This group of anemias, such as hyperchromic ones, is evidence of a violation of hematopoietic processes. The main causes of such conditions are a lack of vitamins B12 and B9. Such hypovitaminosis is extremely dangerous, especially for children and pregnant women. In this category of patients, in the absence of proper control of the condition, the risk of death increases.
What is hyperchromic anemia
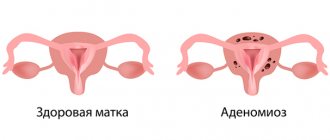
The disease, known to most people as anemia, in official medicine called “anemia”, is associated with a drop in hemoglobin levels. In the hyperchromic form, the number of healthy red blood cells simultaneously decreases and defective ones appear: containing excess iron. Thanks to this substance, the blood cells become saturated with hemoglobin, so their median clearing is covered with a scarlet color (this can be seen in laboratory tests). There are 2 types of hyperchromic anemia:
- Megaloblastic (macrocytic) - characterized by a violation of DNA and RNA synthesis, which leads to the appearance of very large red blood cells (megaloblasts and megalocytes) in the bone marrow. This anemia can be inherited.
- Non-megaloblastic - DNA synthesis is normal, the bone marrow does not produce megaloblasts, but defective red blood cells are present.
Most doctors do not consider anemia to be an independent disease, since it can develop against the background of a primary lesion of the blood system or with other pathologies that are in no way related to this. For this reason, there is no strict nosological classification and, in addition to the already mentioned division of the hyperchromic type into 2 types, there is a grouping according to the conditions to which it corresponds:
- Vitamin B12 deficiency (pernicious) anemia - Addison-Birmer disease, malignant anemia caused by a lack of vitamin B12. It is characterized by the formation of immature megaloblasts in the bone marrow and can manifest as neurological disorders.
- Folate deficiency anemia is also pernicious anemia, but occurs when there is a deficiency of folic acid.
- Myelodysplastic syndrome - characterized by cytopenia (deficiency of one or more types of blood cells) in the peripheral blood, dysplasia (improper development) of the bone marrow. The disease is prone to transition to the acute form of leukemia (poor-quality damage to the hematopoietic system), and is difficult to treat (maintenance therapy is carried out). According to official statistics, 80% of patients with myelodysplastic syndrome are over 60 years of age.
Hyperchromia → hyperchromic anemia
Perhaps, by the time the doctor begins to study the smear, the color index (CI) will already “report” the excessive saturation of red blood cells with hemoglobin and a change in their color as a result.
With hyperchromia, the color index will be higher than 1.1 - the limiting values for the norm ( normochromia: CP - 0.85 - 1.05 ). Red blood cell indices (MCH, MCHC), calculated by a hematological analyzer, will not be left out.
Hyperchromia is the leading laboratory sign of hyperchromic anemia and is most often combined with macrocytosis (hyperchromic macrocytic anemia). First of all, vitamin B12 deficiency and folate deficiency (folic acid - vitamin B9) fall into the category of such conditions. These are typical representatives of hyperchromic macrocytic (megaloblastic) anemia. Why megaloblastic? Because the cells are significantly increased in size and are represented by megaloblasts and megalocytes, and their diameter (>10 microns) is much larger than macrocytes (cells with a diameter of 7-8 microns are normocytes, more than 8 microns are macrocytes, less than 7 microns are microcytes), that is, megaloblastic means macrocytic, but macrocytic does not always mean megaloblastic. Something like this.
