directions
Fine-needle aspiration biopsy (FNA) of thyroid nodules is a highly informative method for diagnosing thyroid tumors. FNA makes it possible to determine whether a thyroid nodule is benign or malignant. Currently, biopsy is considered the most accurate preoperative method to determine the nature of the nodular formation. During the manipulation process, the doctor, using a thin needle, aspirates cellular material from the thyroid nodule, based on the contents, makes a diagnosis and determines treatment tactics (conservative therapy or surgical intervention). The procedure is unpleasant, but practically painless, the sensations are similar to an intramuscular injection, and therefore is performed without anesthesia.
Our clinics in St. Petersburg
Medical center on Pionerskaya Polikarpov Alley 6k2 Primorsky district
- Pionerskaya
- Specific
- Commandant's
Medical center South-West Marshal Zhukov Ave. 28k2 Kirovsky district
- Avtovo
- Avenue of Veterans
- Leninsky Prospekt
Medical center in Devyatkino Okhtinskaya alley 18 Vsevolozhsk district
- Devyatkino
- Civil Prospect
- Academic
For detailed information and to make an appointment, you can call +7 (812) 640-55-25
Make an appointment
Integration of various laboratory methods
When establishing a cytological diagnosis, data from a study of the hormonal status of the thyroid gland are of great importance. To clarify the morphological diagnosis, immunocytochemical or other molecular, including molecular genetic studies are used. A pronounced immunocytochemical reaction of tumor cells to mesothelin (HBME) and galectin confirms the malignant nature of the tumor. If metastases of papillary or follicular thyroid cancer are suspected, the nature can be clarified by determining thyroglobulin.
Genetic predisposition and instability of the RET/PTC genome can “trigger” the mechanism of malignant transformation and further damage to the genome (TP53, CTNNB1 and other genetic changes contribute to tumor progression). Depending on molecular genetic findings, it is possible to determine the phenotypic characteristics of the tumor and the prognosis of the disease.
Indications for aspiration biopsy
- Neoplasms larger than 10 mm;
- Fast-growing nodular formations;
- Multinodular goiter;
- Clinical signs of a malignant tumor (fatigue, weight loss);
- Signs of a malignant formation according to the results of ultrasound diagnostics (uneven contours of the node, fusion of the tumor with other organs and tissues, many vessels or microcalcifications in the node, impaired blood flow in the pathological formation);
- Exposure due to living in a radiation zone;
- Oncological diseases in close relatives.
If suspicious lumps are detected in the thyroid gland area, you need to undergo a diagnostic examination as quickly as possible, which will make it possible to determine the nature of the neoplasm.
How to normalize thyroid hormones
An endocrinologist treats organ dysfunction. His recommendations depend on the causes of hypothyroidism or thyrotoxicosis. If there is a lack of biologically active substances, the doctor will prescribe replacement therapy drugs. The dose is selected individually.
For thyrotoxicosis, agents are indicated to suppress excess production of TSH, T3 and T4. If drug therapy is ineffective, surgical treatment is prescribed.
If a malignant neoplasm is detected, the organ and regional lymph nodes are removed. Radioiodine therapy is prescribed. After treatment, lifelong use of levothyroxine is indicated.
Crossing the border between normal and pathological in diseases of the thyroid gland is very simple. It is enough to ignore the recommendations of the endocrinologist and self-medicate.
Methodology
The doctor treats the injection site with an antiseptic, pierces the skin and, under constant visual control on the monitor of an ultrasound machine, removes the maximum amount of material with a thin needle. During the TAB procedure, the patient should not talk or swallow, and there is no need to hold his breath. The injection and aspiration from the node take a few seconds.
Biopsy of thyroid nodules is always performed under ultrasound guidance. The use of an ultrasound machine allows a specialist to assess the size, shape and structure of the thyroid gland formation, determine the site of the pathological process and get the puncture needle into the gland area as accurately as possible, without damaging nearby neck organs, large nerves and blood vessels. It is not allowed to perform a biopsy without using an ultrasound machine! Ultrasound sensors determine the puncture site and control the movement of the needle into the tissue of the node.
After taking cells from the pathologically changed node, the material is sent to the laboratory to study the nature of the neoplasm. Based on the results of cytology, it is possible to diagnose thyroid cancer or, conversely, to recognize that the tumor is benign. The accuracy of the study is 98%.
After taking an aspirate from the thyroid area, the patient can immediately leave the clinic and engage in physical activity and normal activities without restrictions.
