What parasites are typical for humans and how does infection occur?
Parasitic lung diseases are caused by parasites that enter humans from the environment. Most often, these diseases occur in people who work in animal husbandry. The larvae enter the human body mainly through the nutritional route (through
household items, food, dishes). Among parasitic diseases, the pathogens of which multiply in the stomach and intestines, the most common are ascariasis, toxoplasmosis, cysticercosis, echinococcosis; less often - amebiasis, paragonimiasis, schistosomiasis, trichinosis.
Lung damage occurs through the blood or lymph. In capillaries, alveoli, bronchioles, parasite embryos turn into larvae. As the larva multiplies, it causes inflammation and sometimes allergic reactions, including necrosis and the formation of cysts. The location and size of cysts can be very different: sometimes cysts can occupy a very significant space, even “displacing” an organ. After the death of the parasite, calcification of the shell and the parasite itself occurs.
Parasites usually settle in the human body for a long time, chronically, without causing serious clinical manifestations. Sometimes allergic reactions may occur: skin itching, urticaria, eosinophilia in a blood test. In case of complications, leukocytosis (signs of suppuration, inflammation) and acceleration of the erythrocyte sedimentation rate can be detected in the blood.
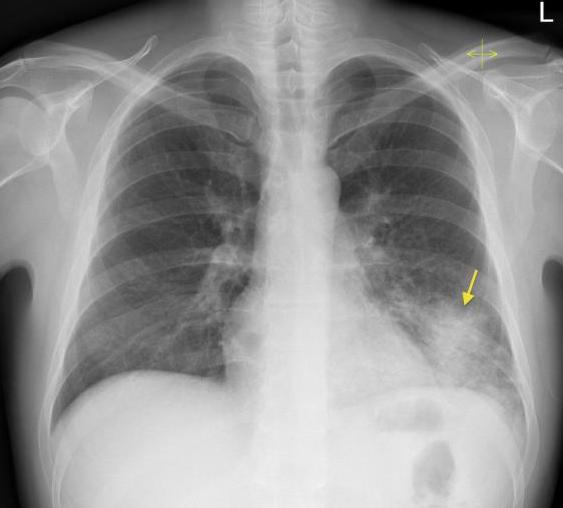
What does coronavirus look like on an X-ray?
COVID-19 attacks the lungs. Fluid accumulates in the pleural cavity around the respiratory organ and it increases in size. The lung tissue becomes scarred, and this makes it difficult for a person to breathe, since part of the organ is destroyed and it is difficult for oxygen to enter the blood.
When X-raying lungs affected by coronavirus infection, darkening is observed in the lower part of the organ (indicated by white spots in the image). The spots are called the “ground glass” symptom. The x-ray shows spots that are caused by the presence of fluid in the lungs.
Pulmonary echinococcosis
The causative agent of echinococcosis is tapeworm cystodes. Getting into the lungs through the blood, the parasite forms cysts there.
There are single-chamber and multi-chamber echinococcosis. When examining the cyst: it has its own membrane, a fibrous capsule is formed around the parasitic cyst, hydatid cysts are filled with liquid content, which can be easily diagnosed using multidetector computed tomography. The parasite may also have daughter cysts. Cysts grow over time, but slowly over several years.
Diagnosis: on X-rays or SCT scans, you can identify an echinococcal cyst, which has clear contours, usually an oval shape, with an average size of about 3-5 cm, sometimes it can reach 15-20 cm, the structure of the cyst remains homogeneous for a long time. If the parasite dies, the capsule shrinks and calcium salts are deposited in it.
Complications : most often there is suppuration of the echinococcal cyst, a breakthrough of pus from the cyst into the bronchi or pleural cavity. Possible compression of the segmental bronchi and disruption of bronchial obstruction with the formation of valvular swelling of the segment, the development of hypoventilation, atelectasis, and the addition of pneumonia.
Perhaps you have questions - ask them to me!
Ground glass sign in the lungs
The “frosted glass” symptom manifests itself in patients against the background of lung damage by the virus. Since the respiratory organ undergoes serious changes, areas of damage appear in it.
