Prostate volume calculation
Urologists usually use a universal formula to calculate the volume of the gland.
It looks like this: patient’s age x 0.13 + 16.4, where 0.13 and 16.4 are special coefficients that reflect normal indicators. Thus, it is possible to determine the normal volume of the gland for any age. The main reasons for the increase in prostate volume are:
- Age-related restructuring of parenchyma cells with weakening of their functions;
- General health;
- Lifestyle;
- Hereditary factors.
In itself, a slightly increased size and volume of an organ may not mean anything. Only the clinical manifestations of this transformation become critical for health:
- Difficulty urinating;
- Increased nocturnal diuresis;
- Pain in the groin;
- Weakened erection.
Ultrasound of the prostate gland and other types of research (for example, analysis of the level of free PSA in the blood) are aimed at differentiating the usual functional failure of the organ from its beginning organic degeneration.
Prostate hyperplasia
Benign prostatic hyperplasia is the formation of the planing structure of the organ from the glandular epithelium. This disease in most cases is detected in older men, after 55-65 years. In 80 percent of all cases, hyperplasia affects the prostate organ of a man after 75-80 years.
BPH is described by the appearance of a benign lesion that stops metastasizing. In this case, a characteristic nodule of small diameter appears on the tissue, which over time begins to significantly increase in size, which compresses the urinary canal. Hyperplastic tissue begins to actively spread to the intestines and bladder.
The main causes of this disease include:
- disruptions in hormone production;
- attachment to bad habits;
- irregular sexual intercourse;
- age-related changes in the human body;
- stagnation of arterial and venous blood in the pelvis;
- emotional experiences, severe stress and nervous breakdowns;
- infections, inflammation processes in the genitourinary tract.
If a patient is diagnosed with BPH, he may feel significant discomfort, pain in the lower back, as well as the lower abdomen, painful urination, difficulties in erectile function, fatigue and malaise. Typically, the patient consults a doctor only after the prostate has significantly increased in size.
There are three main stages of disease development:
- First stage. The total volume of the gland increases to 37-45 cubic centimeters. If a specialist detects a prostate size of 40 to 42 mm, this means initial damage to the disease. With this form, the symptoms are almost invisible, the man may feel slight discomfort.
- At the second stage of the lesion, the total volume of the prostate reaches 56 cubic centimeters. The main symptoms of the disease: frequent urination, pain syndromes in the lower part of the peritoneum and severe discomfort.
- The third stage of damage leads to a strong increase in the size of the organ. The volume of the prostate ranges from 65 to 100 cubic centimeters. The patient may have bleeding, strange discharge from the anus, prolonged constipation, and pain during bowel movements. As a result, the outflow of lymph leads to disruption in the regional lymph nodes, and the patient’s lower extremities swell.
Very often, prostate adenoma is detected at the last stage of development, which threatens the emergence of diseases dangerous to health. For example, a benign tumor with prostate hyperplasia can become malignant. It is for this reason that a man after 40 years of age is obliged to undergo a preventive examination once a year, monitor his health and begin treatment on time.
Normal by age
The size of the prostate gland will also depend on the age of the patient. The normal average volume of the prostate gland for a man over 20 years of age is about 25 cubic centimeters. However, after the age of 40, a man experiences a second stage of prostate growth, during which the organ gradually begins to increase in size. The normal size of the prostate in a 60-year-old man is 30 cubic centimeters. These indicators may vary depending on the physique, height, and other characteristics of the man’s body. The norm of the prostate gland, or rather the volume of this organ by age, is presented below:
- From 19.6 to 24.3 cm3 - for boys from 15 to 20 years old.
- From 20.8 to 25 cm3 - for guys from 20 to 30 years old.
- From 21.3 to 26 cm3 - for men from 30 to 40 years old.
- From 23.3 to 28.1 cm3 - for representatives of the stronger sex from 40 to 60 years old.
- From 25.6 to 30 cm3 - for older men from 60 to 70 years old.
Methods for determining pancreas size
Today, there are many ways to determine the size of the prostate gland, including the use of computer technology and scanning, each of which is relevant in its own way. For example, a simple preventative examination of a patient does not necessarily require the use of advanced technologies. Old proven procedures allow us to conclude that the prostate volume is normal.
Identification of deviations in size will be the reason for a more in-depth analysis of the phenomenon, which is all the more true with the potential need for future surgical intervention in the gland area.
A summary list of methods used today is as follows:
- palpation is the first known method for assessing the size of the prostate gland, which is still widely practiced today. It involves placing the patient in a specific (oblique or bent) position, during which the doctor inserts a finger transrectally and feels the prostate gland through the wall of the rectum, assessing its size and density. Disadvantage of the procedure: pain and discomfort to the patient;
- MRI is the use of a high-precision tomograph to obtain a three-dimensional digital image of a given area. It is possible to carry out both a standard scan of all pelvic organs and the use of a special transrectal sensor, which increases the accuracy of studying the prostate. For greater accuracy, intravenous administration of a contrast agent is often used;
- Ultrasound is the use of ultrasound to obtain images by scanning transabdominally (that is, externally through the abdominal wall). The technique is considered somewhat outdated and not very accurate when examining such a small organ as the prostate, but it is cheaper and easier to perform than MRI;
- TRUS is a more advanced ultrasound examination, the accuracy of which is higher than that of conventional ultrasound due to the transrectal insertion of the sensor. In terms of the accuracy of the result and the cost of performing TRUS, it can be considered a compromise between conventional ultrasound and MRI. The disadvantages include discomfort, which, however, is lower than with palpation;
- Prostatography is a less common technique that involves the perineal or transrectal administration of an iodine-based contrast agent, followed by obtaining an X-ray image of increased volume and clarity. The disadvantage of the procedure is its short duration: the contrast agent is quickly absorbed;
- CT is another way to obtain a digital image of the prostate gland without irradiating the patient, not very expensive and with a small number of contraindications and side effects. Another advantage of the procedure is the greater prevalence of computed tomography scans compared to magnetic resonance imaging.
If possible, a urologist or andrologist will always recommend the most accurate method of examination, subject to the financial capabilities of the patient and the availability of appropriate equipment. The final choice remains with the patient, but it is worth remembering that measuring the size of the prostate gland is not the only diagnostic method for assessing its functionality.