Bethesda system for assessing thyroid cytology obtained by FNA
DOI: 10.18508/02107
Bethesda Thyroid
Cytology Evaluation System The Bethesda System For Reporting Thyroid Cytopathology (TBSRTC)
(Cibas and Ali)
To define terminology and address other issues related to fine-needle aspiration biopsy (FNA) of the thyroid gland, the US National Cancer Institute held a scientific conference in Bethesda, Maryland.
- The project allowed the development of the Bethesda system for assessing thyroid cytology.
- The flexible structure of the TBSRTC aims to facilitate mutual understanding among cytologists, endocrinologists, surgeons, radiologists, and other health care professionals and recommends that each FNA report begin with one of 6 major diagnostic categories.
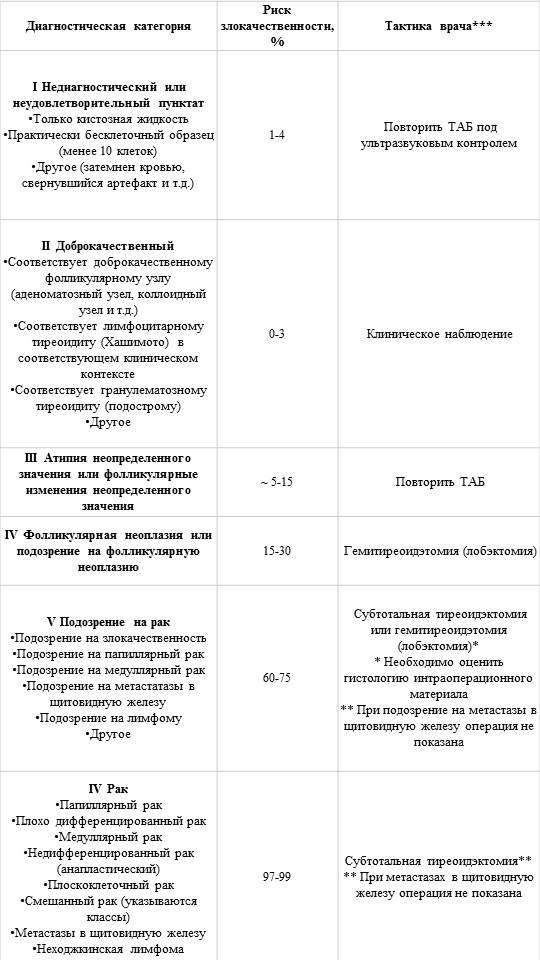
| Diagnostic category | Risk of malignancy, % | Doctor's tactics*** |
I Non-diagnostic or unsatisfactory punctate
| 1-4 | Repeat TAB under ultrasound guidance |
II Benign
| 0-3 | Clinical observation |
| III Atypia of undetermined significance or follicular changes of undetermined significance | ~ 5-15 | Repeat TAB |
| IV Follicular neoplasia or suspected follicular neoplasia | 15-30 | Hemithyroidectomy (lobectomy) |
V Suspicion of cancer
| 60-75 | Subtotal thyroidectomy or hemithyroidectomy (lobectomy)* * It is necessary to evaluate the histology of intraoperative material **If metastases to the thyroid gland are suspected, surgery is not indicated |
VI Cancer
| 97-99 | Subtotal thyroidectomy** ** For metastases to the thyroid gland, surgery is not indicated |
*** The doctor’s tactics, in addition to the cytology results obtained by FNA, may depend on other factors (for example, the clinical picture, ultrasound data).
Source:
Cibas ES1, Ali SZ. The Bethesda System For Reporting Thyroid Cytopathology. Am J Clin Pathol. 2009 Nov;132(5):658-65. doi: 10.1309/AJCPPHLWMI3JV4LA.; NCI Thyroid FNA State of the Science Conference.
Interpretation of biopsy results
As a result of laboratory testing, the nature of the biopsy is determined and a conclusion is made:
- Benign nodule;
- Malignant formation;
- Follicular tumor, which does not make it possible to accurately determine the nature of the formation;
- The material is uninformative (in this case, repeated collection of cellular material is required).
Malignant and follicular formations are indications for surgical treatment of neoplasms.
In a multidisciplinary medical center, a fine-needle biopsy of thyroid nodules is performed by an experienced endocrinologist. Taking a biopsy in the Medicenter clinic network is carried out under ultrasound control, which allows you to accurately determine the location and nature of the pathology and not harm the patient’s health.
