Functions of lipase in the body
The body is not able to independently digest the food consumed by a person. For this you need helpers. The digestion process begins in the mouth, where saliva is produced. When thoroughly chewed, slow carbohydrates begin to break down into fast carbohydrates. Which promotes further digestion. Next, the food enters the stomach, then into the intestines, where complex chemical and physical processes begin. After all, food must not only be digested, but also useful elements must be isolated and absorbed. Therefore, it is recommended to eat daily the foods listed in the article: TOP 12 healthiest foods.
When a chewed lump of food enters the stomach, gastric juice, which contains a huge amount of various enzymes, comes into play. Next, the food is processed into the intestines. At this moment, the pancreas receives a signal and begins to actively produce pancreatic juice. It is at this stage that fats are broken down into their simplest forms.
Interesting! Did you know that the human small intestine consists of three sections - the duodenum, jejunum and ileum. Its length is 6.7 m.
Colipase and bile acids work together with lipase They melt sparingly soluble fats and oils of various origins (vegetable, milk, animal fat). After this, the final products are easily absorbed into the body. If the process is disrupted, the necessary vitamins and microelements are not absorbed. Don't ignore winter vitamin and mineral deficiencies.
Functions of lipase :
- fat fractionation;
- processing of fat-soluble vitamins:
- vitamin A (retinol, retinal, beta-carotene);
- vitamin D3;
- vitamin E;
- vitamin K.
- melts fats;
- participates in energy exchanges;
- regulates blood lipid levels;
- normalizes metabolism.
Lipase the intestine as the inactive enzyme prolipase. It is activated by colipase and bile acid.
Carrying out analysis
To conduct the study, venous blood is taken. There are a number of dietary restrictions before taking the test. So you need to exclude the following foods within 12 hours before: fatty, spicy, spicy, and even better, if you abstain from them for 4 days. Like most other blood tests, it must be taken on an empty stomach and in the morning, preferably before noon. If the patient is scheduled for an x-ray on the same day, you may want to consider rescheduling the day for the blood draw. In emergency cases, when the patient’s life is at stake, the analysis is carried out without specified conditions.
Article on the topic:
Can I drink water before taking a blood test?
In modern medicine, two methods are accepted for determining the amount of enzyme in the blood: immunochemical and, the most popular and fastest, enzymatic.
Application of lipase
Enlarge image
Lipase is one of the active components of enzyme preparations. Used to normalize digestive processes and regulate the functioning of the pancreas. Most often, lipase of animal origin is used in such preparations:
- veal;
- goat;
- lamb
Some preparations contain lipase of plant origin.
Lipase is most often used in combination with other enzymes in replacement therapy. Indeed, if there is a digestive disorder, the patient not only complains of pain and poor health, but also does not receive all the necessary substances from the food they eat. And fats in the diet, broken down by lipase , are the main source of energy, vitamins A, D, E, K, and a stimulator of brain activity.
So why does the body of many people not burn excess fat on its own, but store it? The whole reason is sugars (carbohydrates). When consuming “sweets,” the body begins to actively produce insulin, which forms a certain barrier that prevents the production of lipase .
Reasons for deviations from the norms
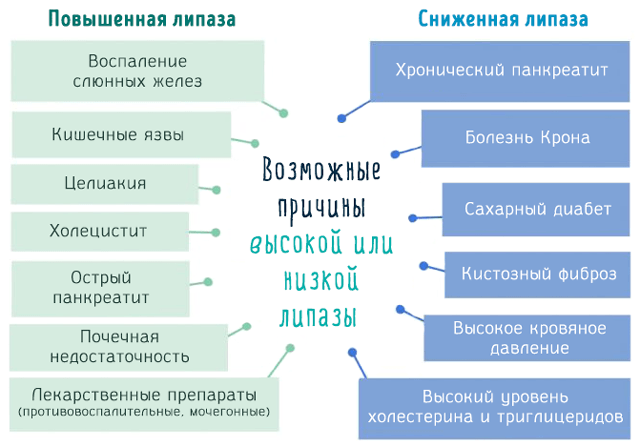
An important diagnostic indicator is an increase in the amount of lipase in the blood plasma. An increase in this indicator indicates that the following pathological processes occur in the pancreas:
- Destruction of gland cells, as a result of which a high amount of lipase, as well as other enzymes, is released into the blood;
- Retention of pancreatic juice in the ducts, resulting from stones, tumors of the duct itself or the duodenum.
