- What is a puncture biopsy for nodular formations in the lungs?
- When is a puncture biopsy performed for pulmonary nodules?
- How should you prepare for research?
- What does the diagnostic equipment look like?
- What is the basis for the research?
- How is the research conducted?
- What should you expect during and after the procedure?
- Who studies the results of a puncture biopsy for nodular formations in the lungs and where can they be obtained?
- Advantages and risks of performing a puncture biopsy for nodular formations in the lungs
- Limitations when performing puncture biopsy of nodular formations in the lungs
What is a puncture biopsy for nodular formations in the lungs?
Nodes in the pulmonary parenchyma are round formations or foci of pathologically altered lung tissue.
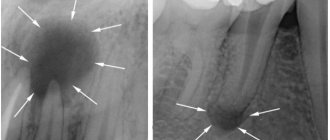
Most often, nodules are detected on a chest x-ray and are usually not accompanied by pain or any other symptoms. As a rule, nodular formations of any localization are detected during instrumental examination. However, imaging methods do not always allow us to talk about the nature (benign or malignant) of the detected changes.
A needle biopsy, or aspiration, involves removing a small sample of cells from a suspicious area using a hollow needle and then examining the resulting tissue under a microscope to make a diagnosis.
A puncture biopsy of nodular formations of lung tissue is often performed under visual control, for example, using MRI or fluoroscopy, which allows the doctor to bring the instruments precisely to the site of pathological growth.
Up
What procedures are meant by interventions on the chest organs?
Chest procedures include minimally invasive procedures that are used to diagnose the causes and treat pleural effusion, which is a collection of fluid in the pleural space.
The pleural cavity is a slit-like space inside the chest that surrounds the lungs. Pleural effusion occurs in a variety of conditions, including infections, inflammation, heart failure, and malignancies. Excessive fluid accumulation around the lungs makes breathing difficult.
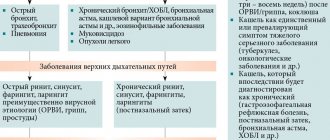
Interventions on the chest organs include:
- Thoracentesis
(thoracentesis, pleural puncture): removal of fluid from the pleural cavity using a needle attached to a syringe, followed by examination of the resulting sample under a microscope. - Pleurodesis
: the introduction of drugs into the pleural cavity in order to reduce its volume and the amount of accumulated fluid. - Pleural puncture biopsy
: involves removing a sample of pleural tissue, a thin layer of tissue that covers the outside of the lungs and lines the inside of the pleural cavity. In this case, a hollow needle is used, and the resulting sample is examined under a microscope.
Up
When is a puncture biopsy performed for pulmonary nodules?
Despite the fact that more than half of single (solitary) nodes in the tissues of the chest organs ultimately turn out to be benign, they are initially treated as malignant formations until the contrary is proven. This is exactly where a puncture biopsy helps.
After detecting a nodular lesion, an instrumental examination is carried out, which in most cases allows us to talk about the nature of the formation: benign or malignant. In cases where this is not possible, a puncture biopsy is necessary.
If the doctor prescribes a biopsy, this indicates that other diagnostic techniques, such as bronchoscopy, do not allow examining the nodular formation.
Up
How should you prepare for research?
It is usually recommended that you stop eating and drinking 8 hours before the biopsy. However, oral use of drugs is allowed with a small amount of water. Patients receiving insulin injections for diabetes should consult their doctor about changing the dose of the drug.
Before performing a biopsy, it is very important to inform the doctor about all medications that the patient is taking, including herbal ones, as well as any allergies, especially to local anesthetics. Three days before the procedure, you should stop taking aspirin or other blood thinners.
You should also tell your doctor if you have any recent illnesses or other conditions.
During the examination, you must wear a special hospital gown.
Women should always inform their doctor about any possibility of pregnancy. Some instrumental studies using imaging techniques are not performed during pregnancy to avoid negative effects on the fetus.
It is advisable to come to the hospital with a relative or friend who will help the patient get home. When using sedatives, this condition is necessary.
Up
Who studies the results of the procedure and where can they be obtained?
The results of the procedure are analyzed by an interventional radiology specialist, who draws up and signs a report for the attending physician.
After completion of the procedure or other treatment, the specialist may recommend that the patient undergo a dynamic follow-up examination, during which an objective examination, blood tests or other tests, and instrumental examination are performed. During this examination, the patient can discuss with the doctor any changes or side effects that have appeared after the treatment.