TAB technique
FNA is preferably performed on an outpatient basis. The patient is previously informed about the limitations of this diagnostic procedure (the possibility of obtaining an inadequate punctate or the so-called “definite” conclusion of a cytological examination), as well as painlessness and the absence of any significant complications.
The patient is in a supine position with a pillow under his head, which ensures relaxation of the cervical muscles. The nodular formation is palpated, after which the patient is asked to swallow saliva several times to prevent this from happening during puncture. The needle is inserted into the node, after which slow aspiration is carried out, which stops immediately after the aspirate appears in the syringe and before the needle moves to the side, which avoids the contents of the channel made by the needle getting into the aspirate.
TAB does not have any significant complications. These include subcutaneous hematomas, hemorrhages in the area of the node and local pain that persists for some time. In rare cases, after aspiration of cystic formations, acute inflammatory processes may develop. There are some rare descriptions of the development of acute thyroiditis, transient bradycardia and transient paresis of the vocal cord.
Carrying out ultrasound-guided FNA (US-FNA) leads to a significant increase in the diagnostic information content of the entire study. This method is indispensable for puncture biopsy of non-palpable, but rather large nodular formations, as well as for visualization and targeted puncture of solid components of cystic nodes.
Number of punctures per node. Thyroid nodules often have a heterogeneous structure. In order to examine different areas of such nodes, several aspirations from the same node may be necessary.
Thyroid nodules
Thyroid nodules are the most common type of pathology of this organ. According to modern data, ultrasound examination can reveal nodes in the thyroid tissue of 30-67% of Russian residents. In the vast majority of cases (95%) thyroid nodules are benign, and in only 5% of patients they are malignant tumors, i.e. cancer.
Currently, science has clearly proven that benign nodes cannot “degenerate” into cancer (malignize). The idea that still exists in some clinics that any thyroid nodule should be removed without fail in order to prevent the development of cancer in it has long been recognized as erroneous. Removing all benign thyroid nodules without exception (some doctors recommend this!) will only lead to the fact that half of the population of our country will undergo surgery and have a stitch in their neck... fortunately, such a prospect is unrealistic - even if such operations were possible necessary, no country in the world has enough endocrine surgeons and health care resources to perform such an “experiment.”
To determine the nature of the thyroid nodule (whether it is benign or malignant), a fine-needle biopsy is used. This type of examination is indicated for all patients with thyroid nodules measuring 1 cm or larger, and also in some cases for patients with smaller nodules (if the patient has relatives with thyroid cancer, or if the patient has been exposed to radiation during his life). Patients with nodules up to 1 cm in the vast majority of cases do not need treatment - they are recommended to undergo an ultrasound of the thyroid gland annually (i.e. once a year, not more often!) in order to monitor the process of changing the size of the nodule.
It is important to note that without a fine-needle biopsy, high-quality patient treatment is impossible in our time. This seems completely logical: how can we determine the treatment strategy for a patient if we do not know whether we are dealing with a harmless benign nodule or thyroid cancer? Only a fine-needle biopsy allows one to clearly determine the nature of the nodule and give the patient competent recommendations. Unfortunately, it is still often necessary to meet with patients for whom doctors have performed a lot of research - ultrasound, scanning, computed tomography, hormonal studies - in short, everything that modern medicine can offer, but they have “forgotten” about fine-needle biopsy. The result of this approach is missed cases of cancer, or recommendations to undergo surgery even for patients with thyroid nodules that are not life-threatening.
Once the colloidal (i.e., benign) nature of the nodule is confirmed by biopsy, the physician must decide whether to treat the patient. Currently, there are no medications that would reduce the size of the node. Thyroxine therapy, which has been used for a long time by endocrinologists, is now recognized not only as ineffective, but also often dangerous. Surgical treatment in Russian conditions is practically the only method of treating patients with thyroid nodules. Radioactive iodine therapy, which is widely used abroad, despite its effectiveness, is used very limitedly in our country - we do not have a sufficient number of centers capable of conducting such treatment.
Patients with colloid thyroid nodules do not require any treatment if the nodes do not cause them complaints or changes in hormonal levels. Such “asymptomatic” nodes do not interfere with the patient’s quality of life and should not be treated, regardless of their size and location.