But most often these processes occur either simultaneously or as a consequence of one another.
Low levels of the enzyme indicate the development of conditions such as:
- cystic fibrosis;
- stomach ulcer;
- cancerous formations;
- peritonitis;
- chronic course of pancreatitis;
- hyperlipidemia;
- diabetes;
- Crohn's disease;
- high blood pressure.
Lipase: effect on the body
When fats (animal or vegetable origin) enter the mouth of an adult with food, they do not undergo changes. And they come out of the stomach in almost the same form. Although the gastric juice contains lipase , its concentration is quite low. And the pH for enzyme activation is far from normal (5.5 - 7.5). It does not break down fats in the stomach, but greatly simplifies their further digestion in the intestines.
It's a different matter for infants. In response to sucking and swallowing movements, lipase , which helps quickly deal with the lipids contained in milk.
When chyme (semi-digested food) enters the small intestine, gastric acid is neutralized, after which the final fractionation of fat begins.
Some vegetables and fruits contain lipase . These foods are easier to digest and even help get rid of “bad fat” in the body. These include:
- avocado (avocado oil and fresh fruits);
- flax seeds;
- pumpkin seeds;
- nuts.
All these foods should be consumed raw.
Lipase release
The pancreas secretes a certain amount of enzymes, including lipase , necessary to break down a certain amount of food. If there are any malfunctions in the established mechanism (excessively large portions of food, too fatty foods, diseases associated with the secretion of secretions), it turns out to be unprepared for a corresponding change in the level of produced enzymes. And the person faces a number of unpleasant symptoms. Foods that should be excluded from your diet: TOP 12 most harmful foods.
There are two points of view:
- the pancreas produces a lipase , which subsequently activates the enzyme;
- lipase is activated by salts of conjugated bile acids.
After splitting, the fat is quickly absorbed. Literally after 10-30 minutes, drops of absorbed fat are found in the intestinal epithelium.
Systematic disturbances in the digestive processes can also manifest themselves externally:
- dry skin;
- acne;
- brittle nails;
- dermatitis;
- obesity.
Due to a lack of essential vitamins and microelements, hair also grows poorly, becomes brittle, and loses its shine.
Symptoms of lipase deficiency and excess
When should you be wary and consult a doctor? If the consistency of the stool changed to liquid, abdominal cramps appeared, appetite disappeared and weight began to disappear, periodic feelings of nausea, vomiting, flatulence, general weakness and low physical activity appeared. In addition, sometimes your body temperature may rise slightly.
All these symptoms indicate both an excess and a lack of lipase. The only thing is that body hyperthermia most likely indicates an excess of the enzyme level.
Elevated lipase

Digestive enzyme is produced by the pancreas. It is then secreted into the duodenum (the initial part of the small intestine) and the terminal parts of the small intestine, where the bonds in glyceride molecules are broken down. Pancreatic lipase the bloodstream in small quantities and does not in any way affect the human body or well-being. But with some diseases, the level of lipase in the blood may increase. And the release of the enzyme outside the intestines has a destructive effect on the body.
Interesting! The duodenum is shaped like a horseshoe. And its length is 12 diameters of the fingers.
lipase levels in the blood to diagnose certain diseases back in the 30s of the last century. The presence of an increased concentration of lipase in the blood is an SOS signal from the body, which may indicate the following pathological conditions:
- neoplasms in the pancreas;
- biliary dyskinesia;
- acute or chronic inflammation of the peritoneum;
- necrosis of the intestinal wall;
- acute inflammatory disease of the gallbladder;
- biliary colic, intrahepatic cholestasis;
- diabetes mellitus, excess weight, gout and other diseases associated with metabolic disorders in the body;
- acute inflammation of the pancreas;
- inflammatory bowel diseases;
- destruction of adipose tissue: fractures of large bones, soft tissue ruptures, postoperative period;
- mammary cancer.
