Pneumonia is an infectious disease that affects one or more segments of lung tissue through an inflammatory process. It is transmitted by airborne droplets, and can also be a consequence of other inflammatory processes of the respiratory system. Pneumonia is a common disease that, if untimely or poorly treated, can lead to more serious inflammation or even death.
If you notice several of the listed symptoms, you should immediately consult a doctor, as a quick start of therapy will relieve complications and ensure short-term recovery. Pulmonologists at the Yusupov Hospital, based on their vast experience and knowledge, will be able to accurately determine the stage and form of pneumonia, as well as prescribe treatment that is individually suitable for each patient.
Symptoms and signs
During the first 48 hours, the pneumonia pathogen may manifest itself as a common cold or flu. It is important to pay attention to each individual symptom and consult a doctor in time. Primary symptoms of pneumonia include:
- elevated temperature that lasts 2-3 days (up to 40 degrees);
- swelling of the nose, cyanosis (blueness of the wings of the nose);
- pale skin, swelling;
- pain in the chest, trachea, throat;
- chills;
- cough (dry, wet, paroxysmal, with mucous sputum, purulent secretion, with wheezing);
- shortness of breath, rapid heartbeat;
- general weakness and drowsiness.
There are the following factors that influence the development and progression of pneumonia:
- respiratory diseases: bronchitis, sinusitis, laryngitis, tonsillitis, tracheitis, diabetes mellitus, cancer, AIDS, caries, diseases of the cardiovascular system;
- vitamin deficiency (seasonal or chronic);
- hypothermia, overheating;
- stressful situations;
- bad habits (especially smoking and excessive alcohol consumption);
- recent surgical intervention;
- age under 5 years and after 65;
- lack of regular physical activity;
- being in poorly ventilated areas;
- contact with infected people;
- being in public places during an epidemic;
- taking medications that weaken the immune system;
- poor hygiene, infrequent hand washing.
Diagnosis of pneumonia
- Complete blood count: increased number of neutrophil leukocytes, shift of the leukocyte formula to the left, toxic granularity of neutrophils, absence of eosinophils, increased erythrocyte sedimentation rate.
- General urine analysis: the appearance of protein, urobilin and casts.
- X-ray of the lungs: more often than not, unilateral infiltration of the lung tissue of a focal, segmental, confluent nature.
- Sputum examination: bacterioscopy of a Gram-stained smear makes it possible, in the first hours of a patient’s stay in a medical institution, to distinguish gram-positive microflora from gram-negative ones and determine the morphology of some respiratory pathogens.
- Immunological methods: identification and determination of the degree of activity of chlamydial, mycoplasma and legionella infections; antigens and specific antibodies in the biological environments of the body.
Indications for inpatient treatment:
- Age over 70 years.
- The presence of concomitant chronic pathology: chronic obstructive pulmonary disease, congestive heart failure, chronic hepatitis and nephritis, diabetes mellitus, drug and alcohol addiction, substance abuse, immunodeficiency states.
- Low effectiveness of outpatient treatment for 3 days.
- Various forms of impairment of consciousness.
- Respiratory movements with a frequency of more than 30 per minute.
- A sharp drop in blood pressure, heart rhythm disturbances.
- Damage to several lobes of the lungs.
- The appearance of exudate in the pleural cavity.
- Decrease in the level of leukocytes to 20,000 in 1 µl.
- Decrease in hemoglobin level to 7 mmol/l.
- Social indications.
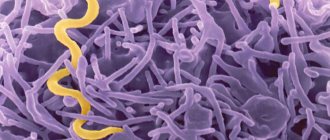
Pathogens of pneumonia
The causative agents of pneumonia completely influence the course of the disease. Each infectious agent gives a different clinical picture. Based on the type of pathogen, pneumonia is divided into several types:
- viral pneumonia (rhinoviruses, adenoviruses, influenza viruses, parainfluenza, measles, rubella, whooping cough, cytomegalovirus infection);
- bacterial pneumonia (staphylococci, pneumococci, chlamydia, streptococci, Haemophilus influenzae, mycoplasma pneumoniae);
- fungal pneumonia (pathogens are fungi of the genus Candida, Pneumocystis, Aspergillus);
- helminth pneumonia (caused by parasites);
- mixed (when the pathogens are several pathogenic agents at once).