What diseases are hidden behind an increase in the permissible size of the prostate?

Prostatitis is an acute or chronic inflammatory process of infectious or non-infectious origin, which is accompanied by the following symptoms: pain in the pelvic area, reproductive dysfunction, increased organ size, problems with urination. From the editor: Prostate adenoma in men: symptoms, treatment, reviews, diagnosis, traditional medicine recipes
Prostatitis can develop against the background of microbial damage to soft tissues, physical inactivity, venous stagnation, hypothermia or irregular sexual activity. If the disease is not diagnosed and treated in time, prostatitis can spread to the kidneys and significantly impair their function, as well as cause impotence and infertility.
Prostate adenoma is a benign tumor in which the size of the organ increases several times. The disease leads to impaired urinary function and deterioration of erection.
Adenoma occurs against the background of hormonal imbalance and age-related changes in the thickness of the prostate. It is accompanied by intense pain and the appearance of symptoms of acute dysuria. If the disease is not treated, the gland will continue to increase in size and worsen the patient's general condition.
A prostate cyst is a rare disease that is accompanied by the formation of a formation with serous content in the thickness of the organ.
As a result of the growth of the cyst, the gland becomes enlarged. The cyst causes dysuria, reproductive dysfunction, and pain in the lower abdomen. Treatment of the formation should be surgical.
Enlargement of the prostate may be associated with the formation of stones in its thickness. This is a rather painful process, which is accompanied by the appearance of blood in the urine and ejaculate, and also leads to infertility. Prostate cancer is the most dangerous disease of the organ, occurring for a variety of reasons, including a hereditary predisposition to malignant transformation, bad habits, and eating poor-quality foods.
As the tumor increases, patients begin to complain of pain in the perineum, swelling of the extremities, impaired urine flow, and the appearance of blood in the urine.
Cancer treatment tactics depend on the stage of the disease and the presence of metastases. Such patients are indicated for chemotherapy, as well as radical surgery to remove the prostate gland.
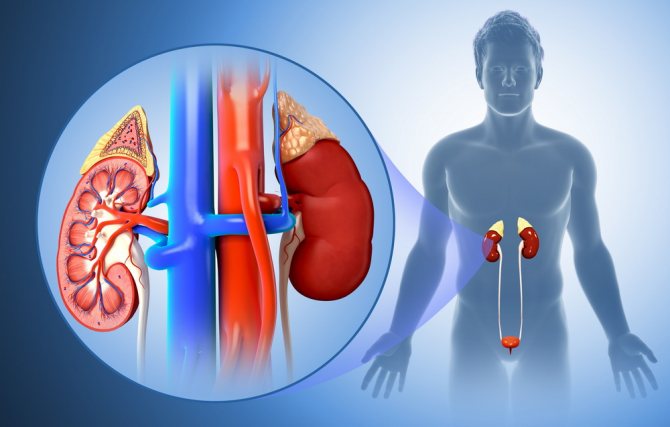
Structure and functions of the prostate gland
The prostate gland is the most important endocrine organ of the male genitourinary system.
Impaired functioning of the prostate leads to a deterioration in sexual life and weakened reproductive health.
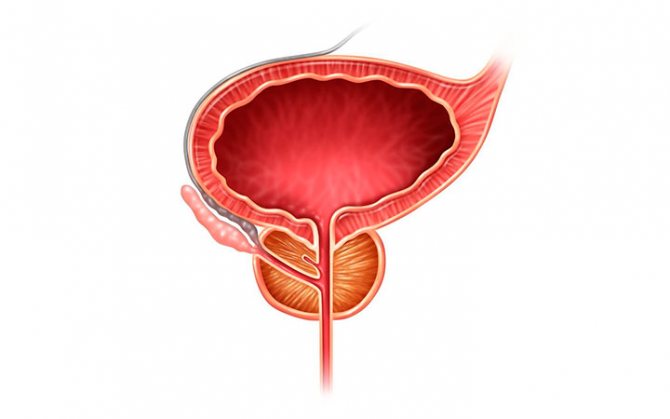
The prostate is an internal secretion organ formed by two lobes connected by a thin strip of tissue.
The gland is a complex alveolar-tubular organ, has an elastic and dense structure, and is trapezoidal in shape.
The ducts of the gland exit into the urethra. The back wall of the prostate is adjacent to the intestine, so the doctor can easily feel the gland by entering the patient’s rectum with his fingers.
The main function of the organ is the synthesis of a secretion that dilutes sperm. The secretion contains vitamins, enzymes, antibodies, and microelements.
The gland also closes the urethra during erection. The activity of the prostate is regulated by hormones secreted by the pituitary gland.
The prostate is a capricious organ; in men 40–60 years old it causes many problems. Prostate volume changes throughout life and is determined by numerous external and internal factors.
The size of the prostate gland is usually determined by the man’s age, hormonal levels, and the general condition of the body. In men over 50 years of age, the tissue connecting the lobes of the prostate begins to grow, gradually squeezing the bladder and urethra. This painful phenomenon is called prostate adenoma.
Prostate structure
It is very important, when determining the normal size of the prostate gland using ultrasound, to also evaluate its structure. The prostate consists of 30-50 lobules with excretory ducts. Normally, its structure is symmetrical, and during palpation the doctor can clearly palpate two symmetrical halves, which are separated by a groove. The structure of a healthy gland according to ultrasound is homogeneous, without any inclusions, calcifications, tumors and cysts.
If a pathological inclusion is detected, the doctor prescribes a more thorough examination - a biopsy to examine the cellular structure. This will eliminate the risk of degeneration into a malignant tumor.
Prostate location and size
The prostate gland is located in the lower part of the pelvis just below the bladder, on the urogenital diaphragm. The prostate is a hormone-dependent organ that can change throughout life.
During puberty, this organ begins to rapidly increase in size, and by the age of 25 it reaches normal size. After 45 years, the prostate gland goes through stage 2 of growth and begins to increase even more.
A slight increase may be normal. Pathological growth is considered the first signal of the occurrence of benign prostatic hyperplasia.
Normal sizes
In the absence of pathologies, the contour of the prostate should have a clear and even appearance.
When scanning transversely, normal values are from 1.6 to 2.5 cm in thickness, and from 2.7 to 4.2 cm in width.
