Low hemoglobin is not an independent disease. It is the result of an underlying disease, therefore, if anemia is detected in a patient, the doctor is obliged to prescribe a comprehensive examination.
Concepts of pseudoanemia and hidden anemia
Pseudoanemia is the entry of tissue fluid into the bloodstream during the resorption of edema.
Hidden anemia is the result of the loss of a significant part of the fluid composition of the blood due to dehydration (can be caused by diarrhea, vomiting, hyperhidrosis). In this situation, the blood begins to thicken, so laboratory analysis shows that the number of red blood cells and hemoglobin is normal, even if this is not the case.
Severity of anemia
Based on severity, anemia is classified into:
- light. Hemoglobin level is more than 100 g/l, erythrocytes - more than 3 T/l;
- average Hemoglobin level from 66 to 100 g/l, erythrocytes - from 2 to 3 T/l;
- heavy. Hemoglobin level is less than 66 g/l.
Classification of anemia
All anemias manifest themselves differently. Taking into account the cause of the pathological condition and its symptoms, there are four main types:
- posthemorrhagic anemia (caused by chronic/acute blood loss);
- hemolytic anemia (develops due to the destruction of red blood cells). This group includes hereditary hemolytic anemias: - with a lack of glucose-6 phosphate dehydrogenase; - thalassemia; - sickle cell; — Minkowski-Shoffar;
- deficiency anemia (caused by a deficiency of microelements/vitamins/iron, that is, any elements that play an important role in the process of hematopoiesis);
- hypoplastic anemia (results from impaired hematopoiesis in the bone marrow, the most dangerous form).
According to the color indicator of blood, anemia can be:
- normochromic (hemoglobin is normal). This group includes hemolytic and posthemorrhagic anemia;
- hyperchromic (hemoglobin increased). These include folate deficiency and B12 deficiency anemia;
- hypochromic (hemoglobin is low). This refers to thalassemia, iron deficiency and chronic posthemorrhagic anemia.
Based on the diameter of red blood cells, anemia can be:
- normocytic (almost all hemolytic and acute posthemorrhagic anemia);
- megaloblastic (B12-deficiency anemia);
- macrocytic (folate deficiency, hemolytic disease of the newborn);
- microcytic (chronic posthemorrhagic anemia).
Based on the iron content in the blood serum, anemia is divided into:
- normosideremic (acute posthemorrhagic anemia);
- hyposideremic (chronic posthemorrhagic and iron deficiency anemia, thalassemia);
- hypersideremic (hemolytic and B12-deficiency anemia).
Causes of anemia
Common causes of low hemoglobin are:
- large blood loss;
- disruption of the formation of new blood cells;
- activation of pathological processes of blood destruction.
Causes of posthemorrhagic anemia
Acute posthemorrhagic anemia is the result of the loss of a large amount of blood in a minimal period of time. The chronic form of this disease is caused by:
- prolonged blood loss;
- polyps, hernias and stomach ulcers;
- kidney diseases;
- malignant tumor neoplasms;
- uterine bleeding;
- disorders of the blood clotting system;
- liver failure, cirrhosis.
What causes hemolytic anemia
All hemolytic anemias occur if “old” red blood cells begin to destroy faster than new ones can form.
The sickle cell form is caused by the synthesis of a defective hemoglobin molecule. The emerging defective molecules form peculiar crystals that stretch the red blood cell, causing the latter to take on the shape of a sickle. Sickle erythrocytes are non-plastic. It leads to increased blood viscosity and blockage of small blood vessels. With their sharp ends they can destroy each other.
Thalassemia is a hereditary disease. It occurs due to a decrease in the rate of hemoglobin formation. Hemoglobin that is not fully formed is unstable. It resembles small inclusions that give the red blood cell the appearance of a target cell.
Deficiency anemias and their causes
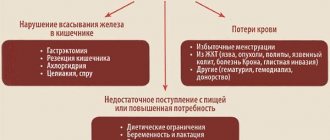
Iron deficiency anemia develops for reasons such as:
- lack of iron/increased need for iron (this is why degree 1 anemia is often diagnosed in premature babies and pregnant women);
- chronic blood loss;
- problems associated with the absorption of iron from the gastrointestinal tract, its transportation and disposal.