Surgical treatment of patients with nodes should be carried out in the following cases:
- if the node has reached such a size that it begins to compress the organs of the neck and cause a feeling of suffocation (due to compression of the trachea), disrupt the swallowing process (due to compression of the esophagus), or simply cause the patient a painful feeling of a “foreign body in the neck” (in this case, patients should be distinguished with true compression of the neck organs by a knot from neurotic patients complaining of a “lump in the throat”). The presence of compression of the neck organs by a knot must be confirmed instrumentally - most often using computed tomography of the neck area;
- if a large-sized node causes a cosmetic defect, deforming the front surface of the patient’s neck (it is important to note that such a defect should bother the patient, prevent him from living peacefully, and not just be noticed by the doctor during examination);
- if during the existence of the node it has acquired the ability to produce uncontrolled hormones (i.e. a so-called autonomous, or toxic, node has formed), which causes the appearance of thyrotoxicosis - an excessive level of thyroid hormones in the blood.
In our country, surgical treatment is very often recommended for patients whose nodes exceed 3 cm in size. It is still not clear who proposed this figure as a certain “border”, after which the patient should be recommended to undergo surgery, and also for what reason exactly 3 centimeters were chosen as the "border". Indeed, why not recommend surgery to everyone whose node size has reached 4 or 5 centimeters? Why do doctors recommend surgery for a patient with a node size of 3.1 cm, but not yet for a patient with a node size of 2.9 cm? What to do with patients who have two 2 cm nodes - to operate or not? On the one hand, 2 nodes of 2 cm each give a total of 4 centimeters, and on the other hand, each of them is still less than 3 cm in diameter... How can you explain, for example, to an Englishman that in our country there is a patient with a node with a diameter of 1.18 inches (namely this is how 3 centimeters look in inches) will they be referred for surgery, but with a knot of 1.16 inches - not? Nevertheless, thousands of patients in our country undergo removal of thyroid nodules every year based on the “three-centimeter rule.”
Of course, no numerical values can be used as an indication for surgery, because people are not alike, and fixed digital norms usually do not apply to them. The general rule should be to prescribe surgical treatment only to those patients with benign nodes who are concerned about their disease. If the node did not allow the patient to breathe normally before the operation, and after the operation this problem disappeared, then the patient will be satisfied with both his doctor and the treatment performed. If before the operation the patient had a node measuring, say, 3 centimeters in size, which did not cause absolutely any sensation, and after surgery the node disappeared, then what will such a patient gain from the operation? There were no complaints before treatment, and there won’t be any after it, so the patient will not feel any improvement in his condition. Meanwhile, surgery cannot be called a pleasant procedure; any surgical intervention is always stressful for the patient, it involves severe pain to one degree or another, and the appearance of a cosmetic defect in the form of a suture on the neck. We should also not forget about the possibility of postoperative complications and complications of general anesthesia (anesthesia). And, of course, it should be borne in mind that in modern conditions, surgery almost always costs money that the patient could spend on completely different needs.
It turns out that surgery on an “asymptomatic” patient brings only disadvantages, and its advantages are completely unobvious. That is why the world's major associations of endocrinologists recommend not treating patients who do not have complaints related to thyroid nodules. Such patients need to be monitored, i.e. Conduct an ultrasound of the thyroid gland no more than once a year and determine the level of the hormone TSH in the blood - no great effort is required.
In order for a benign thyroid nodule to become a reason for surgical treatment, it must reach a significant size and begin to cause the patient complaints of difficulty breathing or swallowing. The operation is also recommended for patients with benign nodes that actively produce hormones - if the excessive function of the nodes is so pronounced that the general hormonal background of the body changes. In the vast majority of cases, benign thyroid nodules are not a reason for surgical treatment. It should be remembered that such nodes are most often not dangerous for patients, therefore excessively active tactics of their treatment only cause harm to patients. If a patient has a single benign thyroid nodule that requires surgical treatment, the operation is performed as a hemithyroidectomy—removal of the lobe of the gland containing the nodule. With large nodules, usually the entire lobe of the gland is occupied by the nodule, so partial resection of the lobe should not be carried out - this will not help preserve a significant amount of gland tissue and will only increase the likelihood of recurrence of nodular goiter. If a patient has a multinodular goiter—multiple thyroid nodules—a thyroidectomy (complete removal of the gland) or subtotal resection leaving a small amount of gland tissue is usually recommended. In this case, again, you should not strive to leave the thyroid tissue - after all, the appearance of multiple nodes indicates the tendency of the thyroid tissue to undergo nodular transformation. Leaving such gland tissue during surgery leads to a significant increase in the likelihood of the formation of new nodes in the postoperative period.