The normal length of the prostate is from 2.4 to 4.1 centimeters.
Volume and weight of the gland
Having determined all linear dimensions, qualified specialists can correctly calculate the volume and weight of the gland.
To do this, you need to multiply the thickness, width and length, multiplying the coefficient, which takes into account the shape of the organ. The resulting figure should not be more than 26 cm³. the maximum allowed value is 30.
All indicators directly depend on the patient’s age category, general health, body structure, genetic predisposition and many other facts.
The main difference between a normal prostate size and a pathological manifestation is the complete absence of symptoms.
Gland structure
In addition to linear and volumetric indicators, it is also quite important to determine the structure of the affected organ. The normal structure varies from 30 to 50 lobules, which are what the excretory ducts have
The structure of the prostate gland must be symmetrical, and when palpating the rectum, the specialist must clearly identify two identical halves, which are separated by a certain groove.
The structure of the gland should exclude inclusions and have a uniform appearance; therefore, no neoplasms or cysts should be detected.
Determining the size of the gland
Determining the size of the gland can occur in several ways.
- Manual examination performed by a urologist.
- Ultrasonography. Using ultrasound waves, you can achieve accuracy in determining the volume, size and weight of the prostate.
- Prostography is used extremely rarely and requires preliminary preparation of the patient. Using a contrast liquid, the required organ is stained.
In order to promptly identify any neoplasm that has arisen, a man must undergo a routine examination by a specialist once a year. By identifying the disease in the early stages, the possibility of a complete cure increases significantly.
Pathologies characterized by enlarged pancreas
Modern medicine does not yet provide a clear answer to the question of the causes of abnormal prostate enlargement. Thanks to the research, scientists were able to accurately establish one of the risk factors - testicular function. In men with testicles removed, the prostate does not enlarge.
All other reasons are somehow related to age. Among them:
- natural age-related decrease in testosterone levels and an increase in the proportion of estrogen in the blood;
- increasing the proportion of dihydrotestosterone, a hormone produced by the pancreas. In older men, it continues to be produced in the same volume and accumulates in the prostate, which leads to its growth;
- hereditary factors. A genetically based program can activate lifespan growth after 60 years (but this is still only a scientific hypothesis).
From the editor: "Vilprafen" for prostatitis: composition, instructions for use, indications and contraindications
An enlarged prostate primarily affects the quality of life. A man sleeps poorly at night, is constantly tied to the toilet, cannot afford long trips, etc. Adenoma and prostatitis are the most common diseases in which prostate tissue grows.
Prostate adenoma (benign hyperplasia)
This disease develops in approximately 50 percent of men over 60 years of age and in almost all after 80. It is accompanied by urinary problems and can cause the formation of a malignant tumor. With hyperplasia, nodular neoplasms appear, the prostate grows either towards the rectum or into the bladder area (with penetration).
The disease goes through three stages of development:
- Compensated. Characterized by frequent urge to urinate, especially at night (up to 10 times). Can last 8-10 years.
- Subcompensated. Accompanied by pain when urinating, intermittency and weakness of the stream, and urinary retention.
- Decompensated. Patients experience significant deterioration in condition, thirst, nausea, and weakness. The functioning of the kidneys and gastrointestinal tract is disrupted. It becomes more and more difficult to urinate; I have to use a urine bag.
At stages 1 and 2, drug treatment is carried out using drugs:
- normalizing hormonal metabolism and helping to reduce pancreas;
- affecting the tone of the prostate and urethra, facilitating urination.
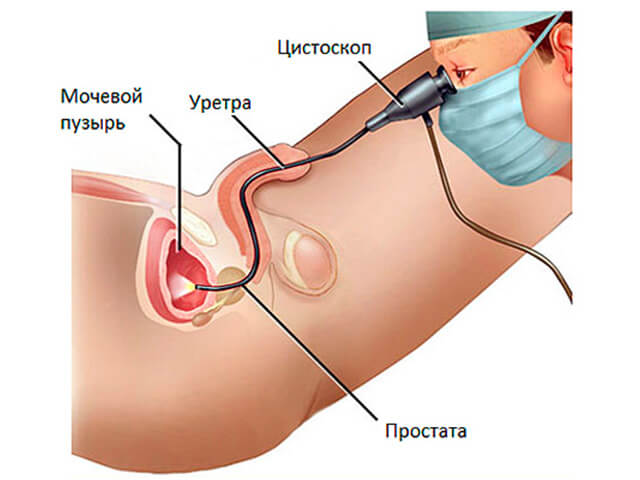
In severe cases of adenoma, surgical intervention is required. Transurethral resection of the prostate gland is considered the most effective method today. During the operation, a special device, a resectoscope, is inserted into the urethra to remove pathological tissue. This is a minimally invasive endoscopic procedure with minimal risk of complications and a relatively short recovery period.
Prostatitis
Prostatitis is an inflammation of the pancreas that occurs due to frequent hypothermia, a sedentary lifestyle, infection, and excess weight. It can develop as a complication of tuberculosis, tonsillitis, influenza and lead to a doubling of the prostate.
Symptoms of acute prostatitis:
- temperature increase;
- frequent urge and sharp pain when urinating;
- sexual dysfunction;
- pain during defecation.
Signs of a chronic form of the disease:
- nervous disorders;
- pain in the perineum;
- discomfort in the groin and pubic area;
- discharge in the form of white flakes;
- erectile disfunction.
The treatment method for prostatitis is selected taking into account the form and course of the disease. The standard course includes hormone therapy, antibiotics, alpha blockers, herbal medicines and physiotherapeutic procedures to help relieve pain and eliminate discomfort.
Prostate functions
The structure of the prostate is such that it flows around the urinary tract with its muscular membrane, therefore, with swelling and inflammation, problems with urine excretion begin, which leads to stagnation and infections. The back of the prostate can be felt when palpated through the anus; it has a very elastic wall.
Functions of the prostate gland:
- the prostate affects the quality of sperm - the reproductive function of men;
- it affects pleasure during sexual intercourse;
- the prostate separates the processes of urination and ejaculation so that they do not mix with each other;
- the prostate gland produces testosterone;
- protects sperm from infection from the ureters.