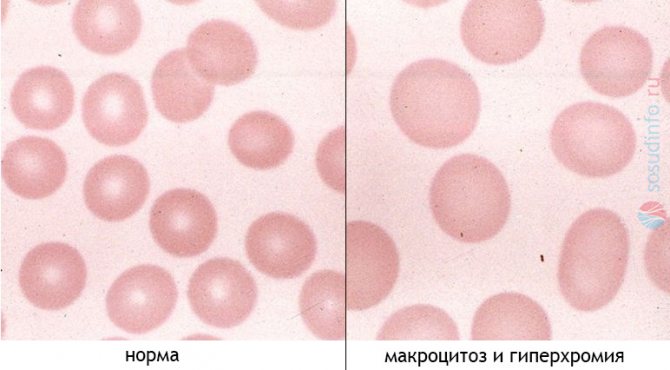
red blood cells in the blood of a healthy person and with hyperchromic macrocytic anemia
Thus, with a morphological study of blood samples taken from patients with hyperchromic macrocytic anemia, one can find:
- Red blood cells (which, in fact, are what we are talking about), are saturated with chromoprotein (hemoglobin) so much that it (Hb) erases the central clearing - hyperchromia (hyperchromasia);
- The diameter of red blood cells exceeds 10 microns (macrocytes and megalocytes);

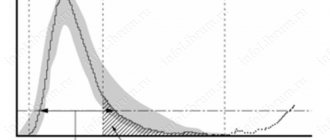
- Fragments of red blood cells (schizocytosis), anisocytosis are noticeable (as evidenced by the following indicators during automatic sample processing: average erythrocyte volume - MCV, volume distribution width - RDW, histogram), as well as a change in the shape of erythrocytes (poikilocytosis);
- You can often find red cells that have not lost their nuclear substances (Jolly bodies, Cabot rings, polychromatophilic elements);
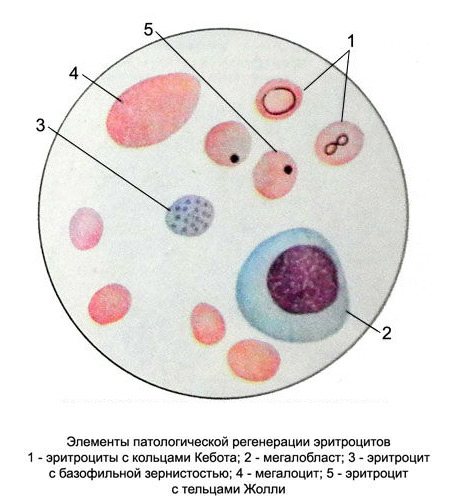
abnormal shapes of red blood cells in anemia - The content of young forms of erythrocytes - reticulocytes, initially remains within the normal range, but as the process progresses, differentiation is increasingly impaired and their number shows a downward trend;
- During a morphological study, one cannot ignore changes in white blood: a decrease in leukocytes (neutrophils, monocytes, eosinophils), the absence of basophils, but a slight increase in lymphocytes. In other cases, young precursors of white blood cells - myelocytes and young ones - come into the blood (shift of the leukocyte formula to the left);
- In the platelet unit, unnatural phenomena may also (to a moderate extent) be present (platelets acquire gigantic sizes, but their total number is reduced).
This whole situation (hyperchromia, macrocytosis, and shift in the leukocyte formula) is created by the megaloblastic type of hematopoiesis in the bone marrow, which is a common feature of all anemias of this kind (associated with impaired DNA formation). These anemias can be inherited or acquired during life.
Causes
Deficiency of vitamin B12 (cyanocobalamin) and folic acid are the most common starting points for the development of hyperchromic anemia, but these conditions can occur under the influence of a number of factors. There is a specific list of reasons for each situation. Lack of cyanocobalamin is provoked by:
- pathological processes in the ileum, in which the digestibility of nutrients is impaired due to poor absorption by its walls;
- infectious intestinal pathologies, which also disrupt the absorption of vitamins;
- worms – tapeworms and bacteria actively absorb vitamin B12;
- atrophic gastritis, in which insufficient synthesis of intrinsic Castle factor (an enzyme that converts cyanocobalamin from an inactive form to an absorbable one) is observed in the parietal cells of the stomach.
In hyperchromic anemia, which occurs as a result of folic acid deficiency, the provoking factors look different. Women often encounter this condition during pregnancy, since all the folic acid is used to build the neural tube of the fetus. The influence may also be exerted by:
- alcoholism;
- liver diseases (especially hepatitis, cirrhosis, liver failure).
