The danger of this disease lies in the fact that it often begins to manifest itself clinically only in the final stages, when effective treatment is no longer possible. This is due to the fact that there are no pain receptors in the lung tissue.
- Risk factors and causes of peripheral lung cancer
- Classification and stages of peripheral cancer
- Clinical picture of peripheral lung cancer
- Diagnosis of peripheral lung cancer
- Treatment of peripheral lung cancer
- Complications and prognosis of peripheral cancer
Risk factors and causes of peripheral lung cancer
Like any oncological process, peripheral cancer can develop under the influence of carcinogenic factors. First of all, these include harmful production conditions. Lung cancer can develop through prolonged contact with various resins, heavy metals, gases and other chemicals used in production.
The risk of developing peripheral lung cancer increases with a genetic predisposition. Bad habits - primarily smoking, as well as environmental pollution - have a detrimental effect on the condition of the respiratory system.
The risk of peripheral cancer increases with age. Concomitant diseases of the respiratory system and endocrine diseases contribute to this. According to statistics, cancer of the right lung is more common (56% of all cases), in its upper lobe.
Classification and stages of peripheral cancer
Staging of peripheral lung cancer (as well as central) depends on the size of the tumor, its growth into healthy tissue, metastasis to regional lymph nodes and nearby organs. The most current and generally accepted classification of cancer is the TNM system, according to which the stage of the disease is determined.
Criterion T is a characteristic of the primary tumor itself. Tx - detection of tumor areas in biomaterial (sputum, washing water from the bronchi), while it is impossible to detect the primary focus of cancer. Then the primary focus was not found. Tis - cancer “in situ” (localized). T1 - the size of the peripheral lesion does not exceed 3 cm, it is surrounded by healthy pulmonary and bronchial tissue without visible signs of growth into the surrounding areas.
T2 - lesion with the following signs (at least 1):
- The tumor exceeds 3 cm in diameter.
- Tumor growth into one of the two main bronchi, and its size is not of primary importance.
- Cancer growth into the parietal pleura.
- Combination of peripheral cancer with collapse of lung tissue or obstructive bronchopneumonia.
- The pathological process spreads to the hilum of the lung, but the organ is not yet fully involved in the tumor process.
T2a - tumor 3-5 cm in greatest dimension. T2b - tumor diameter 5-7 cm in greatest dimension.
T3 is a tumor process of any size that involves the chest wall, pericardial sac, parietal pleura and mediastinum, diaphragm, or exceeding 7 cm, accompanied by collapse or pneumonia of the entire lung.
T4 is a formation of any size that extends to organs and vessels, mediastinum, esophagus, trachea, spine, etc.
This also includes peripheral processes that occur with the formation of effusion in the pleural cavity, the nature of which was determined cytologically, as well as with the presence of a separate tumor node in the same lobe of the lung.
Criterion N is the presence of affected regional lymph nodes. Nх - insufficient amount of data on the condition of local lymph nodes. N0 - no signs of regional metastases to the lymph nodes. N1 - cancer of local bronchopulmonary and root lymph nodes. N2 - metastases in the lymph nodes of the mediastinum and bifurcation (separation) of the trachea. N3 - spread of cancer to the lymph nodes of the adjacent lung, supraclavicular and subclavian regions.
Criterion M - distant metastases:
- M0 - no metastases in organs.
- M1 - there are distant metastases.
All of the above signs are taken into account to determine the stage of peripheral cancer. In total, there are 4 stages of the process, of which 1 is the easiest, and 4 is the most unfavorable.
Peripheral lung cancer includes such forms as disease of the apex of the lung (Pancoast tumor), round, cavitary and pneumonia-like tumor.
Book a consultation 24 hours a day
+7+7+78
Chondroma, lipoma, pulmonary fibroma: treatment
All benign tumors are subject to surgical treatment, since an increase in their size can lead to severe complications (pulmonary hemorrhage, pulmonary fibrosis, abscess pneumonia, atelectasis, bronchiectasis). Surgical removal of a benign tumor is usually performed by thoracoscopy or endoscopy.
The operation is performed by thoracic surgeons. The extent of surgery will depend on the size of the tumor and the extent of the affected tissue. The earlier the tumor was detected, the less tissue will be removed during surgery and the more favorable the prognosis.
Clinical picture of peripheral lung cancer
The danger of peripheral lung cancer is that in the initial stages it does not manifest itself in any way until it grows into surrounding organs and tissues. By the time clinical signs appear, treating the disease becomes much more difficult.