Therefore, for a man to catch prostate diseases, it is very painful physically, mentally, and the inability to satisfy in bed hits a man’s pride.
Therapeutic measures
Based on the results of all necessary tests, the stage of the disease and the clinical manifestations of prostate adenoma, the doctor, together with the patient, selects the appropriate therapeutic tactics.
There are several treatment regimens for patients with prostate adenoma:
- Monitoring the dynamics of the disease, conservative medicine.
- Drug therapy.
- Surgical intervention.
Conservative treatment of prostate adenoma includes adjustments to lifestyle and daily routine. The doctor selects an individual set of physical exercises; you can use herbal preparations to improve blood circulation in the hip area. In the early stages of the development of the disease, when the gland is slightly enlarged, folk remedies such as a decoction of nettle leaves and rhizomes, pumpkin seeds, and medicinal baths can help stop the growth of prostate adenoma and alleviate its symptoms.
Nettle decoction is taken at stages I and II of glandular adenoma. To prepare it you need to take 1 tbsp. l of raw materials and pour a glass of hot water, boil for 5 minutes, strain. Take 200 ml of decoction in the morning and evening. The course of treatment is one month.
Considering that the prostate is an androgen-dependent gland, when it enlarges, low testosterone levels are often recorded. Pumpkin seeds contain a lot of zinc and other trace elements that contribute to the rapid restoration of the hormone. To satisfy the body's daily need for zinc, it is enough to eat half a glass of unroasted pumpkin seeds daily.
Sitz baths will have an anti-inflammatory and decongestant effect on the diseased gland. For these purposes, pharmaceutical preparations from chamomile flowers, oak bark, sage or marsh cudweed are suitable. Take a bath for at least 10 minutes, but no more than an hour.
It is worth noting that it is possible to treat prostate adenoma with traditional methods in situations where an increase in the size of the gland has been recently discovered, and in the absence of disturbing symptoms. If the volume of the prostate is more than 40 cm³, then it is better to turn to official medicine.
Nettle decoction is used as an adjuvant treatment in the initial stages of the disease.
Typically, prostate adenoma is treated with alpha-blockers and 5-alpha-reductase inhibitors. Unlike inhibitors, the effect of which is noticeable only after 3-6 months, alpha-blockers begin to act from the first days of use. However, this feature causes adverse reactions of the body to the drug: dizziness, headache, severe tachycardia, dyspeptic symptoms. Also, adrenergic blockers slow down the enlargement of the gland, but do not stop its growth. 5-alpha reductase inhibitors are used to reduce prostate volume and before surgical procedures.
Abdominal surgery is used to treat large prostate adenomas. Due to the widespread use of diagnostic methods and good awareness among men about sexual health and the symptoms of this disorder, doctors are increasingly less likely to encounter advanced stages of adenoma. Therefore, for pathological enlargement of the prostate, the “gold standard” is transurethral resection. The source of inflammation is removed using a resectoscope, which leads to normalization of the volume of the gland.
Prostate adenoma can significantly worsen a man’s quality of life. Fortunately, many years of experience in treating genitourinary diseases is a guarantee of a successful and effective solution to this problem. Be healthy!
Source egopik.ru
Prostate adenoma is a disease in which a benign tumor develops in the prostate gland. In medicine, this disease is called benign prostatic hyperplasia (BPH).
Multiplane sonography of the prostate: an additional diagnostic method for routine examination

Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Introduction
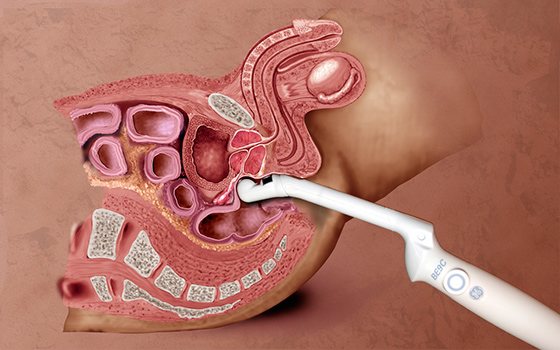
The medical application of the piezoelectric effect, discovered in 1880 by Jacques and Pierre Curie, began in the late 1940s as a further development of the method applied to ocean geology and military needs. The advent of computers led to the rapid introduction of ultrasound into medicine. The success of the use of ultrasound in medicine and the expansion of areas of application are explained by the fact that it is a non-invasive, non-ionizing radiation and inexpensive diagnostic method. A major role in the development of ultrasound examination of the prostate gland belongs to N. Watanabe and co-authors, who in the early 1970s introduced the use of an intracavitary transducer for examining the prostate [1-3]. Currently, transrectal sonography is a routine method to assess the morphology of the prostate gland, its structure and volume; this is the first level of research in clinical urology [4]. Transrectal ultrasound has improved the yield of prostate biopsies by accurately mapping the prostate gland [5,6]. However, the lack of sensitivity of the method needs to be discussed.
The sensitivity of this method is operator dependent and may be limited by technical factors such as the size and location of the lesion [7,8]. In addition, it has been shown that not every centrally located lesion identified by sonography is a neoplasm, and the symmetry and regularity of the contours of the gland are important additional diagnostic information. The diagnosis of prostate neoplasm should always be confirmed by biopsy. Ultrasound can be used to biopsy lesions that are not posterior and therefore not palpable on rectal examination. Transrectal sonography can detect suspicious areas within the prostate, which are primarily hypoechoic and malignant in 17–57% of cases [9].
Prostate specific antigen was discovered in 1979 and is now essential for the diagnosis and control of prostate cancer [10–17]. The feasibility of determining prostate-specific antigen at an early stage of prostate cancer is debatable, since prostate-specific antigen is not specific for prostate cancer, but is a product of normal and hyperplastic prostate tissue. Therefore, PSA has low sensitivity as a screening test for prostate cancer. PSA derivatives should improve its diagnostic value [18]. It is known that the correlation of PSA values with prostate and tumor volume increases the diagnostic and prognostic value of this study [19, 20].