Separately, doctors mention hyperchromic macrocytic anemia, which is hereditary in nature (autosomal recessive transmission from parents) and develops against the background of genetic mutations, and in women, a prerequisite for its occurrence is the use of hormonal drugs. If we do not consider individual types of anemia, in which hyperchromic nuclei appear in red blood cells, common causes include:
- prolonged fasting or poor nutrition (with a deficiency of vitamins and microelements in food);
- smoking;
- presence of tumors;
- infections (especially HIV) and viruses;
- regular large loss of blood during menstruation;
- stomach cancer, gastrectomy (complete excision);
- hypothyroidism (thyroid hormone deficiency);
- taking medications (Metformin, Neomycin, Difenin);
- frequent intestinal disorders.

Causes of anemia – Dr. Komarovsky
It all starts in the bone marrow
Hyperchromic macrocytic anemia is a consequence of the megaloblastic type of hematopoiesis. What all this means can be illustrated by the example of B12 deficiency anemia. So:
- The bone marrow (BM) exhibits high cellularity (due to the presence of a huge number of elements containing the nucleus), megaloblastic hematopoiesis and ineffective erythropoiesis;
- The division of cells that in the future should become full-fledged red blood cells at this stage (see above) is disrupted; they, significantly changing their size (become megaloblasts), also change their structure (the soft reticular nucleus, matures, like the cytoplasm, at different times) ;
- In the population of maturing megaloblasts, depending on the activity of the hematopoietic process in the BM, there is noticeable variability: some cells are more mature, others less so. And if at this stage in the bone marrow the vast majority of future red blood cells are represented by promyeloblasts or basophilic cells, then experts talk about “blue” CM;
- A distinctive feature of these huge cells is the early saturation of their cytoplasm with the delicate nucleus intact with chromatoprotein (hemoglobinization of the cytoplasm - so this is where hyperchromia comes from?);
- At the same time, noticeable degenerative processes occur in the nuclei (mitosis, disintegration of the cell nucleus), which gives them ugliness and, accordingly, inferiority - such cells do not live long, most of them never reach a mature state (“die” on the spot "birth" in "infancy");
- From the remaining erythrocyte precursors, megalocytes are formed (their life is also short) and macrocytes (which will subsequently become the defining laboratory sign of hyperchromic macrocytic anemia);
- It should be noted that a violation of cell division leaves the synthesis of red pigment at a normal level, only the process of formation of red blood cells suffers from this (destruction of nuclei, disintegration of megaloblasts - enhanced, ineffective erythropoiesis);
- Vitamin B12 deficiency leads to changes in white blood (DNA synthesis is impaired synchronously in all cells). The precursors of “adult” leukocytes (promyelocytes, myelocytes, young and rods), as well as mature segmented ones, change their size; in other cases, disorders also affect the platelet component, which explains the change in the blood picture in patients suffering from hyperchromic macrocytic anemia.
By the way, changes in the peripheral blood and bone marrow with folate deficiency anemia are similar to those with vitamin B12 deficiency, because in the synthesis of purine bases, without which DNA construction does not proceed in the right direction, folic acid closely “cooperates” with vitamin B12.
Symptoms of hyperchromic anemia
The disease has external and internal manifestations: the latter imply changes in general well-being, which are not always specific and do not make it possible to make an accurate diagnosis. These symptoms of hyperchromic anemia include:
- increased drowsiness, fatigue;
- decreased performance;
- loss of concentration.
This clinical picture is characteristic of most cases of anemia, so the disease is recognized only after laboratory tests. If the course is more severe, the following may be added:
- tachycardia (rapid heart rate);
- shortness of breath with minimal physical exertion (even after brisk walking);
- tinnitus (not constant);
- sleep disorders;
- loss of appetite;
- headache;
- decreased libido (sexual desire).
