightness (density) against the background of heart tissue. The “golf ball” phenomenon arose because such a hyperechoic inclusion is shaped like a golf ball and bounces like a ball when the heart beats. Most often, a hyperechoic focus (HEF) is found in the left ventricle (LV), less often in the right ventricle (RV) and other chambers of the heart. It still remains a mystery why such a hyperechoic focus (HEF) in the heart muscle, which has bone density, disappears without a trace after birth.
Reasons for education
We have found out what a hyperechoic focus is, but what are the reasons for its appearance? This:
- salt deposits;
- pathology in the chromosome set of the fetus;
- the presence of an additional chord in the heart, which is considered a normal variant and does not in any way affect the activity of the heart muscle.
If the appearance of compaction of myocardial structures was caused by salt deposition, then a pregnant woman has no reason to worry. Most often, such minor pathology goes away by the third trimester of pregnancy.
An additional chord in the heart is a structural feature that can create certain heart murmurs. At the age of 2-3 years, noises most often stop, but even if they remain, they do not pose a danger to the life and health of the child.
It’s another matter if the focus is caused by an incorrect set of chromosomes in the child. There is a risk of detecting Down syndrome in the fetus or other pathologies. If there is such a suspicion, additional tests are prescribed to clarify this information. However, most often the alarm turns out to be false.
The causes of a hyperechoic focus in the left ventricle of the fetal heart are individual and require examination to clarify them.
Possible reasons
Problems of intrauterine development most often arise against the background of the following factors:
- Intrauterine infection with viruses or bacteria;
- Chromosomal aberrations (calcium deposits on the walls of the heart cavities are common in children with Down syndrome);
- Congenital fibrous tissue dysplasia;
- Vascular disorders and fetal heart dysfunction;
- Immunological disorders due to underdevelopment of the thymus;
- Anomalies of heart development in a baby.
GEF in the area of the heart in a baby is serious: if there are risk factors, the doctor will prescribe an additional examination to exclude a dangerous congenital pathology in the baby.

After identifying a hyperechoic focus in the fetal heart, you should be observed by a doctor and do an ultrasound as prescribed by the doctor
Action tactics
In most cases, if a hyperechoic inclusion is detected, additional research is indicated. In this case, they can assign:
- repeat ultrasound to clarify the diagnosis;
- echocardioscopy (performed only until the 25th week);
- blood chemistry;
- karyotyping.
Invasive diagnostic procedures are used quite rarely:
- amniocentesis (taking a sample of amniotic fluid through the abdominal wall);
- placentocentesis (biopsy of placental cells);
- fetoscopy (examination of the fetus using a video probe).
First of all, of course, genetic causes of hyperechoic inclusion should be excluded. To do this, the diagnostician searches for other small markers of chromosomal pathologies. These include congenital heart defects, thickening of the cervical fold, developmental disorders of the gastrointestinal tract and skeletal system. They are usually detected during ultrasound examination. If they are detected, consultation with a geneticist is necessary.
If no additional signs are found, the fetus can be considered completely healthy. However, a follow-up echocardiogram is recommended in the first months after birth. This procedure will make sure that there are no pathological changes.
GEF in the ventricles of the fetal heart: medical tactics
In most cases, if a “golf ball” is detected in the area of the child’s heart, it is necessary to continue observation: a control ultrasound examination during pregnancy should be performed by a certified diagnostician using a modern 3D device. If there is a suspicion of chromosomal abnormalities in the fetus, one must agree to invasive research methods.
After the birth of a child, it is important in the first days and during the first years of the baby’s life to be regularly examined by a pediatrician and cardiologist.
Detection of any changes in the baby’s heart is a significant reason for a careful assessment of the child’s intrauterine development.
What to do if GEF is detected?
As already mentioned, this deviation does not require specific treatment. In approximately 30-35% of cases, the lump disappears on its own by the end of pregnancy. In approximately 80% of newborns, it turns into an additional trabecula in the internal tissue of the ventricles of the heart. Such formations also do not affect health and do not require treatment. Based on the above, you should only worry about the presence of such a disorder after repeated screening if there are other syndromes that may indicate genetic diseases.
If the doctor detects several markers (signs) of such an anomaly at once, he prescribes an additional medical genetic consultation, as well as other studies to determine the diagnosis. After this, if necessary, treatment is prescribed or other further actions for the management of pregnancy and childbirth are discussed with the mother.