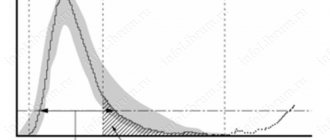
2D sonography does not accurately measure volume. Currently, there are two methods for calculating prostate volume. The first one calculates the volume using the ellipse formula; it has an average error of 20% [21]. The calculation of the volume of the prostate gland by the second method is made by summing the selected areas of the gland obtained at 5-mm intervals. This measurement method is extremely time-consuming, non-repetitive, and inconvenient for the patient. 2D sonography has limited capabilities compared to other technologies such as computed tomography (CT), nuclear magnetic resonance (NMR), and positron emission tomography (PET), which use three-dimensional imaging techniques. The purpose of our work is to evaluate the use of three-dimensional (3D) ultrasound imaging for routine examination of the prostate gland.
Materials and methods
For the study, a modern ultrasound device with a 7.5 MHz volumetric intracavitary sensor was used (Fig. 1). The first step was to select the area of volumetric reconstruction of the prostate gland, then the converter automatically took a series of sequential scans (from 50 to 256) in the selected volume. It took 5-20 s to obtain a three-dimensional image. Images appeared on the screen in three orthogonal planes: longitudinal, transverse and frontal (Fig. 2). By dissecting the test volume layer by layer, it is possible to obtain an image in any plane, which allows for the best assessment of the anatomical details of the prostate gland, especially in the frontal plane (Fig. 3). All information was stored in the device’s memory on a hard drive, which made it possible to evaluate both two-dimensional and three-dimensional images even without the presence of the patient. In addition, this method is easy to repeat and is well tolerated by patients.
Rice. 1.
Endorectal volumetric sensor 7.5 MHz.
Rice. 2.
Multiplane image of the prostate gland: A - transition zone; B - central zone; C—peripheral zone.
Rice. 3.
Prostate gland in the frontal plane. Clear visualization of the transition zone and pseudocapsule: A - transition zone; B - well-defined pseudocapsule; C - apex; D - urethra.
An ultrasound scanner equipped with a three-dimensional vision system allows you to use volumetric information to obtain images in various modes - superficial and transparent (maximum and minimum). Surface mode imaging is of little assistance in imaging the prostate gland because the prostate, unlike the embryo surrounded by amniotic fluid, does not have a highly reflective ultrasound beam interface. In this case, you can use a transparent image, in which the computer transforms the gray scale into different levels of transparency, allowing you to look inside the volume, while increasing the contrast between hyperechoic and anechoic areas. This mode can provide 3D morphological visualization of hypoechoic areas. Based on our experience, we can say that such an assessment of the prostate gland is crude and has no diagnostic value.
Recently, a system was introduced for automatically calculating the volume of the zone of greatest interest selected by the operator - VOCALTM (Fig. 4). For example, by determining the boundaries between a prostate adenoma and its surrounding tissues, using a computer, you can select an area of interest and automatically calculate its volume [28]. To optimize the automatic volume calculation, you can manually adjust the contour of the area defined by the computer in different scanning planes.
Rice. 4.
Automatic calculation of prostate volume. Multiplane scans and a volumetric phantom created as a result of 3D reconstruction.
From January 1998 to June 1999 75 patients aged 58-75 years were studied for dysuria, hematuria, increased prostate specific antigen values, changes detected during rectal examination, or in the case of a combination of various causes. Thirty-two of them had tumors, most of which had been previously diagnosed, and the patients were awaiting radical prostatectomy. In 25 out of 43 patients with benign prostatic hypertrophy, adenomectomy was performed through a suprapubic approach. Other patients received drug treatment with finasteride.
The volumes of prostate adenomas and tumors were calculated by summing them at regular, predetermined intervals. Calculation areas were manually selected on each scan. After this, it became possible to estimate the volume automatically using the VOCALTM program, and the results coincided with the previously obtained data. Volumes obtained from 25 adenomas and 19 tumors were compared with volumes obtained from surgical procedures. Patients with benign prostatic hypertrophy who received drug treatment were examined again after 3 and 6 months. Volumes obtained in three consecutive studies were compared.
Research results
Three-dimensional sonography of the prostate gland allows an accurate assessment of all dimensions of the prostate gland, including the volume of adenoma and malignant tumors [29-39]. The results we obtained regarding the volumes of adenomas and tumor volumes in different groups of patients differed slightly from the actual ones. In 25 cases of transabdominal adenomectomies with adenoma volumes greater than 40 cm³, errors in volume assessment were 1-7%. This may be due to the morphological structure of adenomas, which are not always homogeneous. The error also depends on the common third lobe of the prostate gland (Fig. 5). The error was smaller for small adenomas and in the absence of the third lobe. As expected, large, heterogeneous adenomas produced significant measurement errors.
Rice. 5.
Scheme of the prostate gland: sagittal scan demonstrating the calculation of volume using the ellipse formula: P - prostate gland; ML - medial lobe; UB—urinary bladder; SV - seminal vesicle.
Adenomas were divided into three groups depending on volume: 40-60, 61-80 cm³ and more than 81 cm³. In 8 cases with adenoma volumes of 40-60 cm³, the average error was 2.7%, taking into account that in 2 cases out of 8 observations hypertrophy of the third lobe was noted. In 13 cases of adenoma with a volume of 61-80 cm³, the average error was 3.9%. Among 4 patients with an adenoma larger than 81 ml, the average error was 5.2%. In one of these four cases the error was less than 1%, while in two observations it was 6.5 and 7% (table).
Table
. Measuring the volume of adenomas and tumors using the VOCALTM program.
| Number of cases | Volume, cm³ | Average error, % | |
| Adenoma | 8 | 40-60 | 2,7 |
| 13 | 61-80 | 3,9 | |
| 4 | >81 | 5,2 | |
| Tumor | 15 | 1-3 | 2 |
| 2 | 3-7 | 5 | |
| 2 | >7,1 | 11,5 |
18 patients with adenoma who were treated with finasteride were examined 3 and 6 months after the start of therapy. The volume of these adenomas ranged from 41 to 70 cm³. Medical treatment was preferred over surgery either due to lack of disease symptoms or due to patient preference. In each of these cases, volume calculations from 3D sonography demonstrated a reduction in adenoma volumes of 9% to 21%, with larger adenomas shrinking more than small ones. The greatest reduction in prostate volume was observed after 3 months, then the reduction was less significant.
