Why are our women not in a hurry to regularly do mammography and ultrasound of the mammary glands? They are afraid that “something will be found” on them. In most cases, these findings - cysts, fibroadenomas, calcifications and dilated ducts - do not threaten health and do not require treatment, but sometimes require additional examination. Why do illiterate doctors scare women and what do the results of ultrasound and mammography actually say?
High mammographic density
High breast density on mammography is an unfavorable sign, as it makes it difficult to detect malignant tumors. Various international guidelines have identified “dense breasts” as a factor that increases the risk of breast cancer (BC). But don’t be scared right away, because these words refer to the high density of the mammary gland in a postmenopausal woman (after menopause).
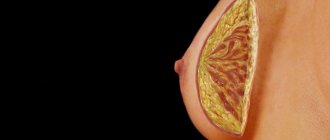
Why is that? The thing is that glandular tissue gives high density, that is, “opacity” in an x-ray image. With age, glandular tissue is replaced by fatty tissue (the breast undergoes fatty involution) and, therefore, becomes transparent in the image. All tumor nodes in such a transparent breast are clearly visible, and even the smallest of them are easy to detect.
But at the age of 30–45 years, glandular tissue is present in the breasts in significant quantities (for each woman this ratio is individual), and, accordingly, the breasts at this age may look “dense” on mammograms.
This is why mammography has the greatest advantage in detecting breast cancer in women 50 years of age and older (in many European countries, screening mammography is performed for women starting at 50 years old, and not at 40, as in Russia).
Why you shouldn't treat a breast cyst
These are round or oval structures filled with fluid, which in the vast majority of cases are benign formations that do not require any intervention.
Cysts can appear naturally at any age (with the exception of menopausal women, for whom cysts are very rare) as a result of normal fluctuations in estrogen levels in the body. They can be single or multiple, large or small, in one or both breasts.
A cyst can be identified by the woman herself or a doctor by touch - it is a smooth and easily removable round or oval “lump” with clear contours. Manifestations of a cyst can be pain and sensitivity in the breast, the appearance of some “lumps” on the eve of menstruation and their disappearance with its onset. Cysts most often appear and disappear on their own without any treatment.
The most informative method for identifying cysts is ultrasound. In this case, its type must be specified in the conclusion.
Types of cysts:
- Simple ones occur in the vast majority of cases. They have a smooth, thin wall, they are regular in shape and filled with a transparent, homogeneous liquid. They do not contain any inclusions and are always benign. The presence of simple breast cysts does not increase the risk of breast cancer!
Simple cysts do not require treatment (you are a healthy woman), except in situations where the cyst is large (2 cm or more) and causes severe pain and discomfort. Then the cyst is punctured and emptied, this is the whole therapy. No dietary supplements, no medications.
- Complex cysts have irregular/uneven contours, they have a thick wall that shows signs of blood flow, and their contents may be heterogeneous and contain various inclusions.
Complex cysts require special attention and almost always aspiration of its contents or biopsy to exclude breast cancer .
- Complicated cysts (in the literature complicated cysts). They are sort of between simple and complex and have most of the characteristics of simple cysts (a thin wall of a regular shape, there is no blood flow in it, etc.), but their contents are heterogeneous and may contain inclusions.
The risk of breast cancer with a complicated cyst is only 2%; such cysts are punctured, their contents are examined and then observed (ultrasound every 6–12 months for 1–2 years).
Please note that nowhere is there any talk about treatment of breast cysts, but only about additional examination to exclude breast cancer.

Diagnostics
Photo: mastopatiya.su
The appearance of cysts in the mammary gland is a very common occurrence for women over 30 years of age. According to statistics, more than 30% of women have ever encountered this problem. These statistics do not take into account those women who have cysts in the mammary glands and do not know about it, since the disease can be asymptomatic throughout their lives.
A cyst in the mammary gland cannot always be diagnosed in a timely manner, since with small tumors it does not manifest itself in any way. In order not to miss the onset of the development of cysts, women at risk after 30 years of age are recommended to undergo an annual examination by a mammologist, who examines the breasts for the presence of tumors. If any signs of a breast cyst appear, it is necessary to initiate a visit to a mammologist earlier than expected. This will help to immediately detect the cyst and begin treatment.
Unfortunately, not all women of the appropriate age follow this important recommendation. In some cases, a tumor or cyst diagnosed in time can be cured, thereby avoiding adverse consequences. The most dangerous complication of a cyst can be a cancerous tumor (if there are oncologically active cells in the contents of the cyst). Timely diagnosis will help determine their presence and remove them, preventing the development of cancer.