In almost all cases of hyperchromic anemia, changes in appearance can be observed: the skin turns pale, the skin becomes thinner, becomes dry, and the hands may acquire a yellowish tint. Early graying appears in the hair. The general clinical picture of severe anemia is supplemented by the following symptoms:
- weight loss;
- visual and hearing impairment;
- nausea, vomiting;
- loss of taste, lack of craving for previously favorite foods and dishes;
- muscle weakness;
- numbness of the lower extremities;
- feeling of chilliness;
- redness of the tongue to a crimson color, the surface becomes shiny.
Persons who have hyperchromic anemia combined with myeloplastic syndrome often experience dizziness and increased fatigue. Chest pain with strong heartbeat and shortness of breath is possible. If the nervous system is severely damaged, the sensitivity of the fingers (toes and arms) is impaired, and loss of consciousness and convulsions may occur. Blood pressure is predominantly low, the liver is enlarged (palpable by palpation).
Symptoms

Discomfort in the heart area may indicate anemia
The onset of hyperchromic anemia in most patients is not accompanied by any complaints. The only manifestation of the pathological condition may be pallor and/or fatigue.
As the disease progresses, general symptoms will appear:
- increasing weakness, fatigue, decreased performance;
- headaches, dizziness, tinnitus;
- thinning hair, nails, increased fragility;
- shortness of breath independent of physical activity;
- increased heart rate;
- lability of blood pressure;
- the occurrence of spontaneous pain in the heart area;
- the skin acquires a yellowish tint, the sclera becomes icteric;
- auscultation of a systolic murmur at the apex of the heart. The advanced stages of hyperchromic anemia are indicated by the appearance of a rough systolic-diastolic murmur.
Complaints from the digestive organs are typical. In this case, patients note a perversion of taste, decreased appetite, heaviness and a feeling of fullness in the stomach, alternating constipation and diarrhea, and discomfort in the right hypochondrium.

Varnished tongue for anemia
A distinctive feature is the “varnished” tongue - a change in the color of the tongue to bright crimson with a transformation of its surface, which becomes smooth and shiny. Patients experience almost constant pain in the tongue - during conversation, eating and at rest. Taste buds also undergo changes - sensitivity in them becomes dulled, food becomes tasteless, and habitual gastronomic preferences do not bring satisfaction. The condition worsens with the addition of bleeding gums.
Damage to the nervous system is manifested by numbness in the arms and legs, a crawling sensation, muscle weakness, and periodic cramps.
Possible complications
In children, anemia, in which hyperchromia of red blood cells is observed, can lead to a lag in mental and physical development, a decrease in the body's defenses (the child will often catch ARVI, and it will be difficult to tolerate even a cold). In adults, a common complication of anemia is a lack of oxygen in the blood, damage to the nervous system, which causes:
- hypoxia (oxygen starvation) of the brain;
- deterioration of memory and thinking;
- death of brain cells and disruption of its blood vessels;
- heart failure (can be fatal).
Complications of anemia
- Catering - what kind of service is it? How does an off-site restaurant work for organizing banquets and buffets?
- Weakness in the legs - causes and treatment. Symptoms of what diseases may include muscle weakness and tremors in the legs
- Liquorice - what kind of plant is it? Benefits and harms of licorice root, use in cooking and folk medicine
Possible consequences and complications

Hyperchromic anemia is especially dangerous during pregnancy
If left untreated, hyperchromic anemia in children can lead to delayed mental and physical development. A decrease in immunity will cause frequent, long-term colds with a considerable number of complications.
Hyperchromia is no less dangerous for pregnant women and the fetus. Lack of proper treatment can lead to spontaneous abortion, early birth, fetal development abnormalities, and death of mother and child due to bleeding.
Also, complications of hyperchromic anemia may include cardiomyopathies, severe cardiac arrhythmias, and heart failure.
Proper nutrition, a healthy lifestyle, timely diagnosis and proper treatment will help eliminate the pathological condition as quickly as possible and regain your health!