B12 deficiency anemia is caused by a lack of vitamin B12. The disease can be caused by poor nutrition (refusal to eat meat) or disruption of the absorption of cyanocobalamin in the gastrointestinal tract (parasites, diseases of the small intestine, stomach). Also, symptoms of B12 deficiency anemia can appear while taking hormonal drugs and anticonvulsants.
Folate deficiency anemia is a consequence of a lack of vitamin B9. It is usually observed in pregnant and lactating women, cancer patients, teenage children, premature newborns, liver disease, alcohol abuse, etc.
Causes of hypoplastic anemia
Hypoplastic anemia is manifested by a decrease in the content of all cells in the blood. External and internal factors lead to such a pathological and life-threatening condition:
- vibration and radiation effects on the body;
- serious injuries;
- taking certain medications;
- ingestion of poisons into the body;
- herpes, fungi, bacteria;
- genetic mutations;
- rheumatoid arthritis, lack of elements involved in hematopoietic processes;
- endocrine diseases, etc.
Symptoms of anemia
Conventionally, the symptoms of low hemoglobin are classified into:
- specific (manifest only in specific types of anemia);
- nonspecific (the same for all types of disease).
Nonspecific symptoms of anemia are as follows:
- pallor of the skin/mucous membranes;
- migraine;
- increased fatigue;
- noise in ears;
- refusal of food;
- constant drowsiness;
- feeling of lack of air;
- dizziness;
- cardiopalmus;
- decreased libido, sexual impotence in men;
- disruption of the menstrual cycle;
- heart failure.
Specific signs of different types of anemia
Each type of anemia has its own specific symptoms. Thus, the acute posthemorrhagic form manifests itself:
- increased heart rate;
- fainting;
- cold sweat;
- attacks of dizziness;
- pale skin;
- decrease in body temperature.
In chronic posthemorrhagic anemia the following are observed:
- very white skin;
- craving for or intolerance to certain smells;
- swelling of the face;
- change in taste sensations;
- dry skin;
- brittle nails;
- nausea;
- lack of air;
- sweating;
- involuntary urination when sneezing or laughing;
- temperature increase.
Hemolytic anemias are characterized by:
- yellowness of the skin and mucous membranes (when red blood cells are destroyed, bilirubin enters the bloodstream);
- increased size of the spleen/liver;
- increased levels of bilirubin in the blood;
- darkening of urine and feces;
- high body temperature;
- weakness.
Sickle cell anemia - a type of hemolytic - has the following symptoms:
- jaundice;
- shortness of breath;
- formation of inflamed areas on the legs;
- blurred vision;
- the presence of hemoglobin in the urine.
Doctors diagnose thalassemia if the patient:
- the shape of the skull bones changes;
- the skin becomes very pale with a yellowish/greenish tint;
- eyes become narrow and swollen;
- there is a lag in mental/physical development;
- bones are deformed;
- the spleen/liver enlarges.
Signs of iron deficiency anemia include:
- buzzing in the head;
- lack of oxygen;
- migraine;
- constant desire to sleep, rest;
- dry skin;
- peeling of nails;
- hair section;
- desire to eat chalk, smell paint, etc.;
- violation of the act of urination;
- hyperhidrosis.
Also, during laboratory tests, it is discovered that the level of hemoglobin and red blood cells in the blood is significantly lower than the established norm.
B12 deficiency anemia affects the gastrointestinal tract and central nervous system. As a result, the patient experiences:
- swelling of the legs;
- crawling sensation on the arms/legs;
- change in gait;
- memory impairment;
- problems swallowing food;
- enlarged liver/spleen;
- drying of the gastrointestinal mucosa.
In turn, folate deficiency anemia manifests itself:
- inability to eat acidic foods;
- glossitis;
- difficulty chewing and swallowing food;
- enlarged spleen/liver;
- atrophy of the mucous membranes of the gastrointestinal tract.
The symptoms of hypoplastic anemia are:
- the appearance of ulcers in the mouth, on the skin of the face;
- bruising on the skin;
- severe bleeding gums;
- increased fatigue;
- desire to sleep;
- tachycardia;
- decrease in the number of leukocytes, red blood cells and platelets in a blood test.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
What is increased hemoglobin and why is it dangerous?