Up
What does the diagnostic equipment look like?
The biopsy needle is usually several centimeters long, and the syringe barrel is the diameter of a wide paper clip. The needle is hollow inside, allowing the tissue sample to be grasped and removed.
Several types of needles are used when performing a biopsy:
- Thin needle attached to a syringe: Thinner in diameter than needles used to draw blood from a vein.
- Automatic Cutting Needle with Spring Mechanism: Consists of an inner “thick” needle that is inserted into a locking cell covered with a cutting sheath and attached to a spring mechanism.
- Vacuum aspiration biopsy device: allows you to obtain a fairly large tissue sample.
A puncture biopsy is often performed under the guidance of CT, fluoroscopy, ultrasound or MRI.
CT scan
A CT scanner is usually a massive, rectangular machine with a hole, or short tunnel, in the middle. During the procedure, the patient is placed on a narrow table that slides inside the tunnel.
The X-ray tube and electronic X-ray detectors are located opposite each other inside a ring-shaped structure called a gantry. In a separate office there is a computer workstation where the resulting image is processed. There is also a doctor or technologist here who monitors the operation of the tomograph and the progress of the examination.
Fluoroscopy
Fluoroscopy typically uses an X-ray tube, a patient table, and a monitor located in the radiologist's office. To monitor the process and control the doctor’s actions, a fluoroscope is used, which converts X-ray radiation into a video image. To improve image quality, a special amplifier is used, suspended above the patient's table.
Ultrasonography
An ultrasound scanner consists of a console that includes a computer and electronic equipment, as well as a video display and an ultrasound transducer used for scanning. The sensor is a small, portable device that resembles a microphone and is attached to the scanner using an electrical cord. The ultrasound sensor sends high-frequency sound signals inaudible to the human ear and picks up echoes reflected from the internal structures of the body. The principle of operation of the device is similar to sonars that are used on submarines.
In this case, an image instantly appears on a monitor resembling a television or computer screen. Its appearance depends on the amplitude (strength), frequency and time it takes for the sound signal to return from the patient's body to the transducer, as well as the type and condition of the tissue through which the sound travels.
Up
How is a transthoracic lung biopsy performed?
Needle biopsy
A puncture biopsy is performed under local or regional anesthesia. Premedication is used beforehand. The patient is positioned in a lying or sitting position, depending on the location of the pathological focus. Before puncturing, the needle entry site is selected based on ultrasound, x-ray or computed tomography. Ideally, the shortest path from the puncture site to the tissue being examined is selected. In this case, the needle should go perpendicular to the chest. The selected point is marked on the skin of the chest.
Two types of needles can be used to collect material:
- Aspiration needle with a diameter of 21G. This is a thin needle similar to those used for venipuncture (taking blood from a vein). With its help, cell aspirate is obtained for cytological examination.
- Trephination needle. Its diameter is larger, 14G. Inside it there is a madren (special plug). When the needle enters the neoplasm tissue, the madrain is removed, and a stylet with a split end is inserted into the lumen of the needle, with the help of which pieces of tissue are plucked off. In this way, material is obtained for histological examination.
During the collection of material, the patient is asked to hold his breath, not move or cough. After this, the needle is removed and a bandage is applied to the puncture site. Immediately after the procedure or within 24 hours after it, a control x-ray of the chest is performed to exclude pneumothorax.
Open biopsy using minor thoracotomy
This biopsy is a full-fledged operation and is performed under general anesthesia. All manipulations are carried out through an incision, the length of which can reach 8 cm. It is located in the 3-4 intercostal space. A suture or staples is placed on the area of the lung from which the biopsy will be taken, after which the organ tissue is cut off. Open biopsy by thoracotomy is a traumatic procedure, but its advantage is the possibility of visual control and removal of a large fragment of tissue. After all the manipulations, drainage is installed in the wound, and a suture and a sterile bandage are applied to the incision site.
Thoracoscopic biopsy
In this case, manipulations are carried out through three small punctures of the chest wall. They are equipped with a video camera and special tools. The camera displays an enlarged image on the screen, which allows you to control the entire process, and the material is collected using tools.
The advantage of this type of biopsy is the low risk of complications (compared to open thoracotomy), low trauma, rapid patient recovery and good cosmetic results. At the same time, it remains possible to collect material under direct visual control.