The first and most characteristic signs of peripheral cancer are shortness of breath and chest discomfort. Shortness of breath increases gradually as more and more lung tissue is involved in the pathological process. In this case, the blood circulation of the organ is disrupted, and atelectasis develops (collapse of the lung or its individual lobes). Many patients do not pay due attention to this symptom, since their disease often begins against the background of existing diseases of the respiratory system.
Painful sensations in the chest occur when cancer grows into the parietal pleura, intrathoracic fascia, etc. With peripheral Pancoast cancer, the tumor spreads into the cervical nerve plexus. The pain can be periodic or constant, and can radiate to the area along the nerves, which is why doctors often confuse it with ordinary intercostal neuralgia.
Cough and hemoptysis occur in the patient already in the later stages of peripheral cancer, which is associated with damage to the small bronchi (starting from the 4th order). Cough causes irritation of the bronchial mucosa. At first it is dry and sparse, but gradually becomes permanent. In the later stages, sputum appears, which consists mainly of mucus and may be mixed with pus. Unfortunately, this symptom is often ignored by patients who perceive it as a worsening of an existing chronic disease. The appearance of bloody streaks in the sputum occurs during the disintegration of lung cancer. In this case, the sputum may contain inclusions of a disintegrating tumor - lumps of mucus, areas of purulent detritus. The intervals between episodes of hemoptysis gradually decrease. Most often, it is this manifestation of cancer that forces the patient to seek medical help.
Fever occurs in half of patients with lung cancer and is caused by a constant inflammatory process in the body. In combination with other symptoms of peripheral cancer, it can be perceived as an exacerbation of bronchitis or pneumonia, however, antibacterial treatment gives an unstable and short-lived effect.
Diagnosis of peripheral lung cancer
The disease can be detected using the following studies:
- X-ray of the chest organs.
- CT scan.
- Bronchoscopy with taking material for biopsy. For peripheral cancer, this method may not be informative.
- Cytological examination of sputum.
- Controlled transthoracic puncture.
Based on radiological signs alone, the diagnosis of peripheral cancer cannot be excluded or confirmed. A survey radiograph is taken in frontal and lateral projections, as well as a targeted radiograph. In 80% of cases, it is possible to detect a focal lung shadow of varying density, which can grow into surrounding organs and the chest wall.
The most informative diagnostic method at the preoperative stage is bronchoscopy, which allows, by inserting a special instrument - a bronchoscope into the lumen of the airways, to examine the tumor in detail and take a biopsy. The round or spherical form of cancer looks like a node with a relatively uniform structure, but unclear contours due to the tendency to grow into surrounding tissues. This is the only method that allows you to prove the diagnosis at the preoperative stage, however, in the case of peripheral lung cancer, it may be difficult to obtain material for research. The pneumonia-like form has the appearance of an infiltrative focal shadow, the structure of which is heterogeneous and the contours are blurred. When decay occurs, a cavity may form inside the tumor.

A special form of cancer is Pancoast tumor. This is a type of peripheral tumor of the apex of the lung, when nearby structures (sympathetic trunk, subclavian vessels and brachial plexus) are often involved in the pathological process.
One of the informative diagnostic methods is a computed tomogram of the chest, which can not only clearly study the tumor itself, but also exclude or confirm metastasis. A computed tomogram can reveal the radiance of the contour, typical for peripheral cancer, a “path” from the tumor to the root of the lung, which is due to the characteristics of the peribronchial and perivascular growth of the pathological focus.
Intrabronchial tumors
Adenoma, cylindroma, carcinoid, hamartoma, papilloma. Most often, these tumors are located in the large bronchi. Their development is accompanied by the appearance of a polypoid node of a round or oval shape. Such a node continues to grow inside the bronchus, into the thickness of its wall.
Benign tumors can degenerate (malignize) into malignant ones.
External manifestations occur only when the tumor blocks the lumen of the bronchus and causes hypoventilation of a large area of the lung. Against this background, hemoptysis, atelectasis, and pneumonia may occur.
Diagnosis : X-rays can reveal varying degrees of bronchial obstruction, hypoventilation, varying degrees of bloating, and infiltration of the pulmonary parenchyma. When performing spiral computed tomography, it is possible to determine in detail the location of the tumor, the relationship between the tumor and the bronchial lumen, determine whether the neighboring bronchi are affected, and identify in detail the changes that have occurred in the lung tissue.
Treatment of peripheral lung cancer
The exact treatment regimen for cancer is always selected individually and depends on the stage of the process, histological type and characteristics of tumor growth. Often, schemes involve a combination of several techniques, which can increase efficiency and improve prognosis.