In 19 of 32 patients with malignant tumors who underwent radical prostatectomy, the pathological calculation of volume coincided with the results of volume measurements by three-dimensional sonography. In 15 cases of tumors located at the posterior surface, with a volume of 1-3 cm³, sonographic and real volumes were almost identical with an error of approximately 2% (Fig. 6). This can be explained by the small size of the tumors and their hypoechogenicity relative to the surrounding tissues at the posterior surface of the prostate gland, which clearly delineated the edges of the tumor on echograms. This may also be explained by the fact that small tumors have a typical growth pattern, resulting in compression of surrounding tissues and resulting in clearer echographic recognition of tumor margins. Large tumors have less clear boundaries separating them from surrounding tissues, possibly due to the infiltrative nature of growth. Therefore, for tumors with a volume of 3-7 cm³, sonography gives an error of 3-7%. Tumor volumes greater than 7 cm³ give an error of more than 10%. This increase in measurement error is associated with difficulties in delineating the lesion, especially in those areas where the tumor is not located at the posterior surface of the gland, but invades the transition zone or has infiltrative growth into the capsule (Fig. 7, 8). It is important to understand that volume calculations are limited by the ability of ultrasound to “recognize” tumors among normal gland tissue. In 6 cases where there was a large error in volume calculation, the pathologist found multifocal tumors that could not be accurately measured due to diffuse tumor infiltration.
Rice. 6.
Automatic calculation of the volume of prostate tumor located at the posterior surface.
Rice. 7.
Automatic calculation of prostate tumor volume at the posterior surface involving the transition zone (arrow). A - image in the frontal plane.
Rice. 8.
Automatic calculation of the volume of prostate tumor located at the anterior surface.
conclusions
In our study, we wanted to evaluate the effectiveness of calculating prostate volume using 3D sonography compared with determination of prostate specific antigen derivatives. This technology provides a rapid and reliable method for assessing prostate volume [37, 40]. The available literature regarding the calculation of prostate volume using the ellipse method reports an error of approximately 20% relative to the actual volume [22]. Previous in vitro and in vivo studies have proven the extreme accuracy of 3D sonography in calculating prostate volume. We correlated these volumes with data obtained from surgery and pathological examination to combine them with prostate-specific antigen calculations. 2D sonography, with a volume measurement error of approximately 20%, cannot be used to assess prostate-specific antigen density. The latter may play a significant role in establishing criteria for selecting patients requiring biopsy, i.e. patients with negative sonography results and prostate specific antigen levels between 4 and 10 mg/ml. Determining the exact volume of the prostate gland and assessing the level of prostate specific antigen can be very useful for developing treatment tactics and monitoring its effectiveness. Clinicians consider prostate tumor volume as an important prognostic factor in assessing tumor aggressiveness. Accurate measurement of tumor volume may be important preoperatively, especially given lymph node involvement. In addition to the exact volume of the prostate gland, the exact volume of the tumor is necessary for therapy and treatment prognosis. In our study, there was good agreement between sonographic prostate volumes and actual volumes, especially when studying adenomas and malignant tumors. The accuracy of volume measurements is extremely high, especially when studying adenomas with a clear distinction between the transition zone and the unchanged part of the prostate gland. In these cases the error is very small.
Tumors up to 3 cm³, limited to the posterior surface of the prostate, with a clear demarcation between the tumor and the surrounding tissue, gave fairly accurate volume measurements. At the same time, it is difficult to identify the edges of a large tumor both during ultrasound and pathological examination due to its infiltrative growth.
The equipment we used made it possible to automatically measure the volume of the prostate gland and provide immediate visualization of the gland on the monitor in three planes: transverse, longitudinal and frontal. The development of this technology makes it possible to truly study the prostate gland in three dimensions, providing better images of the contours, apex and internal structure of the gland. The frontal plane is especially useful for studying the contours of the gland and demonstrating the transition zone, which is poorly defined in the axial and sagittal planes. Reducing the examination time is extremely important for the patient; the transducer is placed in the rectum for a very short time. The ability to save the received information on a hard drive allows you to subsequently reproduce the data with an accurate and detailed study. In addition, the data obtained can be re-examined with colleagues, clarifying the diagnosis.
In our study, we did not compare the diagnostic capabilities of three-dimensional sonography and conventional two-dimensional scanning, but the ability to examine the prostate gland slice by slice, including in the frontal plane, makes it diagnostically significant.
Subsequent studies need to clearly define the significance of volume measurement, but we believe that 3D sonography, as an accurate and reproducible diagnostic method, especially for volume measurement, can become a routine test in the qualitative and quantitative assessment of prostate pathology.
Literature
- Watanabe H, Igari D, Tanahasi Y, Harada K, Saito M. Development and application of new equipment for transrectal ultrasonography. J Clin Ultrasound 1974;2:91.
- Watanabe H. History and applications of transrectal ultrasonography of the prostate. Urol Clin N Am 1989;16:617.
- Strasser H, Janetschek G, Reissigl A, Bartsch G. Prostate zone in three-dimensional transrectal ultrasound. Urology 1996;4:47.
- Aarnink RG, Beerlage HP, Dela Rosette JJM, Debruyne FMJ, Wijkstra H. Transrectal ultraso und of the prostate; innovations and future applications/J. Urol. 1998;159:1568-79.
- Melchior SW, Brawer MK. Role of transrectal ultrasound and prostate biopsy. J Clin Ultrasound 1996;24:463.
- Lee F, TorpxPedersen ST, Siders DB, et al. Transrectal ultrasound in the diagnosis and staging of prostatic carcinoma. Radiology 1989; 170:609.
- Flanigan RC, Catalona WJ, Richie JP, et al. Accuracy of digital rectal examination and transrectal ultrasonography in localizing prostate cancer. J Urol 1994;152:1506-9.
- Hemandez AD, Smith JA Transrectal ultrasound of the early detection and staging of prostate cancer. Urol Clin North Am 1990; 17:745-57.
- Giensen RJB, Huyner AL, Aarnink RG, et al. Computer analysis of transrectal ultrasound images of the prostate for the detection of carcinoma: a prospective study in radical prostatectomy specimens. J Urol 1995; 154:1397.
- Hammerer PG, Mc Neal JE, Stamey TA. Correlation between serum prostate specific antigen levels and the volume of the individual glandular zones of the human prostate. J Urol 1987; 137:686-9.