Classification according to clinical signs
There are several main types of pneumonia. Each of them differs not only in pathogens, but also in the clinical picture. The main types of pneumonia include:
- typical pneumonia, which is characterized by a sharp rise in temperature, severe cough with copious sputum, pain and a feeling of tightness in the chest area. Diagnosis of this type of disease shows wheezing in the pleural cavity, bronchophony, darkening on the x-ray and hard, labored breathing;
- atypical pneumonia. Symptoms may be mild or completely absent. The patient may complain of a mild dry cough, sore and sore throat, headaches or dizziness, myalgia, general weakness and malaise. X-ray or fluorography may show mild signs of pneumonia in the image. This type of pneumonia can very often be confused with another ailment and the wrong treatment can be started. Pulmonologists at the Yusupov Hospital, using their professional skills, will make the correct diagnosis and, referring to all the tests completed, will prescribe a competent decision that will not entail any consequences;
- lobar pneumonia (pleuropneumonia). One of the most severe types of the disease. It is characterized by a sharp increase in temperature up to 40 degrees, shortness of breath, severe cough with greenish sputum, or mixed with pus or blood clots, as well as severe pain in the area of the affected area of the lung. The affected area may even occupy both lobes of the lung, depending on the rate of spread of the infection. Analysis for pneumonia and timely treatment in this case is very important, since otherwise the disease can develop into a lung abscess or cardiopulmonary failure.
Pneumonia
Cold
Fungus
9177 January 13
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Pneumonia: causes, symptoms, diagnosis and treatment methods.
Pneumonia is an acute infectious disease predominantly of bacterial origin, which is characterized by damage to the lung tissue and leads to impaired respiratory function. The disease has typical clinical manifestations.
Pneumonia has been known for a long time, but its successful treatment became possible after the discovery of microorganisms (bacteria, viruses, fungi), the fact of their participation in the development of inflammation in the lungs and the development of specific antimicrobial drugs - antibiotics. Before this, pneumonia was a common cause of death in people of all ages.
Causes
The primary cause of pneumonia is an infectious pathogen.
Most often these are bacteria, less often – viruses and parasitic fungi. Their penetration into the lungs is accompanied by activation of the immune system and the development of an inflammatory response, the main goal of which is to destroy the pathogen.
However, during the body’s fight against infection, damage to its own tissues occurs, including pulmonary tissue, which underlies the occurrence of pneumonia. The release of specific biologically active substances, as well as the entry into the blood of waste products of microorganisms, determines the development of a systemic reaction of the body to an infectious pathogen. Therefore, in case of pneumonia, especially severe, disruption of the functioning of other organs and systems plays a significant role.
Classification
There are several criteria based on which pneumonia is classified.
Thus, depending on the nature of the pathogen, bacterial, fungal, parasitic, viral pneumonia and pneumonia of mixed etiology are distinguished.
The inflammatory process can be unilateral, involving only one lung, or bilateral.
Depending on the volume of the lesion in each lung, pneumonia is classified into focal, segmental, lobar, etc.
Pneumonia is not a mild disease; the prognosis is always serious. However, there is a group of severe pneumonias that require intensive treatment and medical supervision with mandatory hospitalization.
In the medical environment, pneumonia is divided into community-acquired and hospital-acquired.
This gradation is based on the moment of infection: outside the hospital or in the hospital. This indicator is integral, reflecting the possible spectrum of infectious agents (more aggressive pathogens, perhaps even resistant to a number of antibacterial agents, are more common in hospitals), their sensitivity and resistance to the main groups of antimicrobial drugs, the person’s previous health status and the general prognosis of the disease.
Symptoms of pneumonia
Manifestations of pneumonia can be divided into general and local. The first will include symptoms of intoxication. They indicate the presence of an infectious process in the body in general, and not specifically in the lung tissue.
Fever, general weakness, fatigue, loss of appetite, headache, drowsiness - these symptoms are characteristic of a variety of diseases, and not only those of infectious origin.
Therefore, in the diagnosis of pneumonia, the most important characteristic signs from the respiratory system are: cough, shortness of breath, and the appearance of pain in the chest area.