The density of lung tissue decreases. Moderately reduced airiness appears in the affected area, the main sign being the visibility of the lung vessels and bronchial walls.
It is difficult to notice this symptom on an x-ray, so an additional computed tomography is required.
Typical signs of frosted glass symptoms:
- the walls and structure of the bronchi are clearly visible;
- darkening is visible;
- the vascular pattern is preserved;
- The transparency of the lung tissue increases.
Reasons for which this symptom occurs:
- pulmonary edema;
- pneumonia caused by viral particles;
- chronic diseases of the lung tissue;
- respiratory distress syndrome;
- systemic connective tissue diseases;
- heart failure in the stage of alveolar pulmonary edema;
- bleeding from the pulmonary vessels.
Cysticercosis of the lungs
The causative agent is the larvae of pork tapeworm. Entering the lungs through the blood, cysticercus larvae can remain viable for a long time, fixing in the interstitial tissue, the cysticercus begins to multiply. Around it in the lungs a fibrous capsule is formed, which is surrounded by lymphocytic infiltration. Multiple thin-walled oval or round bubbles are formed, 1-2 cm in diameter.
When diagnosed on radiographs or multislice computed tomography scans, clearly defined round or oval lesions of a homogeneous structure, about 1 cm in diameter, can be visualized. They don't merge with each other. At first, the adjacent sections of the pulmonary parenchyma are not changed; over time, signs of deformation of the pulmonary pattern may appear; in the case of the development of foci under the pleura, foci of compaction of the costal and interlobar pleura may be observed. After the death of the parasite (2-3 years), calcification of the foci is observed, which begins from the periphery.
Similar calcifications can be detected in the shoulder girdle, liver, and brain.
How does lung damage manifest due to coronavirus?
Typical manifestations of respiratory disorders during coronavirus infection:
- Fluid accumulates in the lungs and gradually occupies an increasing area;
- the walls of blood vessels and blood cells in the lungs are affected;
- darkening of the “frosted glass” type of various sizes is visible, accompanied by compaction of the partitions between the alveoli - bubbles where the capillaries of the organ are enriched with oxygen;
- Scar tissue called “fibrosis” forms in the lungs, resulting in decreased extensibility and elasticity of the tissue.
Lungs' cancer
A terrible disease that can develop silently and unnoticed over years. It's no secret that smokers are often susceptible to it. Therefore, when they start coughing, many o. And so they miss the initial stage of oncology, says Arkady Vertkin.