Pregnant women often encounter unfamiliar terms during ultrasound examinations, which become causes of concern. Hyperechoic focus in the left ventricle of the fetal heart is one such term that requires explanation. What is a hyperechoic focus? How dangerous is this?
Doctors believe that most often GEF is a variant of the norm; the disorder becomes a pathology only when abnormalities in the structure of chromosomes are detected.
On ultrasound, the GEF appears as a white dot located in the area of the heart. In a certain section, the point looks like a white ball that bounces when the heart muscle contracts.
The appearance of a white dot indicates a denser structure of the heart muscle.
- Deposition of calcium salts.
- Abnormal structure of the heart.
- Chromosomal disorder.
The deposition of calcium salts should not cause concern; it will resolve by the time the baby is due to be born.
A hyperechoic focus in the left ventricle of the fetal heart, caused by the development of an extra chord, does not affect the functioning of the heart, but can cause murmurs, so children with such anomalies are observed by a cardiologist. Chromosomal abnormalities are of greater concern. They can be detected by a blood test ordered by a geneticist. A hyperechoic focus in the fetal heart plus chromosomal abnormalities is evidence of severe pathologies, including Down syndrome.
Developmental defect or sign of chromosomal abnormalities

Excessive impregnation with calcium salts
Yes, yes, this is exactly the reaction that a similar conclusion from an ultrasound diagnostic doctor can cause in parents. In fact, neither one nor the other is true. A hyperechoic focus in the left ventricle of the fetal heart is not a malformation or an anomaly. Many parents are afraid that this kind of finding in the child’s heart is a sign of severe chromosomal pathology, for example, the presence of Down syndrome. To date, there is no scientific evidence that the presence of a hyperechoic focus in the left ventricle of the fetal heart is a reliable sign of chromosomal pathology in the absence of other signs.
Why does such a focus of increased density occur in the prenatal period? There are several possible reasons.
- Excessive impregnation of calcium salts (calcification) of a certain area of the heart muscle. Most often, such changes are localized in the area of the papillary (papillary) muscles. The second trimester of pregnancy, during which such changes are most often detected, is characterized by active mineralization of the child’s musculoskeletal system.
- The presence of an additional or false chord in the ventricle of the child’s heart. Such a false or additional chord does not carry a functional load, and is not a pathology, but refers to minor anomalies of cardiac development (MADC). This phenomenon is a common finding during ultrasound examination. The chords themselves in the prenatal period can provoke the deposition of calcium salts, as well as increase the brightness of the hyperechoic focus.
- One of the signs indicating chromosomal pathology. Let us remind you once again that in the absence of other reliable signs of chromosomal pathologies, the presence of a compaction or hyperechoic focus in the left ventricle of the fetal heart does not indicate genetic disorders.
Carrying out echocardioscopy
If GEF is detected in a child and there are certain indications, the patient is referred for fetal echocardioscopy.
Abnormal cardiac image abnormal heart rhythm palpitation defect defect other mucus instrument increased nodular translucency abnormal urinary flow abnormal amniotic fluid volume. Congenital heart defect Diabetes preeclampsia Phenylketonuria Systemic lymphadenopathy. Increased transventricular abnormalities, cardiac arrhythmias, abnormal arteries of the heart, other abnormalities in the abdomen. Miscarriage Miscarriage during pregnancy Several pregnancies. . According to various sources, hypergenic lesions occur in the range of ± 2-5% in all healthy fats in the second trimester of pregnancy.
Indications for echocardioscopy:
- first pregnancy in women over 35 years of age;
- diabetes;
- infectious disease of the expectant mother;
- identified pathologies in the structure of the heart;
- the child is developmentally delayed;
- relatives of a pregnant woman suffer from heart defects;
- Markers of genetic diseases have been discovered.
Echocardioscopy is performed until the 28th week of pregnancy, after which the method becomes uninformative due to the large size of the fetus and the small amount of amniotic fluid.
Many publications and web pages report that hyperechoic flashes are more common in men with abnormal chromosomes. During each test, the doctor accurately assesses fetal development, including the structure and function of the heart. Ultrasound illustrates the amount of cardiac cavity, valve function, and proper blood flow and contractility of the heart.
Only an experienced specialist can do this, who can accurately assess the structure and functioning of the child’s heart. After about 30 weeks, the light tissue is better developed, the pelvic fins are more calcified, the distance from the heart is greater - all of these factors cause the image of the heart to become less noticeable.
The study is used to assess the size of the valves and cavities of the heart, its contractility and the level of blood filling.
What is the GEF?
We also recommend: When does the fetal heartbeat begin?
To refer to a hyperechoic focus in the left ventricle of the fetal heart, doctors use the characteristic term “golf ball.”
This phenomenon was first described in medical literature at the end of the 19th century in Foggy Albion, when this term was first used.
Most often, such an inclusion is found in women over 35 years of age, predominantly of the Asian race.
During ultrasound examination, the focus of echogenicity on the monitor appears as a small, white dot located in the area of the heart, most often in the left ventricle.
With a more detailed study, if the ultrasound image is enlarged several times, you can see a clearly visible formation, slightly oval in shape, which seems to jump with each contraction of the heart. This is what explains the use of the term “golf ball”.
In the place where the hyperechoic focus of the left ventricle is found, the elastic structures of the heart muscle become denser.
In most cases, such compaction is caused by a number of related factors:
- deposition of excess calcium salts;
- pathologies at the genetic level;
- the formation of an additional string (a kind of thread stretched from the heart valves to the ventricles), the presence of which in most cases does not affect the normal functioning of the fetal heart.
If the formation of a compaction in the left ventricle of the fetus is caused by one of the above factors, then there is no reason for concern.
In cases caused by the deposition of excess calcium salts, the formation occurs on its own. In most cases, the string disappears even before birth and does not pose a danger to the health of the unborn child. Of course, it can cause small murmurs heard in the left ventricle, which also in most cases disappear by the third year of life.
The only recommendation when detecting a heart murmur is to monitor the dynamics of this formation by a cardiologist
A hyperechoic focus in the left ventricle of the fetal heart can be a dangerous pathology only if its diagnosis is accompanied by the presence of a genetic abnormality or chromosomal defect (the appearance of an additional chromosome section). In 20%, the presence of a compacted inclusion in the cavity of the fetal heart may be a sign of the presence of Down syndrome.
When is it discovered?
It is impossible to determine the fetus on an ultrasound before the heartbeat begins, so it is important to understand what time the fetus’s heart begins to beat. The formation of the heart muscle occurs in the 4th week of pregnancy, a week after this you can feel the first tremors
If at the 5th week of pregnancy a heartbeat cannot be heard by transvaginal ultrasound, then there is a high probability of fetal fading.
Using ultrasound diagnostics, it is possible to detect pathology at 18-22 weeks of pregnancy, when a second ultrasound of the fetus is prescribed. There are cases when the pathology disappeared in the last trimester of pregnancy.