Also, an increase in the level of enzyme in the blood is observed when taking certain drugs:
- captopril;
- corticosteroids;
- oral contraceptives;
- furosemide;
- ibuprofen;
- narcotic painkillers;
- heparin.
A significant increase in the enzyme in the blood is observed in alcoholism. lipase levels between men and women. In children under two months of age, pancreatic enzyme activity is reduced. It increases only towards the end of the first year of life.
Indications for lipase testing
This laboratory test is prescribed when there are suspicions of pancreatic dysfunction:
- severe abdominal pain, often girdling;
- body hyperthermia;
- vomit.
In addition, the value of lipase in blood or urine samples may indicate the progress of the following diseases:
- cancerous formations;
- cholelithiasis, bile duct dyskinesia, cholecystitis, cholangitis;
- pathological changes in the pancreatic parenchyma: pancreatitis;
- piggy;
- acute cholecystitis;
- chronic liver diseases;
- diabetic ketoacidosis;
- obstruction of the small intestine;
- impairment of all kidney functions;
- mammary cancer.
Analysis for this enzyme in 98% of cases gives an accurate answer about the presence of pancreatic diseases. If a diagnosis has already been made, the study will show how effective the treatment is.
Decreased lipase

Not only an increased level of lipase in the blood serum can indicate pathological processes in the body. A reduced concentration of the enzyme warns of irreversible damage to pancreatic cells. Enzyme deficiency leads to malabsorption and is manifested by abdominal pain and fatty stools, because fat-soluble vitamins are not fractionated and are poorly absorbed in the intestines.
The most common causes of low lipase in men and women:
- gastrointestinal cancer (except pancreatic carcinoma);
- poor diet (excess fatty foods) and hereditary hyperlipidemia;
- cystic fibrosis;
- postoperative period after pancreatectomy;
- exocrine insufficiency.
In infancy, low levels of the enzyme are considered normal in children.
Normal blood lipase
- from 0 days: 0 – 70 units.
- from 1 years: 0 - 100 units.
- from 10 years: 0 – 130 units.
- from 18 years old: 0 – 190 units.
For a more accurate diagnosis, the lipase is often done with the amylase test. This helps differentiate between acute and chronic pancreatitis if there is any doubt.
Lysosomal acid lipase deficiency: clinical and pathological characteristics
Lysosomal acid lipase deficiency (LALD) belongs to a group of rare lipid storage diseases inherited in an autosomal recessive manner. The disease has a progressive course, which is based on a violation of the metabolism of cholesterol esters and triglycerides from low-density lipoproteins as a result of deficiency or complete absence of the enzyme lysosomal acid lipase. DLCL has two clinical variants: Wolman disease (infantile form) and cholesteryl ester storage disease. Russia has accumulated experience in diagnosing and managing patients with DLCL. The article presents current literature data, and also presents for the first time the results of domestic studies of the morphological signs of DLCL in children, carried out under the guidance of Professor E.L. Tumanova.