- Bazinet M, Peloquin F, Meshref AW, et al. Prospective evaluation of prostate-specific antigen density and systematic biopsies early detection of prostatic carcinoma Urology 1994;43:44-51.
- Littrup PJ, Kane RA, Williams CR, et al. Determination of prostate volume with transrectal US for cancer screening: Comparsion with prostatespecific antigen studies. Radiology 1991;178:537-2.
- Bretton PR, Evans WP, Barden JD, Castellanas RD. The use of prostate specific antigen to improve the sensitivity of prostate specific antigen detecting prostate carcinoma cancer Br J Urol 1994;74: 2991-95.
- Brawer MK, Aramburn EAG, Chen GL, Presten SD, Ellis WJ. The disability of prostate specific antigen index to enhance the predictive value of prostate specific antigen in the diagnosis of prostatic carcinoma. J Urol 1993;156:369-73.
- Partin AW, Oesterling JE. The clinical usefulness of prostatic specific antigen: update 1994. J Urol 1994;152:1358.
- Partin AW, Oesterling JE. The clinical usefulness of prostate specific antigen: update 1994. J Urol 1994;152:1358.
- Babaian RJ, Kojima M, Ramirez El, Johnston D. Comparative analysis of prostate specific antigen and its indexes in the detection of prostate cancer. J Urol 1996; 156:432.
- Van Iersel MP, Witjes WPJ, De La Rosette JJMCH, et al. Prostate specific antigen density: correlation with histological diagnosis of prostate cancer, benign hyperplasia and prostatitis. Br J Urol 1995;76:47.
- Kalisk J, Cooner WH, Graham SD. Serum PSA adjusted for volume of transition zone (PSAT) is more accurate than PSA adjusted for total gland volume (PSAD) in detecting adenocarcinoma of the prostate. Urology 1994;43:601-6.
- Benson MC, Whang IS, Pantuck A, et al. Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer. J Urol 1992;147:815-16.
- Jeminow A, Hammer M, Rather P, Hertle L. Prostatic specific antigen corrected for prostate volume improves differentiation of benign prostatic hyperplasia and organ confined prostatic cancer. Br J Urol 1994;73:538-43.
- Kimura A, Kurooka Y, Hirasawa K, Kitamura T, Kawabe K. Accuracy of prostatic volume calculation in transrectal ultrasonography. Int J Urol 1995;2:252-6.
- Kirbach D, Whittingham TA. 3D Ultrasound The Kretztechnic Voluson Approach. Eur J Ultrasound 1994:1:85-9.
- Baba K, Okai T. Real time processable three dimensional fetal ultrasound Lancet 1996;348:1307
- Hohue KH, Fuchs H, Pizer SM. 3D imaging in medicine algorithms systems, application. Berlin: Springer-Verlag, 1990.
- Fishman EK, Magid D, Ney DR, et al. Threedimensional imaging Radiology 1991;181:321-37
- Terns MK, McNeal JE, Stamey TA. Estimation of prostate cancer volume by transrectal ultrasound imaging. J Urol 1992; 147:857-8.
- Hodges TC, Detmer PR, Bums DH, et al. Ultrasonic three-dimensional reconstruction; in vitro and in vivo volume and area measurement. Ultrasound MedBiol 1994;20:719-29.
- Aarnink RG, Huynen AC, Giensen RJ, et al. Automated prostate volume determination with ultrasonographic imaging. J Urol 1995;153:1549-54.
- Tong S, Downey DB, Cardinal HN, Feuster A. Three-dimensional ultrasound prostate imaging system. Ultrasound Med Biol 1996;22:735-46.
- Littrup PJ, Williams CR, Egglin TK, Kane RA. Determination of prostate volume with transrectal US for cancer screening: accuracy of in vitro and in vivo techniques Radiology 1991;179:49-53.
- Elliot TL, Downey DB, Tong S, McLean CA, Feuster A. Accuracy of prostate volume measurements in vitro using three-dimensional ultrasound. AcadRadiol 1996;3:401-6.
- Riccabona M, Nelson TR, Pretorius DPH. Three-dimensional ultrasound: accuracy of distance and volume measurement. Ultrasound Obstet Gynecol 1996;7:429-34.
- Riccabona M, Nelson TR, Pretorius DH, Davidson TE. In vivo three-dimensional sonography measurement of organ volume: validation in the urinary bladder. J Ultrasound Med 1996; 15:627-32.
- Hamper UM, Trapanotto V, Sheth S, Dejong MR, Caskey CI. Three-dimensional US: preliminary clinical experience. Radiology 1994; 191:397-41.
- Sehgal CM, Broderick GA, Whittington R, Gorniock RJ, Arger PH. Three-dimensional ultrasound and volumetric assessment of prostate. Radiology 1994:192:274-8.
- Hamper UM, Trapanotto V, Dejong MR, Sheth S, Caskey CI. Three-dimensional US of the prostate: early experience. Radiology 1999;212:719-23.
- Tewari A, Indudhura R, Shinohara K, Schalow E, Woods M, Lee R, Anderson C, Uarayun P. Comparison of transrectal ultrasound prostatic volume estimation with magnetic resonance imaging volume estimation and surgical specimen weight in patients with benign prostatic hyperplasia. / Clin Ultrasound 1996:24:169-74.
- Collerelli K, Strasser H, Reissigl A, Janetschek G, Bartsch G. Three-dimensional transrectal sonography: staging of prostate cancer. J Urol 1994:150:504.
- Hamper VM, Trapanotto V, Sheth S, Dejong MR, Caskey CI. Three-dimensional ultrasound: preliminary clinical experience. Radiology 1994:191:397-401.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
How the size and condition of the prostate gland is studied
A urologist deals with treatment and preventive examinations of male organs. The first thing this doctor does is take a medical history of the patient, collecting a primary anamnesis. That is, the doctor interviews the patient in detail, records the answers and his assumptions.
The next step is palpation of the prostate gland. Thanks to this study, a good urologist is able to detect even a slight enlargement of the gland. By palpating the organ, the doctor notes whether there is pain, how elastic the tissue is, or whether there are any seals that may indicate a tumor. If the urologist has noted abnormalities, the next step for examination is ultrasound.