Let's take a closer look at the causes of high hemoglobin and the treatment of this abnormality before it leads to serious health problems.
Hemoglobin is a protein that transports oxygen and carbon dioxide along the lung-cell route. The normal concentration for men is 140 g/l, and for women - 130 g/l. Doctors also note that each age category has individual indicators.
A change in the concentration of this protein by 20 units is considered a deviation from the norm. When hemoglobin decreases, doctors talk about the development of oxygen starvation (hypoxia), which can provoke premature tissue death. If the amount of protein increases excessively, then the number of red blood cells also increases.
And this, in turn, leads to blood thickening, which can cause serious disorders:
- thrombosis;
- stroke;
- heart attack;
- pulmonary thromboembolism.
Such consequences arise only due to the high concentration of hemoglobin and red blood cells. But the violation can be secondary, i.e. the result of any illness. And therein lies an even greater danger!
Diagnosis of anemia
To identify anemia in a patient, the doctor conducts a comprehensive diagnosis, which includes:
- clarification of the circumstances under which health deteriorated for the first time, the symptoms that are most pronounced;
- studying the patient's life history. The doctor clarifies whether there are chronic diseases, a hereditary predisposition to any pathological conditions, whether there are bad habits, whether the patient has recently taken any medications, or whether there has been contact with poisons or toxic compounds;
- examination of the skin, determination of its color. Measurement of pressure, pulse;
- laboratory tests of blood and urine.
In some situations, the patient is prescribed a bone marrow test. It is necessary to understand whether there are any disturbances in the hematopoietic processes. Also, using special equipment, a trephine biopsy can be performed, during which the doctor correlates the bone marrow with the tissues surrounding it.
An ECG is usually performed to examine the heart. If necessary, the patient is referred to a hematologist.
Laboratory diagnosis of low hemoglobin
In blood biochemistry, if anemia is suspected, the levels of:
- glucose;
- cholesterol;
- uric acid;
- creatinine;
- electrolytes.
This is necessary in order to assess the condition of the patient’s internal organs. A urine test is also performed to exclude the presence of concomitant diseases.
Laboratory signs of different types of anemia:
- posthemorrhagic acute anemia. Reticulocytes more than 11%, the presence of immature red blood cells and red blood cells of abnormal shapes. Leukocytes - 12 g/l (increased), shift in the formula - to the left;
- chronic posthemorrhagic anemia. Presence of tiny, poorly colored and oval red blood cells. Unexpressed lymphocytosis. Iron - below 9 µmol/l. A decrease in the amount of calcium and copper against the background of an increase in the concentration of manganese, nickel and zinc;
- sickle cell anemia. Hemoglobin is reduced to a level of 50 to 80 g/l, red blood cells - from 1 to 2 T/l. Reticulocytes are increased by about a third. The presence of red blood cells, the shape of which resembles a sickle;
- Thalassemia. Detection of target-like red blood cells in a blood sample, an increase in the number of reticulocytes. Hemoglobin - 20 g/l, erythrocytes - 1 T/l. Decreased concentration of platelets and leukocytes;
- B12 deficiency anemia. The presence of giant erythrocytes. Their color is bright, there is no highlighted area in the center. Shape: pear-shaped or oval. Life expectancy is shortened. Detection of huge neutrophils, a decrease in the number of eosinophils (may be completely absent). The concentration of basophils and leukocytes also decreases. Bilirubin, on the contrary, is increased.
Folk remedies to increase hemoglobin
If HGB is reduced slightly (not lower than 100 g/l), there are no severe symptoms, then anemia can be treated with folk remedies.
At home, you can prepare decoctions, infusions from plants containing folic acid, iron, vitamin B12, as well as dietary dishes.
Basic recipes:
- Nettle decoction. Prepared from the tops of young shoots. Add one glass of herbs to 1 liter of boiling water, cook for about 5 minutes and filter. Drink 1-2 glasses daily.
- Potato juice. The drink stimulates hematopoiesis. Drink 100 ml before meals 2-3 times a day for 2-3 weeks.