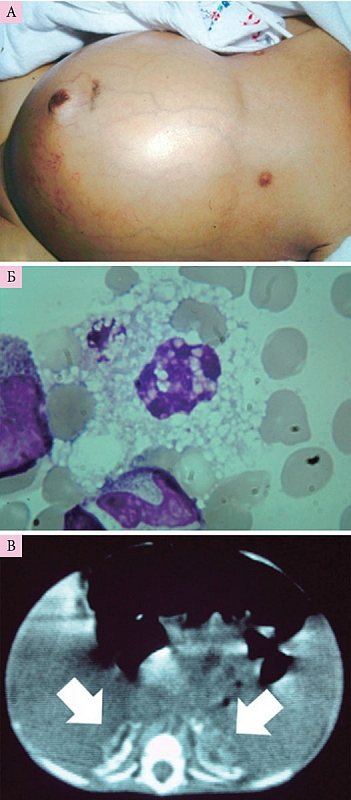
Rice. 1. Clinical signs of Wolman’s disease: large abdomen (A), foam cells in the bone marrow punctate (B), large adrenal glands with calcifications, according to the results of computed tomography of the abdominal organs (C)
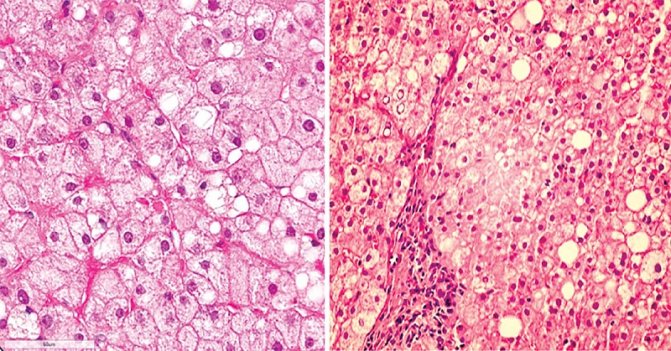
Rice. 2. Microvesicular steatosis, mild infiltration of the portal tract
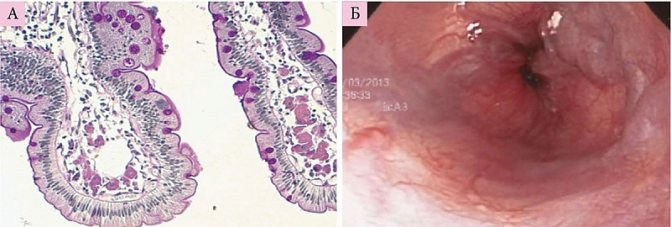
Rice. 3. Histiocytes with ceroid material in the lamina propria of the villi of the duodenal biopsy (A) and varicose veins of the esophagus (B)
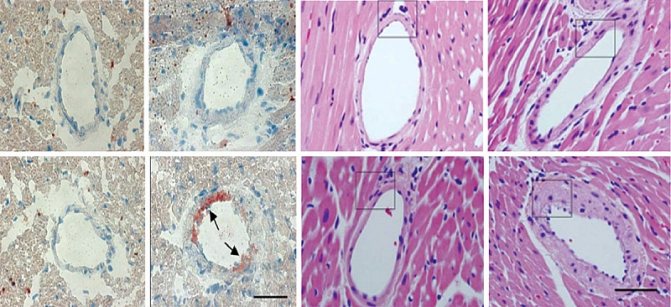
Rice. 4. Changes in arterial walls in cholesteryl ester storage disease
History of the discovery of lipid storage diseases
In 1882, French physician Philippe Gaucher first described a previously unknown disease in a 32-year-old woman with severe splenomegaly and unusual large cells in the spleen. Gaucher disease was the first of the described diseases related to lysosomal storage diseases, and gave impetus to the subsequent study of enzymatic, genetic and molecular disorders in this group. The discovery of Philippe Gaucher made it possible to draw up a phenotypic characteristics of similar diseases and justify enzyme replacement therapy.
To date, over 50 lysosomal storage diseases are known, included in the list of orphan (rare) diseases. The term “orphan diseases” appeared in 1983 in the USA. Orphan diseases have an autosomal recessive type of inheritance, occur with an average frequency of 1/75,000 (the frequency of some orphan diseases is 1/350,000–1/700,000) and have an unfavorable prognosis. The most studied lysosomal lipid storage diseases are Gaucher disease, Niemann–Pick disease, and lysosomal acid lipase deficiency (LALD).
