Structure of the thyroid gland
The thyroid gland, by its origin, belongs to the intestinal canal. At 3-5 weeks of gestation, a protrusion appears on the anterior wall of the pharynx, between the I and II pairs of gill pouches. The bottom of the resulting bag is directed down the anterior surface of the larynx and trachea. The rudiment of the anterior part of the thyroid gland descends along the ductus thyreoglossus, then the duct is overgrown (the rest of it is for. caecum on the root of the tongue). The lateral parts of the gland are also formed by eversion of the wall of the digestive tube, but below the unpaired bud, in the area of the esophagus.
Click on pictures to enlarge.
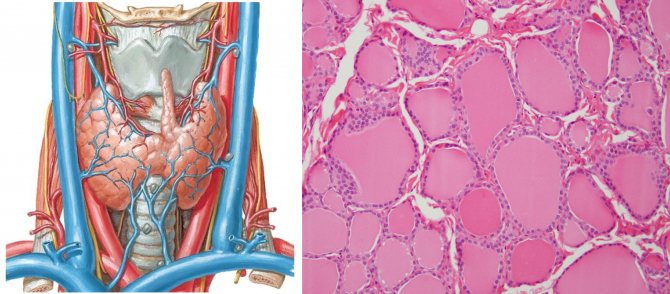
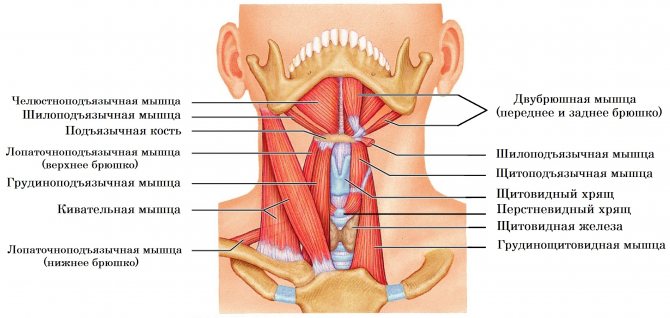
The thyroid gland lies in the anterior part of the neck, with its upper edge touching the thyroid cartilage; consists of two lobes of unequal size and an isthmus; sometimes the isthmus is absent.
Sometimes a pyramidal process extends upward from the isthmus; sometimes it reaches the hyoid bone, and to meet it from for. The coecum of the tongue stretches a canal that may be in connection with the accessory lobe of the thyroid gland, which lies above the body of the hyoid bone.
The parenchyma of the gland consists of round, completely closed vesicles - follicles. The wall of the follicle consists of thyrocytes surrounded by a basement membrane.
The basal surface of thyrocytes is closely adjacent to the capillaries, the apical part faces the lumen of the follicle; colloid with thyroglobulin is secreted into the lumen of the follicle, and the hormones thyroxine and triiodothyronine are secreted into the blood.
Each lobe of the thyroid gland is covered in front by the sternohyoid, sternothyroid and superior belly of the omohyoid muscle; from the sides - the sternocleidomastoid muscle; behind is the longus colli muscle.
The thyroid gland is adjacent to the neurovascular bundle of the neck - the common carotid artery, internal jugular vein, vagus nerve; The recurrent laryngeal nerve passes along the posterior surface.
The posterior surface of the thyroid gland wraps around the upper rings of the trachea; the lower sections reach the fifth and sixth rings.
The thyroid gland is covered with two connective tissue capsules. Violation of the integrity of the capsule when the tumor grows beyond the gland indicates the generalization of the malignant process and dictates the need for external beam radiation treatment or iodine therapy.
With connective tissue bundles, the external bursa secures the thyroid gland to neighboring organs - the cricoid cartilage, trachea, sternohyoid and sternothyroid muscles.
Lymphatic drainage from the thyroid gland is directed to the lymph nodes along the neurovascular bundle, along the sternocleidomastoid muscle, supraclavicular and pretracheal lymph nodes.