Should I worry about this diagnosis?
As a rule, a hyperechoic focus in the left ventricle of the fetal heart does not pose a danger to the child. After birth and a routine examination by a doctor, no deviations from the norm are detected in children; only minor noises are possible in the presence of an additional chord.

When the child reaches the age of 2-3 months, for greater peace of mind for the parents, an ultrasound of the heart can be done, which will detail all the sizes of the cavities and valve openings, the number of additional chords and the general condition of the cardiovascular system. In conclusion, a diagnosis will be written about the health of the heart and full compliance with age characteristics (usually, before the age of one year, children are diagnosed with an open foramen ovale).
Only in a small percentage of cases, an additional chord of the left ventricle in a child can lead to heart disease or other pathologies. But for this, the mere presence of “golf ball” syndrome is not enough; precise confirmation of the danger is necessary through sampling of amniotic fluid or blood from the umbilical cord and the presence, after diagnosing the blood, of pathological markers indicating the presence of chromosomal abnormalities in the fetus.
Ultrasound examination is one of the most informative and important during pregnancy. It allows you not only to see the gender of the unborn child, but also makes it clear whether the baby is developing normally and whether he has any defects or diseases. But the terms used by doctors are not always clear to expectant mothers. A striking example of such terms is the detection of hyperfocus in the ventricle of the fetal heart.