Congenital deficiency of lysosomal acid lipase
DLCL in infants was first described in 1956 by A. Abramov, S. Schorr and M. Wolman. In 1961, M. Wolman, VV Sterk, S. Gatt, M. Frenkel gave a complete clinical description of the disease in three siblings. The disease is named Wolman disease in honor of the neurologist Moshe Wolman (1914–2009). In 1963, a relatively favorable variant of the course of DLCL was described - cholesteryl ester storage disease. In 1969, AD Patrick and BD Lake, and in 1972, JA Burkle, WK Schubert, HR Sloan and DS Fredrickson [1] established the cause of the disease: deficiency of the acid lipase enzyme in lysosomes is caused by a mutation in the LIPA gene, localized on chromosome 10 , locus 10q23.2–23.3 [2]. Congenital DLCL was described in detail in rats in 1990 [3]. In 2015, a drug for enzyme replacement therapy, sebelipase-alpha (Kanuma), was registered, which significantly improved the prognosis of the disease [4–8].
DLCL still remains little studied not only in our country, but also abroad. It is no coincidence that each newly described confirmed case of DLCL is carefully analyzed to clarify the clinical and morphological features of the course in children. Genetic analysis is not leading in the diagnosis of DLCL, since over 40 mutations of the LIPA gene have been described [9]. The main confirmation of the diagnosis is the determination of lysosomal acid lipase activity in dried blood spots.
The importance of the enzyme lysosomal acid lipase
Lysosomal acid lipase is a key enzyme involved in lipid metabolism, catalyzing the hydrolysis of cholesteryl esters and triglycerides from low-density lipoproteins in lysosomes, providing cells with free cholesterol [9, 10]. In turn, free cholesterol is involved in the synthesis of components of cell membranes, steroid hormones and bile acids. It should be noted that, according to its chemical properties, cholesterol is a natural polycyclic lipophilic alcohol and is referred to as cholesterol in the English literature. In Russian literature, the old name (cholesterol), proposed in 1815 by Michel Chevrel, is retained.
Cholesterol constitutes up to 30–40% of the total amount of cell lipids, 60–80% are distributed in the plasma membrane, 0.5–1.0% of cholesterol is included in the structure of the endoplasmic reticulum. In DLCL, cholesterol esters accumulate in various organs and tissues (liver, spleen, intestinal epithelium, lymph nodes, adrenal glands, capillary endothelium, cells of the macrophage-monocyte system), for which high enzyme activity is considered normal.
Clinical variants of DLCL
Lysosomal acid lipase deficiency has two clinical manifestations: Wolman's disease (another name is primary familial xanthomatosis with adrenal involvement and calcification) and cholesteryl ester storage disease.
Wolman's disease, or the infantile form of DLCL, is characterized by an extremely unfavorable prognosis: the manifestation of the disease is noted already in the first month of a child's life, the average life expectancy is 3.7 months [11]. The level of lipase in Wolman's disease is reduced by 200 times or more.
General clinical characteristics of Wolman's disease (Fig. 1):
- increase in abdominal size;
- severe intestinal malabsorption;
- anemia; hepatomegaly; hepatosplenomegaly (79% of children);
- diffuse adrenal calcifications (pathognomonic sign);
- increased levels of serum transaminases;
- progressive hepatic fibrosis and cirrhosis;
- delayed physical development;
- rapidly progressing course of the disease;
- the presence of vomiting, diarrhea, steatorrhea, changes in biochemical blood tests (in 43% of children, the first symptoms occur already in the first month of life);
- poor outcome on average in the first six months of life. In the absence of pathogenetic treatment, all children die by the age of one year. In a study, 67% of children receiving enzyme replacement therapy survived beyond the 12-month mark [12].
In a biochemical analysis of the blood of children with Wolman's disease, elevated levels of alanine aminotransferase (average value - 56.5 U/l) (53.3% of cases), aspartate aminotransferase (average value - 151 U/l) (94.7%), gamma glutamyl transpeptidase (84.6%), bilirubin (52%). In the vast majority of cases, cholesterol levels are normal (1.54–4.58 mmol/l). Elevated cholesterol levels (> 5.17 mmol/l) are observed in 5% of cases. Children with high cholesterol levels do not have delayed physical development, life expectancy can reach 12 months (subject to further liver transplantation).