The normal size of the prostate gland during ultrasound can be easily distinguished from abnormalities with almost 100% probability. Modern equipment provides a clear enough image to diagnose and clarify most diseases: cysts, tumors, nodules.
From the editor: “Vitaprost” (tablets): reviews, instructions for use
The more specific the structure of the neoplasm, the easier it is for the urologist to make a final diagnosis and begin the correct treatment. A cyst is a cavity formation in the gland that is filled with fluid. Ultrasound is also excellent at diagnosing diseases such as calcifications. These are peculiar stones of oval or round shape. Their size usually does not exceed 200mm.
Before TRUS, you need to properly prepare your bowels. To do this, you can choose either an enema with warm, boiled water, or a microenema. Microclysters are very popular. They are harmless and gently relax the intestines even with severe constipation. Fecal stones dissolve, facilitating the process of defecation.
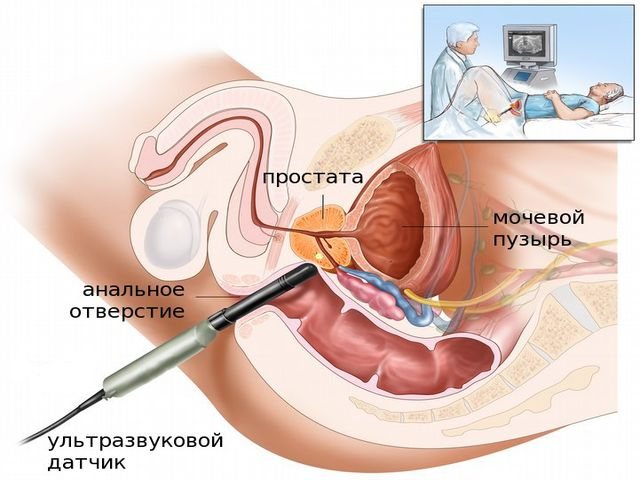
Ultrasound performed through the peritoneum of the lower abdomen does not always give a satisfactory result. For example, a large layer of abdominal fat in obese men is a huge barrier to ultrasound. Another type of ultrasound examination, TRUS, comes to the rescue.
A sensor is inserted into the patient's anus, which allows you to see the organ being examined, literally in the palm of your hand. In the attached video you can see details of how a transrectal ultrasound examination is performed, find out how unpleasant it can be and how you need to prepare before the appointment.
In addition to ultrasound examination, if tumors or malignancies are suspected, the patient undergoes an MRI. This is the most accurate device that allows you to examine the smallest changes in the volume of the prostate gland, which normally should be smaller, but the doctor cannot draw a conclusion based on ultrasound and age standards due to suspicions of cancer or a tumor.
X-rays are used less and less frequently to distinguish between a normal prostate and an enlarged one. This method of studying the size of the prostate gland is called prostatography. Since the gland stands out little in shape, texture and color against the background of other organs located nearby, a simple x-ray of this organ is ineffective.
In order to isolate the prostate, a contrast agent is injected into the empty bladder using a catheter. A healthy organ has a clear, even structure, without irregularities, spots, or neoplasms. If, during prostatography, a heterogeneous structure was identified, the diagnosis will most likely be prostate atrophy. Exceeding the normal volume of the prostate is prostatic hyperplasia.
How to reduce the size of the gland
If a man’s case is not advanced, and it implies the possibility of reducing the prostate without surgery or active medical therapy, then you can try to reduce its size. Reduction of the gland during prostatitis is possible by reducing tissue swelling during inflammation.
When treating adenoma, it should be remembered that it is almost impossible to reduce it with tablets, solutions or folk remedies. But with the help of surgery this is possible.
Laser removal is the most modern method for removing benign tumors in men. It does not take a lot of time, gently burns through unnecessary tissue, and at the same time carries out coagulation of blood vessels.
The transurethral method is a good method in that no unnecessary incisions are made to access the adenoma. There are limitations to the method:
- the mass of the adenoma should not exceed 55 grams;
- the volume of liquid should not exceed 0.13 liters;
- kidney diseases.
Open prostatectomy is the most common method of tumor reduction, but there are limitations:
- weight should not exceed 40 grams;
- the volume of liquid is not more than 0.14 liters.
Treatment of prostate adenoma
There are several methods of treating BPH, which also depend directly on the degree of development of the pathology. Treatment of the disease is often complex: medicinal methods are combined with the use of additional alternative traditional medicine, the prescription of a special diet and physical exercises aimed at improving blood circulation and eliminating congestive processes.
Drug treatment
If the disease is at the first stage, then the pathological process can be slowed down with the help of special medications.
If the prostate has increased in size due to adenoma, then the treatment method is alpha-1-blockers such as Alfuzosin or Tamsulosin. The products improve the urinary process, eliminate inflammation and irritation in the urinary tract, and restore normal tone of the smooth muscles of the gland.
Alpha-5-reductase drugs are also prescribed to shrink the gland. The drugs help neutralize the effects of androgen hormones on the prostate gland.
To relieve pain, doctors prescribe painkillers, available in the form of suppositories and tablets.
Surgery
If the patient is diagnosed with a second or third degree of severity of adenoma, then surgical methods of therapy are often prescribed (laser vaporization, embolization of prostate arteries, microwave treatment, prostatectomy, and others).
Source vylechim-prostatit.ru
Reducing prostate size at home
There are many methods for home reduction of the prostate described, but in most cases they are combined with the main therapy, for example, taking medications, antibiotics, physiotherapy or taking dietary supplements. There is no need to replace taking medications with tea or exercise - everything should be done in combination and with a competent approach.
Prostate adenoma cannot be reduced so easily, but prostatitis can be dealt with.
The 100% effectiveness of the same biological additives has not been proven, so there is no need to rely solely on yourself in this regard. Hardware treatment at home should be carried out only with the permission of a doctor, as well as taking medications.
Prostate massage is allowed for home use, but only if you have enough knowledge not to harm yourself.
No one can prohibit drinking infusions and teas that help cleanse the urinary ducts and have antibacterial properties; you just need to take into account the individual characteristics of the body. If taking infusions is comfortable for you, then drink them according to the instructions indicated. Just study your body’s reaction, since individual intolerance to some products is quite possible, especially if you have not used the product before.