Symptoms:
- cough that has a long, persistent character;
- hemoptysis;
- hoarseness of voice;
- dyspnea;
- chest pain, often unilateral, aggravated by deep breathing and coughing;
- weight loss and loss of appetite;
- weakness and fatigue.
“In addition, pneumonia of the same localization, occurring repeatedly within a short period of time, may indicate lung cancer,” the specialist emphasizes.

Hidden threat. The tuberculosis epidemic may be worse than the coronavirus Read more
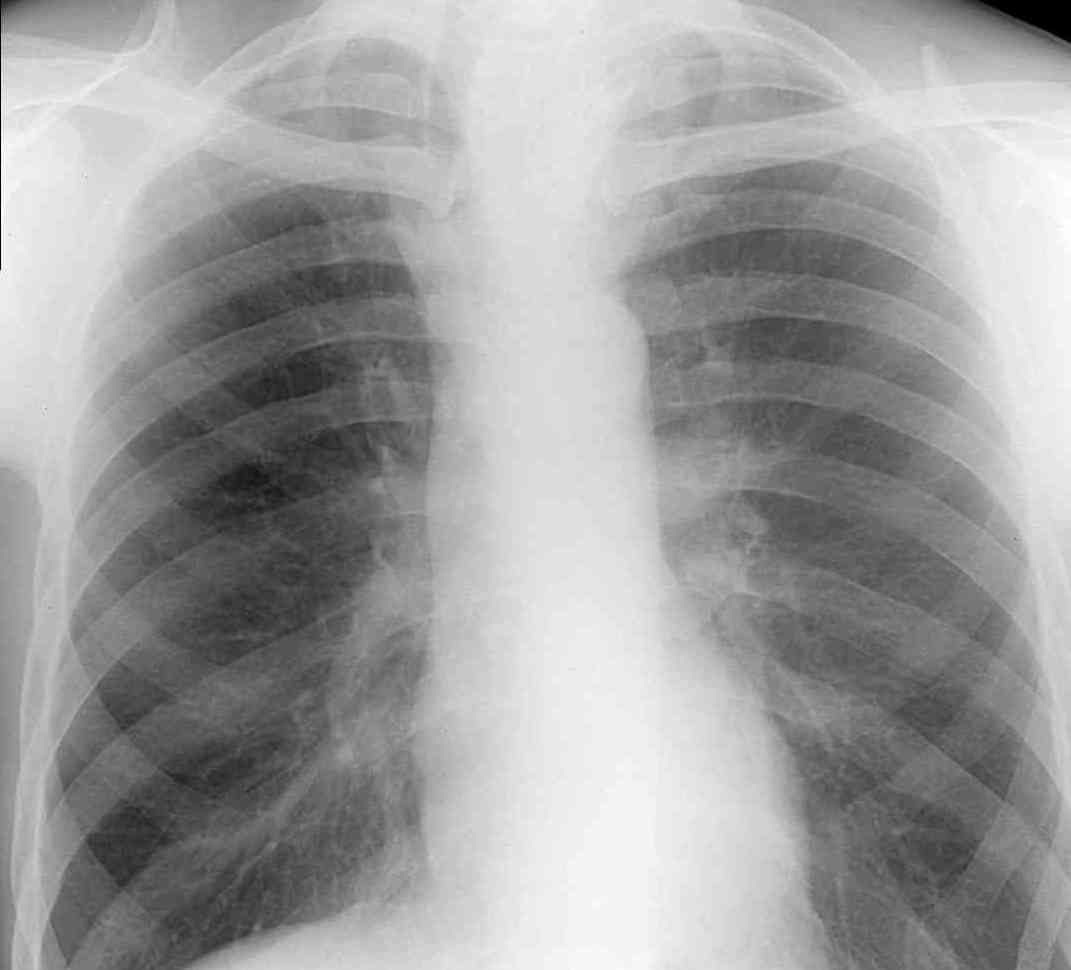
Differences between pneumonia and coronavirus?
Pneumonia is an inflammation of the lungs that is caused by bacteria. Ordinary pneumonia develops when sputum accumulates in the respiratory organs, causing the organ’s ventilation to become impaired and microorganisms to multiply.
With pneumonia, only part of the lungs is affected, but with a coronavirus infection, the entire organ suffers; it fills with fluid and is no longer supplied with oxygen.
Pneumonia, unlike coronavirus, can be cured with antibiotics by destroying the pathogen.
In case of pneumonia, the following signs are visible on an x-ray of the lungs:
- in different parts of the organ there are foci of darkening with uneven contours and a size of 3-12 mm;
- shadows differ in appearance (oval, ring-shaped, round), color intensity - the darker the spot, the stronger the pathological process;
- if the lymph nodes are affected and the blood supply to the organ is impaired, changes in the roots of the lungs may be noticeable; if the pleura is affected, disturbances in the pattern of the domes of the diaphragm are visible.
On an x-ray, pneumonia looks like this:
Pneumonia can develop over several weeks, and the incubation period for COVID-19 is 2-5 days.
Patients with COPD are at risk for coronavirus
Like all people suffering from chronic diseases, patients with COPD are at risk of severe disease and mortality from COVID-19.
According to Philips surveys, the coronavirus pandemic has had a huge impact on the lives of people who suffer from COPD. 56% of patients reported that it became more difficult for them to receive treatment, 58% noted difficulties in controlling symptoms of the disease. 68% of respondents admitted that COVID-19 made them more worried about their illness, and 75% began to look for ways to cope with their illness on their own: giving up bad habits, changing their diet, purchasing air purification systems.

Image: MedPortal
The difference between viral pneumonia and coronavirus?
Viral pneumonia differs from coronavirus in that it has a milder course of the disease. Common causative agents of viral pneumonia are group A and B viruses, adenoviruses and parainfluenza viruses.