Cholesterol ester storage disease
The disease has a slower progression and does not develop as rapidly as the infantile form. The disease can manifest at any age, but in most patients it begins in childhood. It is likely that many patients do not survive to adulthood due to the development of life-threatening conditions (liver cirrhosis, liver failure, atherosclerosis, cardiovascular complications). The level of the enzyme lysosomal acid lipase can be reduced by 50-100 times. As a rule, the level of lipase in peripheral blood leukocytes does not exceed 5% of the norm [13].
Cholesteryl ester storage disease is a progressive, metabolic liver disease with an autosomal recessive pattern of inheritance. DLCL leads to the primary accumulation of cholesteryl esters and triglycerides in hepatocytes and macrophages. As a consequence, the development of hepatomegaly, microvesicular steatosis, cirrhosis, dyslipidemia, and early atherosclerosis. Clinical manifestation of the disease is possible both in the first year of life and at an older age. Statin therapy does not lead to reversal of the disease. The only treatment method with proven effectiveness is enzyme replacement therapy.
In cholesteryl ester storage disease, lipids accumulate in the liver and spleen. The level of cholesterol in liver tissue exceeds the norm by 70 times or more. Dyslipidemia is noted (increased levels of total cholesterol, low-density lipoproteins, sometimes triglycerides, decreased high-density lipoproteins). The accumulation of lipids in the intestines can cause gastrointestinal dysfunction. The accumulation of neutral fat and cholesteryl esters in the arteries causes early atherosclerosis. Hepatomegaly, hepatic fibrosis, cirrhosis are the result of the accumulation of cholesterol esters and triglycerides in macrophages and hepatocytes.
Morphological features of DLCL
Wolman's disease.
If it is possible to perform an intravital liver biopsy, all children show signs of fibrosis and/or steatosis. At autopsy, characteristic features are a large liver and spleen, yellow-orange coloration of the liver, necrosis of hepatocytes, fibrosis and cirrhosis, large adrenal glands with microcalcifications.
Cholesterol ester storage disease.
In the liver biopsy of all patients, characteristic pathological progressive signs are noted: microvesicular steatosis, contributing to the development of fibrosis, micronodular cirrhosis and ultimately liver failure (Fig. 2), the presence of histiocytes with ceroid material in the
lamina propria of
the villi of the duodenal biopsy (Fig. 3) [2 ], the formation of atherosclerotic plaques in the arteries [14], changes in the walls of the arteries (Fig. 4) [14].
Diagnosis of DLCL
Taking into account the close relationship between the clinical and pathomorphological picture of DLCL, the earliest possible diagnosis of this rare disease and timely administration of enzyme replacement therapy are necessary. The keys to early identification of DLCL and early diagnosis are high low-density lipoprotein levels, low high-density lipoprotein levels over a long period of time, and elevated transaminase levels. It must be remembered that DLCL is characterized by progressive impairment of liver function, often leading to transplantation. Any course of the disease is characterized by the presence of steatosis, often in combination with fibrosis and cirrhosis [4, 14]. DLCL should be excluded in patients with non-alcoholic fatty liver disease and non-alcoholic steatohepatitis.
The main laboratory method for diagnosing DLCL is to determine the activity of acid lipase in dried blood spots. In Russia, such a study is carried out in several scientific and medical centers, including in Moscow at the National Center for Children's Diseases and the Moscow State Research Center.