Treatment of peripheral lung cancer by stage is as follows:
- Patients with stages 1-2 of the disease can be cured by radical surgery.
- Some patients with stage 2 disease are prescribed antitumor drug therapy.
- Patients with the third stage can receive three-component treatment - chemotherapy and radiation therapy, as well as surgery.
- Some patients with stage 3, in whom the oncological process has spread to the nodes of the mediastinum, adjacent lung and supraclavicular region, and patients with stage 4 are considered inoperable and receive palliative therapy.
Today, targeted therapy is gaining popularity in the treatment of cancer pathology, which specifically affects tumor cells, slowing their growth and development. In this case, molecular genetic testing must be performed first.
Complications and prognosis of peripheral cancer
Complications of peripheral lung cancer can be associated both with the tumor process itself and with the treatment already performed. It can be:
- Damage to organs (brain, spinal cord, liver) by metastases with disruption of their function.
- Purulent melting of the tumor focus with the formation of a lung abscess, which can break into the bronchus and into the pleural cavity, mediastinum, etc.
- Sepsis (so-called blood poisoning).
- Bleeding from a disintegrating tumor.
- Associated with the operation, failure of the bronchial stump, bronchopleural fistulas, etc.
Unfortunately, due to the mild clinical picture and late referral to specialists, the prognosis for this form of cancer is often unfavorable. The five-year survival rate of patients even after radical treatment is no more than 30%. Prevention of peripheral cancer includes giving up bad habits, optimizing working conditions, and timely detection and treatment of inflammatory diseases of the respiratory system.
| More information about lung cancer treatment at Euroonco: | |
| Lung cancer treatment | |
| Oncologist consultation | from 5100 rub. |
| Emergency oncology care | from 11000 rub. |
| Chemotherapy appointment | 6900 rub. |
| Radiologist consultation | 10500 rub. |
Book a consultation 24 hours a day
+7+7+78
Material and methods
The work is based on the results of examination and treatment of 110 patients with pathological formations of small diameter lungs who were in the Faculty Surgery Clinic named after. N.N. Burdenko from 1997 to 2013. There were 63 men, 47 women. The age of the patients ranged from 19-74 years.
In all patients, an X-ray examination, including computed tomography, revealed for the first time focal formations in the lungs ranging in size from 0.5 to 2 cm. All patients underwent operations to remove sections of lung tissue with a tumor from various approaches: 44 video-assisted thoracoscopic lung resections, 43 mini-thoracotomies with video support, 23 minithoracotomies. The final diagnosis was formulated after a planned histological examination of the removed pathological lung formation. There were no deaths.
All patients were divided into groups depending on the size of the focal formation: group 1 (TLC diameter 0.5-1; Fig. 1) consisted of 9 men and 14 women, group 2 (TLC diameter 1-2 cm; Fig. 1). 2) - 30 men and 13 women, group 3 (multiple AOLs; Fig. 3) - 27 men and 17 women.

Rice. 1. CT scan of the chest of a patient of group 1
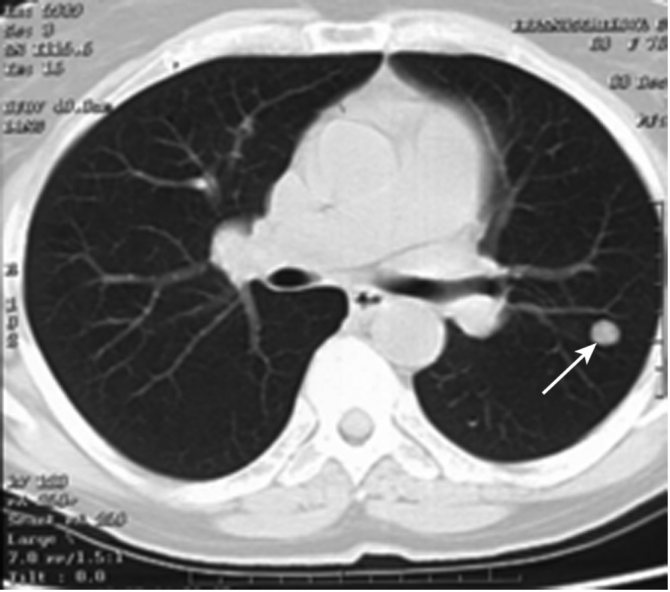
Rice. 2. CT scan of the chest of a patient of group 2.

Rice. 3. CT scan of the chest of a patient of the 3rd group.