Ultrasound of the thyroid gland
The patient is in a supine position with a pillow under the shoulders. A 10-15 MHz linear sensor is used. We are interested in the size, echogenicity and echostructure of the thyroid gland. It is important to examine the lymph nodes in the neck, especially when a suspicious node is found in the thyroid gland. For more details, see Lymph nodes on ultrasound.
Drawing. Each lobe is scanned in the transverse (1) and longitudinal (2) plane. In the anterior mediastinum (3) there may be an intrathoracic goiter, and behind the trachea (4) there may be ectopic lobules of the thyroid and parathyroid glands.

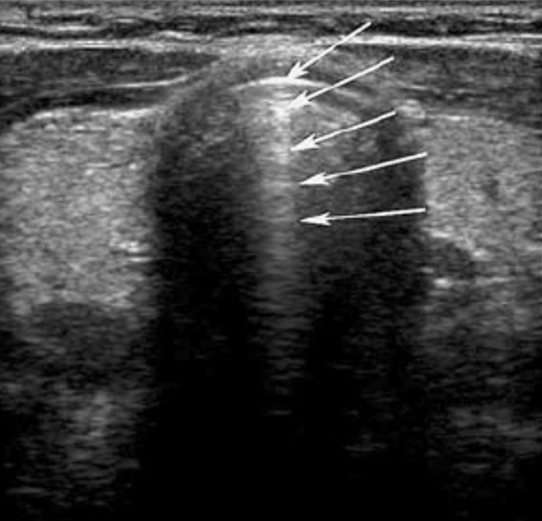
Drawing. On ultrasound, only the anterior wall of the trachea is visible; behind it is an acoustic shadow due to the reflection of the signal at the boundary of two media (tissue and air). Parallel lines behind the anterior tracheal wall are often mistaken for tracheal rings, but are actually a reverberation artifact.
Drawing. On transverse scanning, the left (LTL) and right (RTL) lobes of the thyroid gland resemble triangles separated by the isthmus (ISM). The anterolateral border is adjacent to the sternothyroid (STM) and sternohyoid (SHM) muscles, and the sternohyoid muscle (SCM) is located laterally. The muscles are hypoechoic compared to the parenchyma of the gland and have a fibril structure; they are covered by the fascia of the neck (FC), which is woven into the subcutaneous muscle of the neck (PM) and skin (SK). The posterolateral border is in contact with the neurovascular bundle of the neck: internal carotid artery (CA), internal jugular vein (JV), vagus nerve (not visible on ultrasound), jugular lymphatic duct (not visible on ultrasound). The parathyroid glands are usually not visible unless they are enlarged. The lower angle on the right rests on the longus colli muscle (LCM), and on the left on the esophagus (ESP). When the patient swallows saliva, peristalsis is detected in the esophagus. The inner side is adjacent to the trachea, where the recurrent nerve (not visible on ultrasound) and the inferior thyroid artery pass through.
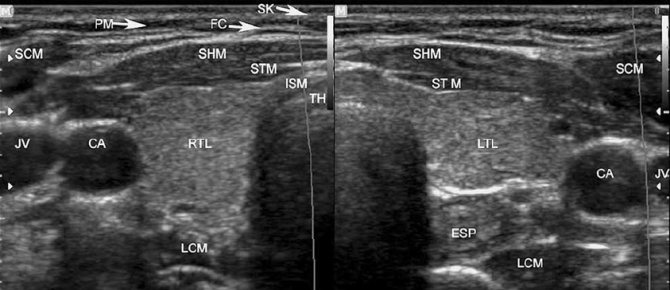
Drawing. In a longitudinal section, the lobe of the thyroid gland has an oval shape: PM - subcutaneous muscle of the neck, FC - cervical fascia, SH - sternohyoid muscle, ST - sternothyroid muscle, TL - lobe of the thyroid gland, LC - longus colli muscle.
Signs of nodes
The early stages of nodular thyroid disorders are asymptomatic. The size of a formation less than 1 cm does not reveal itself in any way, both externally and during the process of collecting anamnesis data. They are noted only during preventive examinations or additional examinations during the development of other diseases. True, nodular formations larger than 0.5 cm in size can be palpated if they are on the surface of the gland or along its edges. This pathological area remains in place when trying to displace it; it differs from neighboring tissues in a greater degree of density.