Possible complications of transthoracic biopsy
- Pneumothorax is the accumulation of air or gas in the pleural cavity. More common after puncture biopsy. Its symptoms are chest pain and difficulty breathing. A small pneumothorax usually resolves on its own. But in severe cases, it can lead to a decrease in pressure and the development of acute respiratory failure. Then air evacuation is required. This is usually done using a syringe.
- Hemoptysis - blood in the sputum. Usually does not pose a threat to the patient's life and does not require medical intervention.
- Pulmonary hemorrhage. A symptom of this complication is a cough with sputum, which contains admixtures of scarlet foamy blood. Against this background, the patient experiences shortness of breath, and there may be bleeding from the nose or throat. As part of treatment, bronchoscopy or repeated surgery with hemostasis is performed.
At Euroonko, lung biopsies are performed by highly qualified doctors using expert-class equipment. Preference is given to minimally invasive techniques. This reduces the likelihood of complications and allows the patient to recover faster. Check the cost of the study with the specialists of our clinic.
Book a consultation 24 hours a day
+7+7+78
What is the basis for the research?
Image guidance allows the doctor to insert a needle through the skin and guide it to the suspicious area of tissue.
A sample of cells and tissues is collected using one of the following methods:
- A fine-needle aspiration biopsy
uses a small-gauge needle and syringe to remove fluid or a small sample of cells. - During a core needle biopsy,
an automatic spring mechanism is activated, which “pushes” the needle deep into the tissue. After returning the needle, the hollow part of the instrument is filled with a tissue sample in the form of a column. The cutting element of the instrument immediately cuts off the tissue and holds it inside the syringe. The process is repeated several times. - In a biopsy using a vacuum device,
the needle is first placed into the area of pathological changes. After this, a vacuum device is activated, which “sucks” the tissue sample under pressure into the hollow part of the needle. The tissue is cut using a cutting element and passes through a needle into a special reservoir. The process is repeated several times.
Up
How is the research conducted?
Typically, minimally invasive image-guided procedures, such as needle biopsies for lung nodules, are performed with the assistance of an interventional radiologist.
As a rule, in this case the study is carried out on an outpatient basis.
To administer sedatives during the procedure, the nurse inserts an intravenous catheter. In addition, a sedative may be prescribed orally.
The area where the biopsy needle is inserted is numbed with a local anesthetic. If the study is carried out under fluoroscopy control, then during the procedure the patient lies or stands in front of the screen.
During a CT or MRI-guided biopsy, the patient is positioned horizontally.
Tomography allows you to determine the exact location of the node in the lung parenchyma and the safest route for needle insertion. After detecting a pathological focus, the needle insertion point is marked with a marker. Hair is carefully removed from the skin, it is disinfected, and a sterile surgical drape is applied.
For very small lesions located deep in the lung tissue or near blood vessels, nerves, or airways, CT is preferred during the planning phase of the procedure. A CT-guided biopsy requires the patient to remain still for 30 minutes or more.
Fluoroscopy and ultrasound guidance are carried out in real time, which makes it easier for those patients who have difficulty holding their breath to perform a biopsy.
In some diagnostic departments, examinations of young children are carried out under general anesthesia, especially if the child is restless and unable to lie still. In such cases, one of the parents is allowed to remain in the office next to the child during the procedure. You can go home after the examination only after the child’s consciousness has fully recovered, which takes some time.
A tiny puncture is made in the skin where the biopsy needle is inserted. Under image guidance, the doctor inserts a needle through the skin, advances it to the nodule, and removes a tissue sample. A complete analysis may require several samples.
After the procedure is completed, the needle is removed, bleeding is stopped, and a pressure bandage is applied to the wound. No stitches are required.
For several hours after the biopsy, the patient is under the supervision of medical personnel. X-ray(s) or other testing is done to monitor for possible complications.
The procedure usually takes about an hour.
Up
2.Why is a biopsy performed and how is it done?
Why is a biopsy performed?
A lung biopsy is performed to detect the following diseases:
- Sarcoidosis or pulmonary fibrosis. In rare cases, a lung biopsy is performed for severe pneumonia, especially if the diagnosis is inconclusive.
- Lung cancer.
- To evaluate other abnormalities found on a chest x-ray or CT scan. A lung biopsy is usually done when other tests cannot pinpoint the cause of lung problems.
How is a lung biopsy done?
Bronchoscopy biopsies and needle biopsies do not require a postoperative hospital stay, unlike open biopsies, which require you to stay in the hospital for at least a few days.