As with simple pneumonia, with the viral form of the disease, the same signs of lung damage are visible on x-rays:
- darkening;
- shadows of different shapes and sizes;
- change in the roots of the lungs.
Viral pneumonia looks like this on an x-ray:
Coronavirus differs from viral pneumonia in these ways:
- a severe form of pathology develops quickly, viral pneumonia, even with disappointing prognosis, leaves a chance for recovery;
- coronavirus is accompanied by frequent dry cough, if both lungs are affected, sputum is produced;
- The temperature is difficult to control; with a viral form of pneumonia, the temperature decreases in the morning.
It is impossible to independently distinguish coronavirus from pneumonia.
Coronavirus infection has a devastating effect on the lungs. Therefore, if your health worsens, you need to seek medical help. This approach significantly increases the chances of recovery.
Smoking is a major factor in the development of COPD
Between 80% and 90% of COPD cases develop due to years of smoking. Mortality rates from this disease are highest among smokers; such people develop airway obstruction and shortness of breath more quickly. With every cigarette you smoke, you inhale thousands of chemicals into your lungs, including nicotine, carbon monoxide and tobacco tar. They increase mucus, make it difficult for the lungs to cleanse themselves, cause irritation and inflammation of tissues, which leads to the development of COPD.
There is no cure for this disease, but you can significantly alleviate the symptoms and improve your quality of life, first of all, by quitting smoking. This is the most obvious and annoying recommendation for every smoker, but it is incredibly important, since nothing has such a deadly effect on the respiratory tract as tobacco smoke.
The development of COPD is also influenced by occupational factors - people who work in the mining industry are at risk. Daily inhalation of dust containing cadmium and silicon leads to the development of inflammatory processes in the bronchi and lungs. In rare cases (1% of cases), the development of COPD is due to genetic factors.
Tuberculosis
Many are still confident that tuberculosis is a thing of the past, in history and in Remarque’s novels, says Arkady Vertkin. Unfortunately, it is not. Russia is in third place in terms of the prevalence of this disease.
Another incorrect belief is that tuberculosis is a disease of people of special social status (people without a fixed place of residence, migrants released from prison, alcohol and drug abusers).
“These are indeed risk groups for infection with this disease, but, unfortunately, due to its widespread prevalence, tuberculosis can be contracted regardless of belonging to any social group - just look at the patients in TB departments,” the professor notes.
Symptoms:
- prolonged dry cough;
- constant low-grade fever (increase in temperature from 37.0 °C to 37.9 °C) or an increase in body temperature in the morning with the evening temperature curve returning to normal;
- sweating, especially at night;
- weight loss with preserved appetite;
- weakness, fatigue;
- generalized or limited enlargement of lymph nodes;
- hemoptysis.
Treatment is required; there should be no self-help, only examination and therapy prescribed by a doctor, so as not to aggravate the situation.

What is COPD and how to cope with chronic bronchitis? More details
Bronchitis
Bronchitis is an inflammatory disease of the bronchi. “The symptoms depend on the type of bronchitis: is it acute or chronic, occurs with or without obstruction, etc.,” says Arkady Vertkin. Let us dwell, the specialist notes, on the main clinical symptoms of acute bronchitis lasting less than 3 weeks, which, as a rule, is one of the manifestations of catarrhal respiratory syndrome in acute respiratory viral infection (ARVI)
Symptoms:
- typical symptoms of general intoxication are weakness, malaise, headache;
- fever of varying severity (optional);
- dry cough (boring and paroxysmal), alternating with wet cough;
- greenish and yellowish sputum indicates a bacterial infection, and white or clear mucus indicates its absence;
- possible pain behind the sternum and between the ribs, aggravated by coughing;
- in the presence of bronchial obstruction, shortness of breath with prolonged exhalation and wheezing appears.
We should not forget that symptoms characteristic of pulmonary diseases can also occur with pathologies of other organs and systems, for example, with heart failure and gastroesophageal reflux disease (GERD), the specialist emphasizes.

Flame pump. Why does chronic heart failure develop? More details