A rapidly growing nodule of the right lobe of the thyroid gland, causing compression of the esophagus and trachea
The patient can feel the node on his own or notice its existence when its size becomes more than 3 cm. Sometimes this cosmetic defect is noticed visually by strangers. Failure to contact an endocrinologist in a timely manner reduces the possibility of using conservative therapy. Typically, the initial signs of the disease are expressed in:
- painful sensations in the cervical region of unknown duration;
- the appearance of a sensation of a foreign object in the throat, creating difficulty in swallowing as the node develops;
- sore throat;
- breathing complications, since an enlarged thyroid gland compresses the airways passing behind the gland;
- changes in voice timbre due to compression of the laryngeal nerve innervating the vocal apparatus of the larynx;
- enlarged lymph nodes, as an extreme symptom with suspicion of the development of metastases in them due to a malignant tumor in the endocrine gland.
If an autonomous nodule develops in the thyroid gland, the patient may feel symptoms similar to manifestations of hypothyroidism: arrhythmia, emotional outbursts, exophthalmos, chaotic tachycardia, hot flash, etc. Identification of a solitary node is an indication for further, in-depth examination of the patient to identify the formation as benign. If the malignant nature of the neoplasm is confirmed, then the progress is one of the fastest, and nearby lymph nodes are also affected.
With the development of multiple nodes, confirmed during examinations (multiple adenoma), the prognosis is more favorable, although an in-depth examination is desirable. Despite the high quality of modern diagnostic methods, patients with thyroid nodules should be observed and examined by specialists before they are removed from the dispensary register.
When identifying symptoms, you should pay attention to children exposed to radiation in the cervical region, people who have relatives with papillary and medullary carcinoma, a period of life beyond adulthood, men, patients with high-density nodules. Suspicion is raised by nodes growing to the trachea or adjacent muscle tissue. Progressive symptoms such as dysphonia and dysphagia should be immediately diagnosed and examined by an endocrinologist.
Volume of the thyroid gland on ultrasound
The volume of the thyroid gland is equal to the sum of the volumes of the right and left lobes; the isthmus is neglected. It is required to display a longitudinal and transverse image of the thyroid lobe in the plane of maximum section. Measure the length, height and width of each lobe. Most ultrasound machines calculate the volume of the thyroid lobe using the formula for an ellipsoid of revolution: Length*Height*Width*π/6, where π/6=0.523.
Studying cadaveric material, in 1984 Brunn calculated a correction factor that most accurately corresponded to the actual volume of the thyroid gland - 0.479 (instead of 0.523).
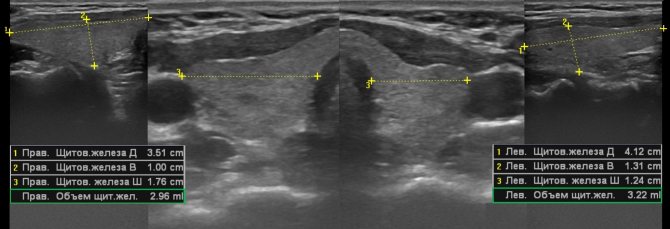
If the thyroid volume is greater than normal, it is hyperplasia, and if it is less than normal, it is hypoplasia. When the volume of the gland is at the upper limit of normal, the anteroposterior size of the isthmus is taken into account: if the isthmus is more than 3 mm before 10 years or more than 5 mm after 10 years, then the gland is considered enlarged.
The volume of the thyroid gland depends on gender, age and location. See the normal volume of the thyroid gland in children and adults here.
Minerals
Iron affects hemoglobin levels, which ensures the transfer of oxygen to body tissues. If there is a lack of iron, then problems with the endocrine system begin, in particular, there are risks of developing hyperthyroidism.
If any problems begin, then you should refrain from manipulating the neck area, notes the endocrinologist. In particular, we are talking about various procedures, for example, from a cosmetologist.