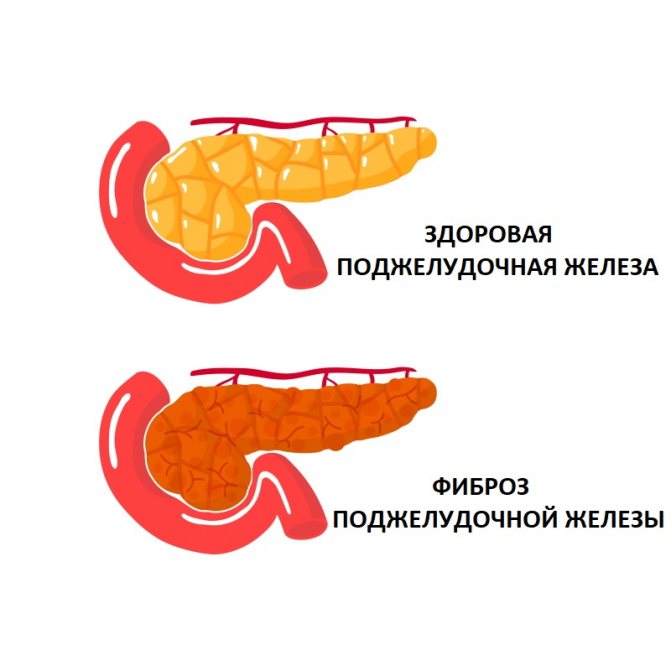
Lipase for pancreatitis
When pancreatic cells are renewed, a small part of the enzyme enters the blood. And this is completely normal and does not cause discomfort in a healthy person. But if the pancreatic tissue is damaged, the concentration of lipase in the blood increases greatly.
Interesting! Pancreatitis is often called a “disease of abundance,” because in most cases it occurs due to excess in eating and drinking.
In acute pancreatitis, lipase increase 3-10 times 4-8 hours after an attack and last up to 7-10 days. In other diseases, the enzyme concentration increases less intensely.
With chronic pancreatitis, these indicators will not be so high, because over time the pancreas loses the ability to produce the necessary enzymes. In this case, the concentration of lipase in the blood will be normal or even reduced.
Lipase - what is it?
An enzyme essential for normal digestion is lipase. It breaks down triglycerides (fats/lipids) into glycerol and carboxylic acids. Lipase is also important in the processing of vitamins (retinol, calciferols, tocopherol, phylloquinone, prenylmenaquinone) and linoleic, linolenic, arachidonic, eicosapentaenoic and docosahexaenoic acids.
It is produced by a variety of organs, depending on its origin, and is divided into:
- synthesized by the lungs (pulmonary);
- produced by the intestines;
- gastric (of particular importance in infancy, when the pancreas has not yet begun its production of enzymes);
- leukocyte;
- pancreatic;
- in infants, in the oral cavity (for the absorption of mother's milk) - lingual.

Pancreatic lipase plays an important role. Its content in human plasma is constant. But if degenerative processes occur with pancreatic acid cells, then the amount of lipase increases.
Taking Pancreatin to compensate for lipase

In order for food to be completely digested and all the necessary substances to be absorbed by the body, a sufficient amount of enzymes is required:
- lipases;
- amylase;
- trypsin;
- chymotrypsin.
If there are not enough of them, the person requires replacement therapy. One of the most effective drugs is Pancreatin. It helps in the breakdown of carbohydrates, proteins and fats, and is used in the treatment of pancreatitis. With its help, digestion processes are normalized, and the functional state of the gastrointestinal tract is improved.
On a note! Pancreatin is an international nonproprietary name (INN). Therefore, many manufacturers can produce it under the same name, because The name "Pancreatin" does not belong to anyone.
Pancreatin: at the pharmacy
In any pharmacy in Moscow and St. Petersburg you can find a variety of drugs containing lipase . Manufacturers promise an almost instant effect. Or vice versa, you need a lot of pills and take them for a very long time. And many people have long noticed that conventional drugs do not always give the expected effect. There are good drugs in pharmacies, but many people prefer to order dietary supplements on iHerb.com, because... All products are shipped from warehouses in the USA. And here many people from Russia and 150 countries around the world regularly place orders for various herbal supplements and vitamins. When purchasing dietary supplements and sports nutrition from iHerb, you can be confident in its quality and originality. iHerb works only with trusted manufacturers.