Biopsy during bronchoscopy
carried out by a pulmonologist. Typically a thin, flexible bronchoscope is used. In rare cases, a biopsy may be done using a rigid bronchoscope. Bronchoscopy usually takes 30 to 60 minutes. You will be in the recovery room for 1 to 2 hours.
Needle biopsy of the lungs
performed by a radiologist or pulmonologist. A CT scanner, ultrasound, or fluoroscope is used to guide the biopsy needle. A small puncture is made and a needle is inserted. During the procedure, you must hold your breath and avoid coughing. After the required amount of tissue has been collected, the needle is removed and a bandage is applied to the puncture site.
Open lung biopsy
performed by a surgeon under general anesthesia.
The doctor will make a large cut between the ribs and take a sample of lung tissue. In a video-assisted thoracoscopic biopsy,
only two small incisions are made. The patient experiences much less pain and recovery is faster. The whole procedure takes about an hour.
Visit our Pulmonology page
What should you expect during and after the procedure?
The introduction of a local anesthetic to numb the skin is accompanied by a light injection, after which the sensitivity of the skin disappears for a while. There is a feeling of slight pressure as the biopsy needle is inserted.
Before the procedure, the doctor may prescribe the patient a mild sedative in tablets. In addition, sedatives are administered intravenously, if necessary, throughout the procedure.
The doctor asks the patient to remain as still as possible and not cough during the procedure. In addition, several times during the biopsy it is necessary to hold your breath for a short time. It is very important to hold your breath in the same manner to ensure correct needle insertion.
How to care for your skin after a biopsy may vary, but you can usually remove the bandage one day after the procedure and then shower or bathe.
During the day after the biopsy, it is necessary to observe a protective regime: do not lift heavy objects, walk slowly, do not play sports, avoid long stairs, etc. On the second day after the procedure, it is important to assess your condition and, if possible, return to your usual activities. If you plan to travel by air soon after your lung biopsy, you should consult your doctor.
After the local anesthetic wears off, pain often appears in the area where the biopsy needle was inserted, which, however, quickly goes away. In addition, when coughing, small amounts of blood may appear in the sputum.
Symptoms gradually subside within 12-48 hours after the procedure.
Signs of pulmonary atelectasis, which rarely occurs after needle biopsy of nodules, include shortness of breath, difficulty breathing, tachycardia (increased heart rate), sharp pain in the chest or shoulder when inhaling, and/or pale or bluish skin. If such symptoms occur, you should immediately call an ambulance.
Up
4.Risks and contraindications
Risks of Lung Biopsy
A lung biopsy is generally a safe procedure. Any risk depends on how severe the disease is. The following risk factors exist:
- A lung biopsy may increase the chance of developing a pneumothorax (accumulation of air or gas in the pleural cavity) during surgery. In this case, the doctor will place a tube in the chest to keep the lung inflated.
- Heavy bleeding (hemorrhage).
- Infections such as pneumonia may occur, but can usually be treated with antibiotics.
- Bronchial spasms may cause difficulty breathing immediately after the biopsy.
- The occurrence of arrhythmia.
After a lung biopsy, tell your doctor right away if you have:
- Severe chest pain.
- Dizziness.
- Labored breathing.
- Excessive bleeding.
- Cough with blood discharge (more than a tablespoon).
- Heat.
Advantages and risks of performing a puncture biopsy for nodular formations in the lungs
Advantages:
- A needle biopsy is a reliable method of obtaining tissue samples, which allows you to confirm the benign or malignant nature of the tumor.
- A needle biopsy is a minimally invasive procedure that does not have the disadvantages of a surgical biopsy, including the need for large skin incisions and general anesthesia.
- In general, the procedure is not accompanied by severe pain, and the accuracy of its results is comparable to a surgical biopsy. • Recovery after a needle biopsy is fairly quick, and patients can soon return to their normal lives.
Risks:
- Any procedure that involves violating the integrity of the skin carries a risk of developing infection. However, in this case, the chance of developing an infection that requires antibiotic treatment is less than 1 in 1000 cases.
- Bleeding.
- Coughing up blood (hemoptysis).
- If air enters the chest cavity through a puncture in the lung tissue, pneumothorax or pulmonary atelectasis may develop. For large lesions, the surgeon inserts a drainage tube into the chest to remove accumulated air. Usually the tube is removed the next day.
- A woman should always tell her doctor or radiologist about the possibility of pregnancy.
- The procedure is often accompanied by the use of ionizing radiation. However, the benefits of a biopsy significantly outweigh the possible risks from exposure to X-rays.
Up