“Any procedures are contraindicated during periods of exacerbation of thyroid diseases. During the period of remission, consultation with a specialist is necessary for specific procedures (for example, massage, cosmetic procedures), says Elena Gubkina.
The thyroid gland should be given maximum attention, then it will pay back in kind: it will maintain health and work like a clock.
Echogenicity of the thyroid gland on ultrasound
The echogenicity of the thyroid gland can be assessed in comparison with the muscles of the neck, spleen and parotid salivary gland. Normally, the echogenicity of the muscles is much lower, and the spleen is close, but not identical, to the thyroid gland. The parotid gland is most suitable for assessing echogenicity.
Drawing. Echogenicity of the spleen (1), thyroid (2) and parotid (3) glands.
Drawing. With autoimmune damage, the echogenicity of the thyroid gland decreases and approaches the neck muscles. See more details here.
Prevention
To protect your health, you should not turn a blind eye to signs of diffuse changes in the thyroid gland and put off visiting a doctor. Despite the fact that today medicine makes breakthrough after breakthrough, specialists have not been able to determine the nature of thyroid disorders, and therefore there is no sure way to prevent such ailments. But not everything is so pessimistic: it is still within our power to prevent some conditions. For example:
- If there have been cases of such diseases in the family, you need to try to protect yourself from exposure to provoking factors - for example, to prevent exposure to toxic substances.
- To prevent iodine deficiency, you need to eat foods that contain this substance: seafood, seaweed, fatty fish, apples, plums, apricots and grapes, milk, cheese and cottage cheese. You can also replace regular salt with iodized salt.
- Excess weight often provokes thyroid diseases, so you need to reconsider your diet and choose the appropriate type of physical activity.
- If the diagnosis has already been made, do not forget to regularly visit a specialist and do an ultrasound to prevent the development of pathology.
Echostructure of the thyroid gland on ultrasound
The echostructure of the thyroid gland is assessed as homogeneous or heterogeneous. Homogeneous tissue is characteristic of a healthy thyroid gland, as well as the initial stages of diffuse non-toxic goiter. The echostructure is described as heterogeneous with a focal or diffuse arrangement of foci of varying echogenicity.
Diffusely heterogeneous echostructure of the thyroid gland in AIT
- little changed tissue – against the background of normal parenchyma, hypoechoic inclusions are determined (2-4 mm);
- altered tissue - against the background of reduced echogenicity, hypoechoic inclusions are determined (4-6 mm);
- dramatically changed tissue - against the background of a general decrease in echogenicity, almost anechoic foci and hyperechoic structures of various sizes and shapes are determined.
Drawing. Ultrasound of a patient with autoimmune thyroiditis. Against the background of normal parenchyma, there are a large number of hypoechoic foci (3-5 mm) with a clear contour. Foci that are isoechoic to salivary gland tissue are not yet involved in inflammation; in sharply hypoechoic foci, inflammation is maximally expressed; in hyperechoic structures, parenchyma was replaced by connective tissue.
Blood flow in the thyroid gland on ultrasound
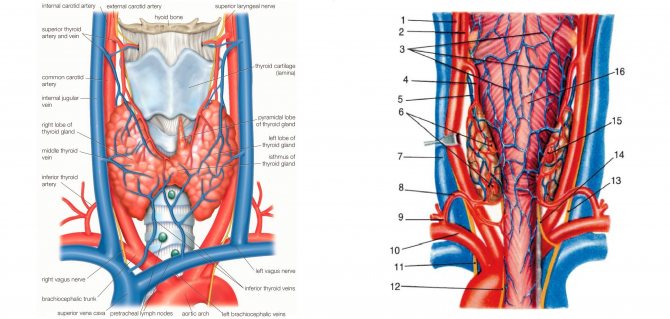
Each lobe of the thyroid gland is supplied by the superior and inferior thyroid arteries. The superior thyroid artery (a. thyroidea superior) departs from the external carotid artery at its beginning. The artery approaches the upper pole of the lobe and divides into posterior and anterior branches. The posterior branch descends along the posterior surface of the gland and anastomoses with a similar branch of the inferior thyroid artery (posterior longitudinal anastomosis). The anterior branch runs down the anterior surface of the gland and, at the upper edge of the isthmus, anastomoses with the artery of the same name on the opposite side (transverse anastomosis). The inferior thyroid artery (a. thyroidea inferior) departs from the thyrocervical trunk (a branch of the subclavian artery), approaches the posterior surface of the lobe and is divided into a number of branches that supply blood to the posterior surface.