Diagnosis of a breast cyst includes the following steps:
- At the first stage of diagnosing a cyst, an examination by a mammologist and palpation of the breast cyst are performed. By palpating the breast, you can find lumps that indicate the presence of tumors, possibly cysts. If a breast cyst is detected, further research will help confirm this diagnosis. If there are serious symptoms accompanied by pain, diagnosing cysts will not cause problems.
- To find out what caused the lumps, an ultrasound of the mammary glands is performed. Cysts will be immediately visible on ultrasound, and you can find out their size and number. No special preparation is required for ultrasound examination. Usually you are asked to bring a disposable diaper and a napkin or towel to remove any remaining lubricating gel from the breast.
- After an ultrasound, a puncture of the breast cyst is often performed. During this study, the contents are removed for cytological examination using a long thin needle. This type of study involves examining cells for cancer markers. Thus, puncture of the cyst is necessary in order to exclude the development of a breast cancer tumor. This study involves breast cyst fluid and epithelial tissue.
- Breast cyst biopsy is similar to the previous research method, however, it involves not only an invasive method of tissue removal, but also analysis through surgery. In addition to the presence of tumor markers, a biopsy allows you to measure the composition of the cyst. Red blood cells in a breast cyst indicate the presence of an inflammatory process. If no symptoms of inflammation appear, and the cyst is not accompanied by cutting pain and burning, then a sluggish, asymptomatic inflammatory process is occurring.
- To take a picture of the mammary gland and see all the tumors on it, mammography is performed. A breast cyst will be immediately visible on the image, even if it is small. The picture is taken in two projections to assess the volume of the tumor. However, a heterogeneous breast cyst and the size of such a neoplasm cannot be fully assessed without ultrasound.
- Tests for breast cysts are necessary to determine the level of leukocytes and ESR. Thus, it is possible to indirectly assess the nature of the inflammatory process occurring in the mammary gland.
It is not necessary to use all of these tests to detect and evaluate a breast cyst. It is possible to assign only some of the most necessary ones. For example, if mammography results reveal one small cyst, then it is not necessary to conduct an ultrasound examination, since, most likely, it will not provide the necessary information.
So, an annual examination by a mammologist will help to promptly detect any lumps that have appeared in the mammary glands. The presence of such seals serves as a reason for further diagnosis of the breast, which includes palpation, ultrasound, puncture, biopsy, mammography and blood test. A mammologist prescribes only those tests that are necessary to make a correct diagnosis and prescribe further treatment for the disease. And a timely detected cyst will allow this treatment to be simplified and avoid the development of complications.
How to live with a breast cyst
Prevention of breast cysts and ways to minimize associated discomfort:
- A bra of the right size that can support your breasts well without squeezing anything.
- Reduce your caffeine intake or eliminate it altogether. There is no conclusive evidence that can link caffeine to the occurrence of breast cysts, but most women report a decrease in soreness.
- In case of severe pain, painkillers from the NSAID group (paracetamol, ibuprofen, etc.) can be used.
- Evening primrose oil, gamma-linolenic acid, and omega-6 unsaturated fats may ease breast tenderness during the menstrual cycle.
- Stop smoking and maintain ideal body weight. Overweight and obesity increase the risk of not only breast cysts, but also breast cancer.
- Avoiding stress, moderate physical activity and a balanced diet with plenty of vegetables and fruits.
Treatment
Photo: medcentr-diana-spb.ru
Therapeutic tactics depend on the characteristics of the woman’s education, age and health. The presence of factors that can improve or worsen the current situation is taken into account. For cysts with a low risk of malignancy, conservative therapy is indicated. If conservative measures are ineffective, multiple large formations, or a high risk of malignancy, minimally invasive intervention (sclerotherapy) or open surgery (sectoral resection, mastectomy) is recommended.
Conservative therapy
A cyst is a benign formation that rarely degenerates into malignant. However, it must be taken into account that the mammary gland is an organ with an increased risk of developing oncological processes. If the formations in the breast are small and do not pose a danger, the following comprehensive treatment is prescribed:
- drugs that normalize the activity of the thyroid gland and ovaries - this helps eliminate hormonal imbalances, which may cause the appearance of cysts;
- anti-inflammatory drugs;
- medications with immunomodulatory effects;
- decongestants and painkillers to eliminate the main symptoms of the disease;
- resorption therapy.