Small ultrasound markers of congenital pathology
Ultrasound scanning during pregnancy is carried out three times in each trimester. The most important is the first prenatal screening, on the basis of which chromosomal abnormalities in the fetus can be detected in a timely manner. Gross anatomical defects are the easiest to identify: it is much more difficult when the doctor sees minor defects. Small ultrasound markers of chromosomal abnormalities include:
- Hyperechoic focus in the chambers of the heart (GEF in the ventricles of the fetal heart);
- Vascular cysts;
- Dilated hyperechoic intestine;
- Enlargement of the renal pelvis;
- Shortening of the limb bones (femur or humerus);
- Thickening of the neck fold;
- Ventriculomegaly (enlargement of brain cavities).
None of these signs can indicate the presence of congenital anomalies, but the ultrasound diagnostic doctor cannot guarantee the absence of developmental defects. GEF in the ventricles of the fetal heart is a risk factor for the possible development of pathology and a reason for careful assessment of the intrauterine growth and development of the baby.
Diagnosis of the problem
If GEF is detected, the specialist refers the pregnant woman to amniocentesis and cordocentesis. Additionally, 3D fetal ultrasound, echo, cardiotocography and Doppler ultrasound are performed.
The most effective diagnostic methods:
- Blood test to detect abnormal chromosomes.
- Fetoscopy allows you to identify the pathological development of a child as a result of genetic disorders. The method is an examination of the amniotic space using a tube inserted through the uterine wall of a pregnant woman. The use of fetoscopy is justified if other diagnostic methods have already been used and have not yielded results. Fetoscopy is considered a dangerous method and is therefore used in extreme cases. There is a possible risk of premature birth.
- Placentocentesis (biopsy) is used to obtain the material required to study the cellular composition of the placenta. The method allows you to study the genes of the fetus and confirm or refute the presence of genetic diseases.
- Amniocentesis is a method that allows you to examine amniotic fluid through a puncture in the abdominal wall of a pregnant woman. Provides biochemical, immune and hormonal indicators to assess the risk of genetic disorders.
Greatest danger
In rare cases, a hyperechoic focus may persist after birth. In such a situation, blood pressure in the left atrium increases, due to which an insufficient amount of physiological fluid enters the right atrium. Among the consequences of this pathology, oxygen starvation of internal organs is noted. If the diagnosis is not made in a timely manner, even the death of the fetus from hypoxia – oxygen starvation – is possible.
A child born with this pathology may experience the following symptoms during the first years of life:

- Increased fatigue, which is expressed in drowsiness and reluctance to play for a long time.
- Apathy.
- Attacks of acute pain in the heart area, which arise due to disturbances in its functioning.
- Shortness of breath, especially during light physical exertion, such as climbing stairs or active games.
- Cardiopalmus. This symptom can be either constant or periodic.
- Swelling of the limbs, which is most noticeable in the evening, as well as in the morning if the child drank water at night.
- Paleness of the skin, sometimes cyanosis.
- Cool hands even in hot weather.
In addition, attacks of tachycardia and rapid breathing are sometimes observed. In such cases, it is necessary to register the child with a cardiologist. He will prescribe appropriate treatment that will help relieve symptoms in a sick child. By the age of 4, the child will either “outgrow” the disease on his own, or may require medication or surgery.
RESULTS
RESULTS ASSURANCE ASSURANCE ASSURANCE. RESULTS registry ° slop RESEARCH RESEARCH ÑедÑеÑдие. OPTIONAL RESEARCH RESULTS оÑганов. RESULTS ¾Ð¶Ð½Ð° даже ÑмеÑÑÑ Ð¿Ð»Ð¾Ð´Ð° Ð¾Ñ Ð³Ð¸Ð¿Ð¾ÐºÑии — киÑÐ»Ð¾Ñ Ð¾Ð´ ного голоданиÑ.
Ребенок, ÑожденнÑй Ñ Ð´Ð°Ð½Ð½Ð¾Ð¹ паологиеР¹, ¹ RESULTS:
- RESULTS, RESULTS ливоÑÑи и нежелании игÑаÑÑ Ð´Ð»Ð¸ÑеР»Ñное вÑемÑ.
- RESPONSIBILITY
- RESPONSIBILITY, RESPONSE ROOM ÑабоÑе.
- оÑÑка, оÑобенно пÑи неболÑÑÐ¸Ñ ÑизиÑеÑÐºÐ¸Ñ Ð ½Ð°Ð³ÑзкаÑ, напÑÐ¸Ð¼ÐµÑ Ð¿Ñи поР´Ñеме по леÑÑниÑе, акÑивнÑÑ Ð¸Ð³ÑаÑ.
- RESULTS. RESULTS ак и пеÑиодиÑеÑким.
- RESULTS, RESULTS меÑна в веÑеÑнее вÑемÑ, а Ñакже ÑÑÑом еÑли вÑÐ¿Ð¸Ð»Ð²Ð¾Ð´Ñ Ð½Ð° ноÑÑÑ.
- ROOM оÑÑÑÑ.
- RESULTS.
RESULTS, RESULTS ºÐ°Ñдии и ÑÑаÑенного дÑÑаниÑ. RESULTS RESULTS. RESULTS ¾Ðµ поÑпоÑобÑÑвÑÐµÑ ÑнÑÑÐ¸Ñ ÑимпÑомаѸки Ñ Ð±Ð¾Ð»Ñ Ð½Ð¾Ð³Ð¾ Ñебенка. Ð 4-sound µÐ»Ñно «Ð¿ÐµÑеÑаÑÑеѻ заболева°Ð½Ð¸Ðµ, лР¸Ð±Ð2 µ µ µ µ µ