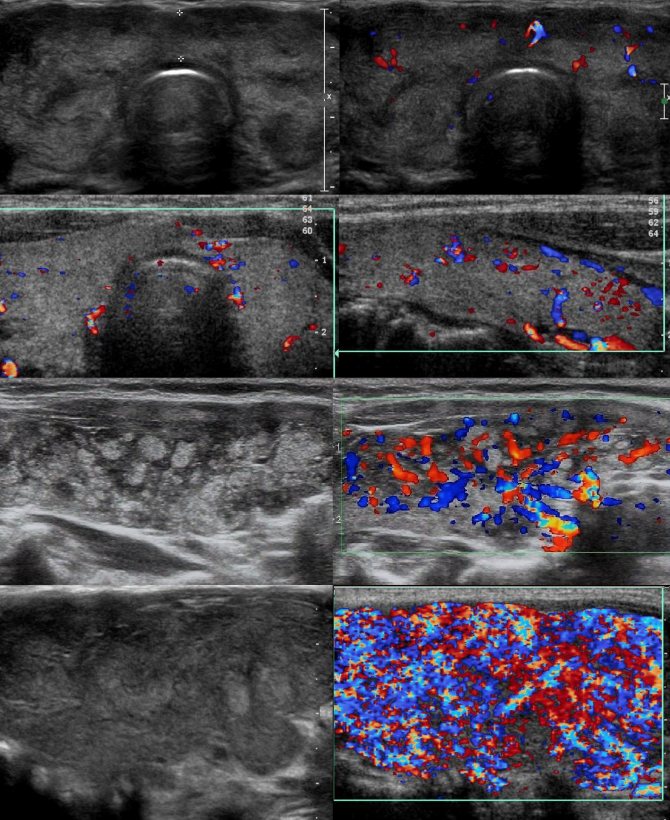
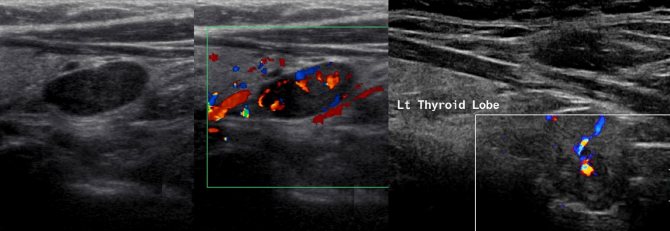
Thyroid gland in color flow mode
A healthy thyroid gland has a vascularization score of 0-3. An increase in blood flow up to 4-5 points occurs only in pathology.
- 0 points—colored pixels on a slice of a lobe are not detected;
- 1 point - single color pixels mainly along the periphery of the slice;
- 2 points - single colored pixels mainly in the thickness of the slice;
- 3 points - single color pixels along the periphery and in the thickness of the slice;
- 4 points—multiple colored pixels throughout the entire slice of the lobe;
- 5 points - a huge number of merging color echo signals throughout the slice.
Drawing. Assessment of the thyroid gland in the CDC mode: 2 points (1, 2), 3 points (3, 4), 4 points (5, 6) and 5 points (7, 8).