Diagnostics
The absence of a specific clinical picture for anemia of any type increases the importance of diagnostic measures to clarify the disease. A general blood test is the primary test, the results of which can show changes in the structure of red blood cells (shape and size of cells) and detect nuclear Jolly bodies. If there is a suspicion of hyperchromic anemia, the doctor additionally prescribes:
- biochemical blood test - to determine the level of bilirubin, serum iron level;
- fluoroscopy of the abdominal cavity (abdominal organs);
- Ultrasound of the digestive organs;
- immunological study - helps to identify antibodies that are specific against the cytoplasmic antigens of gastric parietal cells and the internal factor of Castle.
Treatment
For mild forms of hyperchromic anemia, the basis of the therapeutic regimen is dietary correction, especially if the problem lies in a deficiency of folic acid or vitamin B12. Additionally, it is important to take 8 mg of iron with food per day. The menu is based on the following products:
- chicken, beef liver (2-3 times a week);
- buckwheat grain;
- fish (especially cod);
- meat (it is advisable to include a rabbit in the diet);
- chicken eggs;
- cheeses;
- legumes.

Be sure to eat fresh vegetables and fruits to complement the list of foods useful for anemia. Spicy and fried foods should be avoided as they irritate the digestive system. Caffeine is also excluded, since it interferes with the absorption of iron. This diet should be followed for several months (in some cases, more than a year); it is relevant for all stages of the disease, but individual correction of the diet for a specific clinical picture is possible. Drug treatment depends on the causes of anemia and its course:
- Therapy for mild deficiency conditions begins with the administration of Cyanocobalamin: a synthetic analogue of vitamin B12, which is taken orally or injected intramuscularly. If 1-1.5 weeks after the start of its use no positive dynamics are observed, the doctor prescribes Folic acid (tablets), Femibion. In some cases, simultaneous treatment with both drugs is carried out.
- For moderate anemia, Cyanocobalamin or Oxycobalamin (a stronger drug for severe cases) is administered intravenously and on days 5-8 the level of reticulocytes is monitored: their number should increase by 20-30%.
- If necessary, iron supplements are prescribed - Maltofer, Hemofer (tablets, injections), especially if the disease is diagnosed in a child.
- During pregnancy (or after childbirth, if the condition does not improve), the doctor may prescribe intravenous vitamin supplements to the patient, starting with large doses. Afterwards they decrease, and the injection form is replaced by the oral one.
The restoration of blood counts occurs quickly: within a month you can see the result, but neurological disorders are eliminated more slowly and may require additional medications. If the initial (mild) form of hyperchromic anemia can be treated on an outpatient basis (at home), then the moderate and severe form requires the patient to be placed in a hospital, where he will be given injections of drugs and constantly monitor his condition. A few points for treating such cases of anemia:
- A sharp disturbance in hemodynamics, a drop in hemoglobin below 70 g/l (severe form of anemia) requires immediate hemotransfusion - blood transfusion.
- Myelodysplastic syndrome requires hospitalization, blood transfusion (transfusion of red blood cells and platelets, often with cell replacement) and intravenous administration of drugs that accelerate the division of blood cells to prevent leukemia.
- If treatment involves injecting medications simultaneously with taking pills, this course lasts 2-3 months. After that, 1 injection is given once a week, leaving the tablets, and after 2 months they are given once every 14 days. The main form of treatment for non-serious conditions is tablets.
Anemia How to treat anemia?
Prevention
Following the principles of a healthy diet, maintaining a good level of vitamins B9 and B12, and iron is the simplest and most important way to protect against hyperchromic anemia, especially for pregnant women. The diet used to treat it is also preventive in nature. Additionally worth:
- visit a gastroenterologist regularly;
- exercise;
- stop smoking;
- do not contact with pesticides;
- to walk outside;
- promptly treat infectious diseases and remove parasites;
- take vitamin and mineral complexes.