Along with drug treatment, a good effect is observed when using physiotherapeutic techniques: medicinal electrophoresis, magnetic therapy, laser therapy. During the treatment period, the doctor periodically prescribes breast examinations. In this way, the dynamics of the process are determined. It is important to understand how effective the therapy was. If the cysts have enlarged, most often a decision is made to undergo surgery.
Sclerosis of breast cyst
This treatment method is an excellent alternative to surgery. When used, the mammary gland is minimally injured and formations are effectively eliminated. The following are considered as indications:
- cysts no larger than 2 cm;
- anechoic formations;
- unilocular cysts.
Contraindications are the presence of hemorrhagic contents, parietal and intracystic growths, inflammation, signs of degeneration according to morphological or cytological examination. Sclerotherapy is performed by a breast surgeon. The procedure includes several stages:
- Under general or local anesthesia and ultrasound guidance, puncture of the tumor is performed through the skin.
- The fluid contents of the cyst are removed by aspiration.
- A special sclerosant is introduced into the cavity, which promotes gluing of the walls of the formation, which reduces the risk of relapse.
The resulting liquid is sent for cytological analysis. The presence or absence of a malignant process in the mammary gland is determined. In the absence of signs of malignancy, a woman should undergo a preventive examination every six months by a mammologist, endocrinologist and gynecologist.
Surgical removal of the cyst
Surgical removal of a cyst in the mammary gland is indicated in the following cases:
- multi-chamber formations;
- detection of atypical cells in a fluid sample, suspicion of malignancy;
- numerous cysts;
- formations with thickened walls;
- growth in the cyst cavity.
Sectoral resection is carried out for single cysts, local neoplasms with signs of malignancy without involving regional lymph nodes and distant organs. In benign processes, the affected area is marked, two semi-oval incisions are made, they are connected with a third incision at the base of the organ, the resulting sector is excised, the soft tissue is sutured and drained.
If there are signs of malignancy, removal of the gland site is supplemented with lymphadenectomy. Mastectomy is indicated only for widespread lesions of the gland, giant cysts. Possible complications of surgical interventions are wound suppuration, hematoma formation, and external deformation.
Prevention of breast cysts
To prevent the development of cysts and other formations in the mammary glands, you must adhere to the following recommendations:
- Choose underwear that fits your size, doesn't pinch, doesn't rub, and supports your breasts well.
- Do not abuse alcoholic beverages or caffeine.
- Stop smoking, as it negatively affects both the condition of the breasts and the body as a whole.
- Try to avoid injury to the breast.
- If possible, minimize the use of hormonal medications. If prescribed by a doctor, follow his instructions completely and do not change the dosage, either down or up.
- Treat diseases of the genital organs, digestive, nervous and endocrine systems in a timely manner.
- Move enough, limit the amount of fatty and sweet foods in your diet - this will help prevent the development of metabolic syndrome, which contributes to the formation of cysts.
- Regularly undergo preventive examinations with a mammologist.
Local dilatation of the mammary ducts
First you need to understand that the width of the mammary gland ducts depends on:
- phases of the cycle (in the second phase the ducts are slightly wider);
- the woman’s condition (during pregnancy and lactation, the ducts are normally dilated);
- localization of the duct: behind the nipple, the ducts expand, forming milky sinuses. Therefore, if the conclusion says “the ducts are dilated behind the nipple to 2–3 mm,” this is the norm.
But sometimes there may be a single duct dilated to 3–5 mm. Is it dangerous?
It all depends on whether there are any structures inside the duct. If the wall of the duct is smooth and thin, and there is no bloody or yellow-orange discharge from the nipple, there is nothing to worry about. This situation needs to be monitored after 6–12 months. If some structure is visible in the duct on ultrasound, if the wall of the duct looks uneven, thickened, and the patient has bloody or bloody discharge from the nipple, this is a reason for a biopsy. In this case, it is important to exclude intraductal papilloma or breast cancer.
Calcifications in breast tissue
These are deposits of calcium salts. On a mammogram they appear as bright white spots and dots of different sizes and shapes. There may be single or multiple calcifications, grouped or scattered diffusely throughout the gland. Calcifications are formed:
- in old fibroadenomas;
- cysts (“calcium milk”, calcified galactocele);
- walls of blood vessels;
- ducts of the mammary gland;
- after injuries and operations (fat necrosis, hematoma);
- in malignant tumors.