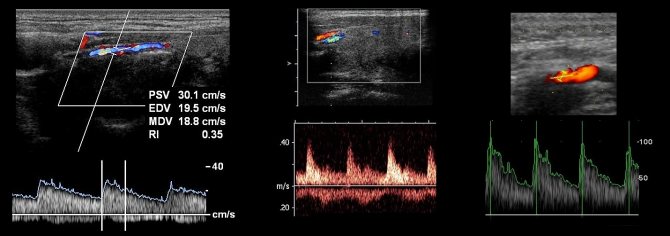
Thyroid gland in D-mode
- In the color flow mode, on a longitudinal section, find the location of a stable color signal from the artery;
- Switch to D-mode and set the control volume to the center of the vessel;
- Correct the angle between the ultrasound beam and the vessel to a value of no more than 60°;
- Freeze the spectrum with five complexes;
- Determine the qualitative and quantitative characteristics of the spectrum.
For more information, see Vascular Doppler for Beginners.
Blood flow parameters in the superior and inferior thyroid arteries do not differ. Normal PSV in the thyroid arteries is 20-28 cm/sec. When the maximum systolic velocity is more than 45 cm/sec, diffuse changes in the thyroid gland can be assumed. In small arteries of the parenchyma, the blood flow velocity does not exceed 10-20 cm/sec, peripheral resistance indicators have strict boundaries: RI ranges from 0.6 to 0.7, PI - from 1.0 to 1.5.
In diffuse toxic goiter and autoimmune thyroiditis, PSV can be more than 100 cm/sec. This is characterized by a sharp increase in blood flow throughout the thyroid tissue. Dynamic measurement of blood flow parameters provides valuable information regarding the course and prognosis of these diseases.
Drawing. Superior thyroid artery in D-mode: in a normal thyroid gland PSV 30 cm/sec, in subacute de Quervain's thyroiditis PSV 40 cm/sec, in diffuse toxic goiter PSV 98 cm/sec.
Treatment methods for nodules
The purpose of the treatment regimen is directly dependent on the number of nodules in the gland, their volume, overall health, and the patient’s age. If multiple small nodes are detected, the use of medications is not necessary; only constant monitoring by a specialist is required. A single small nodule is also not treated, but an examination and consultation with an endocrinologist is carried out 4 times a year. If necessary, the doctor prescribes additional tests.
Treatment of a cyst is determined by its volume: a large volume of a cyst, like colloid nodes, requires surgical intervention. A small volume of formation can be eliminated with sclerotherapy followed by iodine-containing and hormonal medications. If such methods do not give the expected effect and the tumor does not stop after 3 months, additional examination is carried out to exclude the possibility of autoimmune thyroiditis. Purulent inflammation within the formations requires a course of antibiotics and toxin suppression therapy.
The remaining nodes in the thyroid gland are treated surgically. The benign nature of the formation during surgery allows for incomplete resection of the thyroid gland; the remaining cells take on the functionality of the removed ones. In case of thyroid cancer, a total ectomy is performed, and for the rest of your life you have to take hormonal and calcium-containing medications due to the removal of the parathyroid glands.
Parathyroid glands on ultrasound
The parathyroid glands are located on the posterior surface of the thyroid gland outside its capsule near the upper and lower poles, have a round shape, and a diameter of up to 5 mm. Like the thyroid gland, they originate from the intestinal tube. Typically, a person has four parathyroid glands (two upper and two lower). Sometimes accessory parathyroid glands are found in the tissue of the thyroid and thymus glands, in the anterior and posterior mediastinum, in the pericardium, behind the esophagus, in the area of the bifurcation of the common carotid artery. The parathyroid glands supply the branches of the inferior thyroid artery. In only 10% of cases, the arteries for the superior glands arise from the superior thyroid artery.
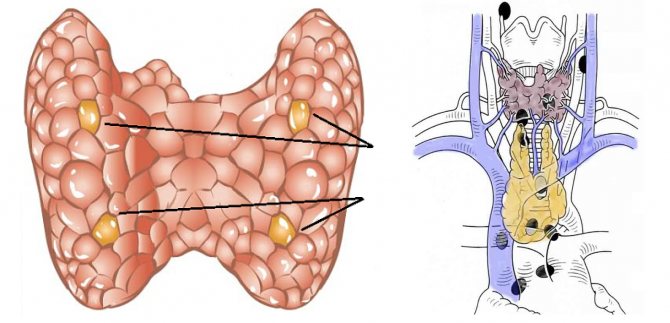
Normal parathyroid glands are very small (3-5 mm) and can only be identified with a high frequency probe. If the parathyroid gland is very clearly visible on ultrasound, then hyperplasia, adenoma or cancer should be suspected. Assess the size, shape, contour, echogenicity, and echostructure of the parathyroid gland.