All products are purchased, stored and delivered in accordance with all GMP and manufacturer safety requirements. Humidity and temperature conditions are regularly monitored. Absolutely all additives have documents confirming the quality of the products.
Pancreatin: instructions
The enzyme preparation is often used in gastroenterology. It facilitates the digestion of food and promotes better absorption of essential vitamins and microelements in the small intestine. Since the enzymes contained in the product lose activity when exposed to gastric juice, the medicine is available in the form of tablets or capsules coated with a special coating. It is destroyed in the intestines, activating enzymes.
How to use

How and in what quantities to use the drug depends on the dosage, age of the patient, diagnosis, form of release and other factors. It is better if the prescription is made by a doctor after all the necessary examinations.
Important! Preparations containing digestive enzymes are taken with meals or immediately after meals, unless otherwise indicated in the instructions.
The recommendations for the dosage form of the specific drug used, indications for use and dosage regimen should be strictly followed. The daily dose for an adult is 150,000 units/day. The duration of treatment depends on the disease and can vary from several days and even up to several years.
Prevention of lipase surges
Like any other malfunction in the body, lipase surges can be avoided by following some rules:
- Diet. It is useful to eat small and often, dividing portions into smaller ones. Don't skip breakfast. Compliance with sanitary and hygienic standards.
- Diet. Avoid smoked, fried, spicy, too salty foods. But fiber-rich foods can be consumed in unlimited quantities. Cabbage, legumes, radishes, mustard, and garlic cause gas formation in the intestines, so it is worth limiting their consumption.
- Don't overeat. The standard serving for an adult is 300-400 ml.
- Drink enough fluids. It is recommended to drink a glass of warm water half an hour before meals.
- Keep your body weight under control. Excess weight aggravates the course of diseases and provokes increased symptoms.
- Quitting alcohol. Many alcoholic drinks contain dyes, preservatives, sugars and flavorings, which negatively affects the functioning of the pancreas. Although conditionally safe doses of ethanol have been established, it is better to refrain from drinking it completely.
- Minimize the amount of stress, walk more, relax and get enough sleep.
- If you smoke, you should definitely give up cigarettes. Tar and nicotine significantly weaken the body and subject it to additional stress.
- Increase your level of physical activity. Swimming strengthens you well, improves intestinal motility, take advantage of every opportunity to move more often.
- If you have diabetes, monitor your blood sugar levels especially carefully.
- Follow all the recommendations of your doctor, undergo regular medical examinations, and if you have chronic diseases, regularly take tests for control.
- Taking many medications can provoke the development of diseases of the gastrointestinal tract, so be sure to consult your doctor before taking it.
Timely diagnosis of diseases of the gastrointestinal tract, and especially the pancreas, is the key to quickly relieving the main symptoms of the disease. And a huge role in this diagnosis belongs to lipase analysis, which helps to accurately diagnose and begin therapy as quickly as possible, avoiding serious consequences.
Pancreatin: reviews
Diseases of the pancreas occur at any age, especially in those people who do not particularly monitor their diet, exceed the portions required by the body and abuse alcohol. Pancreatin is extremely necessary in the first aid kit, people with gastrointestinal problems note in reviews. The effect after administration occurs literally within 30-40 minutes. As a rule, it is prescribed by doctors, because this drug has proven itself well. Take Pancreatin alone or in combination with other medications. Many people have known pancreatin since the times of the USSR.
People with chronic pancreatitis take a course of the drug for prevention 1-2 weeks before the holiday feast. The drug helps improve the functioning of the gastrointestinal tract and also replenishes the deficiency of digestive enzymes.
The main contraindication is individual intolerance, but it occurs in only 1% of people taking Pancreatin. If you follow all the recommendations and follow a diet, this will allow you to avoid surgical intervention and quickly return to your normal life.
On average, in reviews in general, people note the positive role of Pankratin in alleviating the gastrointestinal tract after:
- abundant holiday food;
- food poisoning;
- consuming stale or not very clean products from hand in markets, stalls, etc.