- Rowan infusion. Pour two teaspoons of ripe berries into one glass of boiling water and leave for at least 1.5 hours. Take 100 ml 2-3 times.
- Infusion of rosehip berries. A handful of dried fruits are poured into 500 ml of boiling water, left in a thermos overnight and drunk 100 ml before meals several times a day.
- Carrot and sour cream salad. For breakfast, eat 100-150 g of carrots, this stimulates the production of red blood cells and hemoglobin.
For low HGB, freshly squeezed juices from pomegranate, carrots, beets, as well as grapefruits, oranges, kiwis, blueberries, black currants, raspberries, and persimmons are useful.
The disadvantages of traditional methods are the duration of treatment, side effects such as diarrhea, flatulence, and exacerbation of gastritis.
If your hemoglobin level continues to decrease during treatment, malabsorption or bone marrow disease may be suspected. Additional examination is required.
Treatment of anemia in children and adults
To get rid of the symptoms of anemia, you need to eliminate the factor that provoked the decrease in hemoglobin. So, if the pathological condition is associated with the presence of parasites in the body, you need to get rid of them, if with poor nutrition, start following a diet, if with a malignant/benign tumor, it should be removed.
In other words, treatment of low hemoglobin in men, women and children may be conservative or require specialized surgical procedures. Usually, in order to improve the condition of patients and reduce the severity of negative symptoms, doctors adhere to the following therapeutic regimen:
- drugs are prescribed that can compensate for the resulting deficiency - B12 for B12-deficiency anemia, iron for iron deficiency, B9 for folate deficiency, etc.;
- normalize the level of red blood cells. This can be accomplished by transfusion of red blood cells or washing of red blood cells. However, these measures when providing assistance to people with low hemoglobin levels are extreme and are carried out only if the resulting disease is life-threatening.
Treatment of acute and chronic posthemorrhagic anemia
Treatment of the acute form of posthemorrhagic anemia is carried out in a hospital or hematology clinic
. The medications prescribed to the patient help normalize the amount of blood and the level of formed elements, and are also aimed at preventing relapses of the disease. Taking into account the amount of blood lost, the patient may need a transfusion, the introduction of blood substitutes or red blood cells.
As for the chronic form of this type of anemia, it is impossible to get rid of its symptoms without eliminating the cause. After the factor that provoked the pathological condition has been eliminated, the patient will be prescribed a diet that includes eating foods rich in iron. Medicines that can be used are Sorbifer Durules, Ferrum-Lek, vitamins B12 and B9, etc.
Treatment of sickle cell anemia
The main goal of therapeutic measures when it comes to a patient with sickle cell anemia is to prevent the development of hemolytic crises. To do this, the patient must avoid being in places with low oxygen levels. In parallel, blood substitutes and red blood cell infusions can be used.
Elimination of iron deficiency anemia
Treatment of iron deficiency anemia includes eating foods rich in iron and treating existing gastrointestinal diseases. The patient should regularly eat:
- cheeses;
- porridge;
- chicken eggs;
- meat;
- dairy products.
Iron supplements can also help quickly get rid of the symptoms of anemia. The tablets usually used are “Ferrum-Lek”, “Totem”, “Sorbifer Durules”, etc. Injections are prescribed only for severe forms of the disease. It is important that the medicine used does not cause problems with the gastrointestinal tract. If constipation or flatulence occurs, the product needs to be replaced.
Treatment of B12 deficiency anemia
Complex therapy of gastrointestinal diseases and adherence to the principles of proper nutrition help eliminate the manifestations of B12-deficiency anemia. Most often, patients are prescribed vitamin B12 injections. They allow you to quickly restore hematopoietic processes in the bone marrow.
How to get rid of folate deficiency anemia
Folate deficiency anemia is treated by taking vitamin B9 and following a diet. The patient should include foods that contain high amounts of folic acid in their diet. This means citrus fruits, vegetables, herbs, asparagus, nuts, seeds, tomatoes, watermelons, corn, avocados, eggs, animal liver, cod liver, cereals, grain bread.
Treatment of hypoplastic anemia
A hematologist treats hypoplastic anemia. Depending on the age, gender and condition of the patient, he can use different methods - bone marrow transplantation, stimulation of hematopoietic processes, blood transfusion, etc.