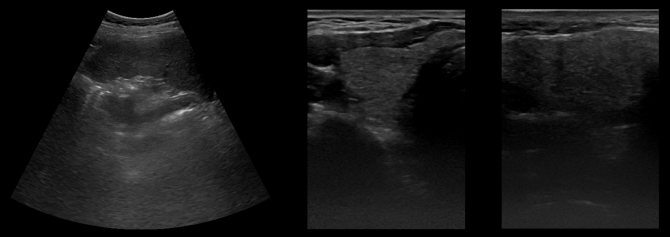
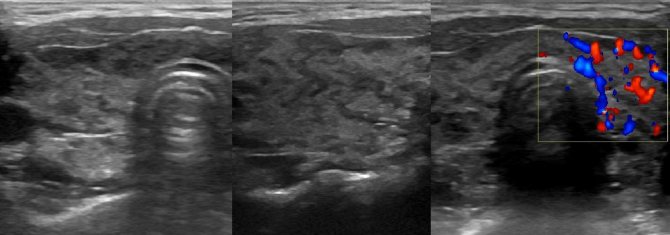
Drawing. Ultrasound shows a normal lower parathyroid gland on longitudinal (1) and transverse (2, 3) sections: hypoechoic round formations at the lower pole of the left lobe, with a clear and even contour, size 2.5*2*2 mm. Color flow will help distinguish glands from vessels.
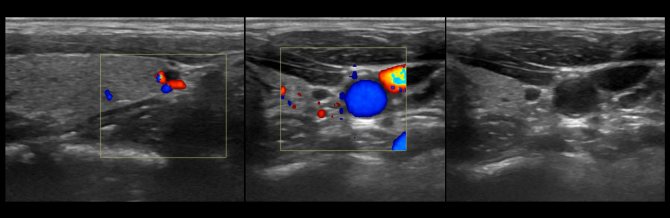
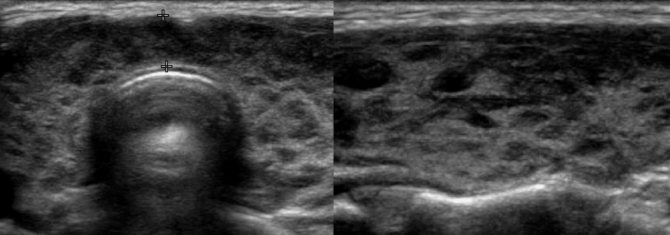
Drawing. In patients with hyperthyroidism, ultrasound shows hyperplasia of the parathyroid glands: at the lower poles of the thyroid gland, hypoechoic formations of irregular shape are detected, with a clear and even contour without a halo, and insignificant blood flow along the periphery. Enlarged parathyroid glands are often mistaken for a thyroid tumor.
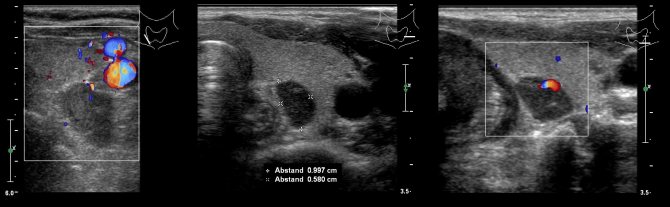
Drawing. Ultrasound at the lower pole of the thyroid gland clearly shows enlarged hypoechoic formations with increased blood flow. Regular shape with a clear and even contour (1, 2), probably a parathyroid adenoma. Irregular shape, unclear contour, heterogeneous echostructure with small cystic cavities are characteristic of parathyroid cancer.
Take care of yourself, Your Diagnosticer !
Tags: lectures, ultrasound, thyroid gland