Tumor calcifications are very small, located in a limited area, clusters of such calcifications have an irregular shape and uneven edges. Thus, sometimes they require further examination, but most often this is the norm.
Advertising
Rules for disease prevention
- Annual visit to a mammologist, regular mammography or ultrasound of the mammary glands.
- Regular self-examination.
- Taking care of the mammary gland.
- Take COCs only as prescribed and under the supervision of a physician.
- Rejection of bad habits.
- Selecting and wearing the right bra.
CELT clinic specialists will help you choose the appropriate treatment and maintain your health. The latest equipment, advanced techniques, professional doctors - CELT offers complete patient support, from diagnosis to recovery.
Breast fibroadenoma: what is it?
Fibroadenoma is a fairly common benign tumor that consists of several tissue components, the main of which are the fibrous stroma and the elements of the glandular epithelium contained within it. Fibroadenomas appear more often at a young age (from puberty to 40 years).
What does fibroadenoma look like? You can feel a dense round or oval painful or painless formation. Upon examination and palpation, as a rule, it is difficult to say whether it is a fibroadenoma, a cyst, a lobule of the mammary gland, or another tumor.
On mammography, fibroadenoma is a rounded darkening with clear contours. Ultrasound shows an oval hypoechoic (dark gray) formation with clear, even contours. The structure of fibroadenoma may contain calcifications (usually large and isolated).
The reasons for the appearance of fibroadenomas are not fully known; at the moment, it is generally accepted that the main factors predisposing to the occurrence of fibroadenomas are:
- hormonal influences (increased estrogen levels);
- the use of the drug cyclosporine is associated with the occurrence of multiple fibroadenomas (this cytostatic is used in organ transplantation to prevent transplant rejection in the recipient);
- heredity - if the mother had multiple fibroadenomas, her daughters have an increased risk of this pathology.
Typical fibroadenomas do not transform into breast cancer. But there are nuances. The fact is that on ultrasound and mammograms, breast cancer may not differ from fibroadenoma. Therefore, fibroadenomas identified during the study require a biopsy and/or observation.
How is fibroadenoma treated?
For newly diagnosed fibroadenomas, a biopsy is recommended. It is better if it is a core biopsy rather than a fine-needle puncture. In some cases (very small sizes), a biopsy may not be performed.
When the diagnosis of fibroadenoma is established histologically (or cytologically, which is less preferable), the patient is offered the choice of surgical treatment or observation. Surgery is preferable for questionable histological results, for large fibroadenomas (more than 2 cm), if growth of the formation is noted (visually or according to research data). For small fibroadenomas (less than 2 cm), vacuum aspiration biopsy is a good alternative to surgery.
If it is decided to choose observation as a tactic, then follow-up examinations and studies are usually carried out at intervals of 3-6-12 months (the frequency is determined by the attending physician). When planning a pregnancy in the near future, management tactics are carefully discussed with the patient, since fibroadenoma during pregnancy can increase in size and be complicated by hemorrhages inside the tumor. Therefore, in such cases, it is recommended to remove fibroadenoma larger than 1.5–2 cm.
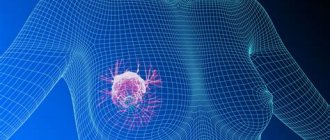
Ultrasound scan for suspected malignant tumors
The reliability of ultrasound in the diagnosis of malignant neoplasms reaches 95% (without specifying the nosological form). When the tumor diameter is more than 5 cm, the accuracy reaches 100%, and less than 2 cm - 63%.
Main ultrasound signs of carcinoma:
- “blurred” uneven contours;
- heterogeneity;
- low echogenicity;
- blurred anterior wall;
- lack of visualization or low echogenicity of the posterior wall;
- presence of dorsal echo.
Scirrhous carcinoma, which occurs in 34% of patients, appears on scans as an irregularly shaped heterogeneous formation with uneven contours. A typical symptom is a dorsal acoustic shadow. Difficulties in differential diagnosis are caused by solid and medullary carcinomas, since they have ultrasound signs characteristic of benign neoplasms.
Due to the similarity of the ultrasound picture, differentiation of many pathologies can be difficult. In doubtful situations, the doctor should recommend mammography. There is a widespread opinion among experts that when diagnosing cystic diseases, the informativeness of ultrasound reaches 100%, and in the presence of small, up to 1 cm, tumors, preference should be given to X-ray examination. The latter is also indicated for studying abnormal areas during fatty degeneration of the gland. At the same time, mammography is not recommended for females under 35 years of age and pregnant women.