How to normalize a value
Self-medication is dangerous in all respects, so you should not take pills before talking to your doctor. After measuring hemoglobin and blood iron, the therapist will make recommendations. They can be aimed at increasing or decreasing performance.
| Promotion | Demotion |
| Taking dietary supplements | Medications selected by a doctor will help lower iron in a patient’s blood with normal hemoglobin. |
| In case of acute deficiency, injections are prescribed to quickly increase the patient’s hemoglobin | The diet includes cereals, flour products, dairy products |
| Increase consumption of blueberries, chicken eggs, carrots, fish, beef liver | Quitting smoking - the more smoke enters the body, the more actively the level of blood viscosity increases |
Serum blood iron levels should be stabilized under the supervision of a physician. The patient takes the OAC as regularly as recommended by the physician. The goal of everything is to control the level of dynamics of changes in the level of concentration of blood cells.
Anemia risk group
Low hemoglobin is most often diagnosed in:
- people with gastrointestinal diseases (oncology, gastritis, stomach and duodenal ulcers, inflammatory process in the large/small intestine, etc.);
- persons with poor nutrition, vegetarians;
- people with a genetic predisposition to a certain type of anemia (the disease can be passed from parent to child).
What are the dangers of low hemoglobin?
Anemia can be simultaneously called both a dangerous and harmless disease. So, if we are talking about a mild degree of the disease in a pregnant woman or a small child, then this is more likely a variant of the norm than a deviation. After taking a course of iron supplements, the baby/future mother will become absolutely healthy.
At the same time, moderate and severe degrees of some forms of anemia can lead to such dangerous conditions as:
- anemic coma (the patient loses consciousness and does not respond to any external stimuli, death may occur);
- malfunctions of internal organs (kidneys and liver are especially often affected by anemia);
- decrease in hemoglobin level to less than 70 g/l (death is also possible).
Low hemoglobin in childhood
A decrease in hemoglobin to dangerous levels is observed in adolescence due to hormonal changes. In second place among the causes of anemia are nutritional disorders. The child’s diet must contain meat, vitamin-rich vegetables and cereals to normalize intestinal motility.
Newborns often have low hemoglobin levels if they did not receive enough nutrients in the womb. If there is no threat to the life of the baby, the amount of the substance increases to normal levels by correcting the nutrition of the mother and child.
Prevention of anemia
To prevent the development of anemia, it is necessary:
- avoid contact with poisons and toxic substances;
- refuse to visit areas contaminated with radiation;
- do not contact with sources of ionizing radiation;
- do not take medications uncontrollably;
- to harden;
- eat right, include meat, greens, fruits and vegetables in your daily diet;
- spend more time outdoors.
Secondary prevention of low hemoglobin includes:
- blood test once a year;
- seeking qualified medical help in the event of acute infectious and viral diseases;
- annual medical examinations;
- pregnancy planning (for women).
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
How often do you need to get tested for hemoglobin?
In accordance with WHO recommendations, a healthy child should be examined once a year to determine the amount of hemoglobin. In the presence of chronic diseases, children are examined regularly, including repeated clinical blood tests.
When taking a clinical blood test for hemoglobin, the following nuances should be taken into account:
- The hemoglobin concentration will be lower if you take a blood test from a child in a horizontal position (lying down).
- After eating a meal, the amount of hemoglobin decreases. Also, less hemoglobin is observed when taking the test in the evening.
- If a health care professional applies excessive finger pressure when collecting capillary blood, interstitial fluid may enter the blood sample and dilute it. Because of this, the hemoglobin result will be 5-7% lower than the actual level.
- In the event that venous blood is taken, and the tourniquet was applied for a long time by a health worker during the procedure, vascular stasis will occur and, as a result, the hemoglobin level will be elevated.
Any changes that suddenly arise in the baby’s condition should alert parents. For example, if the child began to get irritated for no reason, became capricious, circles appeared under the eyes, or the baby became pale. But you shouldn’t sign up for a blood donation without permission from a doctor. If you suspect your child has anemia, the first thing you should do is contact your pediatrician.