During the examination, the doctor determines a change in the density of the lung tissue during percussion (tapping a finger on the patient’s chest), as well as the presence of fluid accumulation in the lungs during auscultation: wheezing and crepitation are heard (a type of sound especially characteristic of pneumonia). In severe cases, respiratory dysfunction is so severe that the patient's skin, especially around the mouth, becomes bluish due to insufficient oxygen saturation of the blood. Due to hypoxia (oxygen starvation) of the brain, impaired consciousness may occur.
Pulse oximetry, a non-invasive way to assess the degree of oxygen saturation in the blood using a small device placed on the patient’s finger or earlobe, has quite widely entered into the practice of a doctor.
Diagnostics
Diagnosis of pneumonia begins with identifying complaints. Patients usually note a sudden onset of cough and increased body temperature. However, these symptoms are characteristic of many diseases, and not just pathologies of the respiratory system.
Finding out the medical history allows you to establish predisposing factors, possible conditions of infection and suspect the causative agent of the infection.
It is important to find out whether the patient has concomitant diseases, the fact that he is receiving medications that reduce the body’s natural resistance to infections, as well as bad habits, especially smoking.
The gold standard for diagnosing pneumonia is a chest x-ray in two projections.
Analyzes
Quick identification of the causative agent of pneumonia will speed up the recovery process, since it will be easier for the doctor to navigate what therapy should be aimed at (antifungal, antiviral, etc.). To determine the causative agent of pneumonia, it is necessary to undergo a full examination, including the following tests:
- chest x-ray;
- fluorography;
- computed tomography;
- blood and urine tests.
Fluorography is rather a preventive method, since x-rays are considered to be a more informative method. Certain types of pneumonia may be difficult to read on fluorography. Moreover, the radiation dose received with fluorography is higher than with x-rays.
General analysis
Blood in pneumonia can be characterized by the following indicators:
- In pneumonia, leukocytes are increased and leukocytosis occurs. Normally, the content of white blood cells in the blood of a healthy adult varies from 4 to 9 G/l. However, with pneumonia, this figure can increase to 40-60 G/l, as the body begins to resist the infection;
- red blood cells are within normal limits or slightly decreased. A significant reduction in the number of red blood cells can only occur if the disease is severe as a result of dehydration;
- decrease in the number of leukocytes (leukopenia) – characteristic of viral pneumonia;
- if the leukocyte formula shows a reduced number of lymphocytes and an increased number of neutrophils, this in most cases indicates the presence of viral pneumonia;
- decrease in the percentage of monocytes, basophils and eosinophils;
- ESR in pneumonia (or sedimentation reaction, ESR) exceeds normal values. The normal ESR for women is 2-15 mm/h, for men 1-8 mm/h, while with pneumonia this figure in both sexes can exceed 30 mm/h;
- platelets are usually within normal limits.
Sources and reference materials
Click on the required document to download:
| # | File | file size |
| 1 | Laboratory and instrumental standards | 145 KB |
| 2 | Laboratory standards (blood, biochemical, feces, respiratory function, etc.) | 218 KB |
| 3 | Diagnosis of respiratory diseases. Hams | 9 MB |
| 4 | Diagnosis and treatment of community-acquired pneumonia. Infectious Diseases Society of America Guidelines | 833 KB |
| 5 | Diagnostic algorithms and protocols for providing medical care for pneumonia | 3 MB |
| 6 | Lung studies and major syndromes | 199 KB |
Blood counts during illness and during recovery
Immediately after the patient’s recovery, the UAC indicators improve, but do not return to normal completely. An inflammatory process of this nature does not go away quickly, so there is no need to worry about changes in the blood flow after recovery, since they will persist for quite a long time until the immune system is completely restored. White blood cells reach normal levels, but the erythrocyte sedimentation rate may remain at the same high level. A characteristic feature of the normal healing process is a slight increase in the number of eosinophils. If they are reduced or completely disappeared, this most likely indicates the development of complications.
It is very important to start treating pneumonia on time to avoid the development of more serious secondary pathologies. Timely and high-quality treatment determines the speed of recovery and the ease of the disease itself. The competence of the doctors at the Yusupov Hospital has been repeatedly confirmed by international certificates and the trust of our patients. The therapy clinic is equipped with all the necessary medical equipment, thanks to which specialists are able to establish the most accurate diagnosis and select effective treatment tactics for pneumonia. Appointments can be made by calling the clinic. You can contact the coordinating doctor through the feedback form on our website.