To make an appointment with a doctor
Calling a pediatrician to your home
Our doctors
Our prices
A blood test is one of the most important examinations to assess a child’s health. Among the parameters that it determines is the level of hemoglobin. This is a protein that is involved in the transport of oxygen and carbon dioxide through the blood. It has a complex shape and contains iron, which is located in red blood cells. This is what red blood cells are called. If the hemoglobin level is reduced, then almost all parents know that this is dangerous, which is a symptom of anemia. However, there is also a reverse process when the causes and symptoms of high hemoglobin in a child appear.
An increased level is considered for the following indicators, which differ depending on the age of the child:
- up to 2 weeks – more than 200 grams per liter;
- 2-4 months – more than 180 grams per liter;
- 1-2 months – from 130 grams per liter;
- from 2 months to 5 years – from 140 grams per liter;
- 5-12 years – from 145 grams per liter;
- 12-18 years old - from 152 grams per liter for girls and from 160 grams per liter for boys.
Such indicators indicate increased hemoglobin in a child.
Causes of elevated hemoglobin in a child
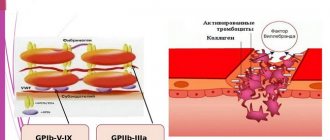
The reasons for increased hemoglobin in a child are most often associated with an excess of red blood cells in the blood and a lack of plasma. Very often, this phenomenon indicates that the body has lost a lot of fluid, causing the blood to thicken. This is the most common cause in children. It is triggered by intense sweating, overstrain of the nervous system, warm and dry air, drinking tea with a diuretic effect, and fever.
Pathological causes include the following:
- blood diseases;
- intestinal obstruction;
- kidney diseases, due to which erythropoietin is synthesized in large quantities;
- congenital heart diseases, pulmonary fibrosis and cor pulmonale (in these cases, an increased level of red blood cells compensates for the oxygen deficiency);
- severe forms of burns (in this case, the synthesis of red blood cells is increased to help deliver nutrients and oxygen to the affected areas of the body, and this promotes faster healing);
- Vaquez-Osler syndrome. This disease is also called erythremia or polycythemia. In this disease, the bone marrow produces an excess amount of red blood cells.
A child's red blood cells and hemoglobin may also be elevated if he smokes. In adolescence, frequent stress affects it, as well as the use of anabolic steroid drugs if the child plays sports.
What analysis should be done after a year?
After a year in children, the level of hemoglobin in the blood gradually rises:
- up to 5 years the norm will be 110-140 g/l;
- 6-10 years the indicator will increase to 115-145 g/l;
- From 11 to 12 years, the normal value will be 120-150.
Twelve-year-old adolescents begin puberty and standards are affected not only by age-related changes, but also by gender.
Table 2. Hemoglobin norm in adolescents 13-18 years old
| Gender | Hemoglobin norm (g/l) |
| Boys | 120-160 |
| Girls | 115-140 |
Eighteen-year-old boys and girls have the same standards as adults. Strong deviations up or down indicate the development of a pathological process.
Symptoms of hanging hemoglobin in a child
Symptoms of elevated hemoglobin will persist for a long time. As a rule, the child exhibits the following signs:
- severe drowsiness, weakness, fatigue;
- poor appetite;
- dizziness and headaches, fainting;
- problems with vision and hearing;
- the appearance of bruises even with slight palpation;
- arrhythmia, tachycardia;
- blue or pale fingertips and lips, numbness.
In addition to these symptoms of increased hemoglobin, blood clots can also be detected in the stool. Some people experience itching after swimming in the water. Problems with the urinary system may also occur, and sudden weight loss may begin.
Hemoglobin indicators by age
Immediately after birth, the child’s hemoglobin concentration is quite high and can reach 220-240 g/l.
In just two months, this figure drops sharply, and hemoglobin at 3 months can reach the minimum limit value of 90 g/l. It is at this time that the child develops physiological anemia, which does not pose a threat to health and is explained by the destruction of fetal hemoglobin. An infant does not yet have such a developed hematopoietic system and his body is not yet able to independently produce the required amount of protein. Doctors have a special table that determines the normal hemoglobin level depending on the age of the child up to one year. The table gives a clear idea of possible fluctuations.
| Age | Hemoglobin amount (g/l) | |
| upper limit | lower limit | |
| Immediately after birth | 240 | 180 |
| After three days | 225 | 145 |
| In one week | 215 | 135 |
| In two weeks | 205 | 125 |
| in one month | 175 | 110 |
| By the end of the second month | 140 | 90 |
| from three months to six | 135 | 95 |
| At seven months | 130 | 100 |
| At nine months | 130 | 110 |
| At ten months | 135 | 110 |
| One year old baby | 145 | 105 |
Hemoglobin in a 3-month-old baby, its normal range is 95-135 g/l. Both indicators do not cause concern and indicate the normal development of the baby. But deviations in one direction or another should alert parents and force them to immediately consult a pediatrician for advice.
Quite often there are cases when the hemoglobin level in a child at 3 months may be lower, and not only during this period.
There are several reasons for this phenomenon:
- genetic predisposition;
- lack of iron by the child during pregnancy;
- multiple pregnancy;
- prematurity;
- early ligation of the umbilical cord;
- seasonality of birth - the cool season can affect the decrease in iron levels in the newborn;
- mother's health status during pregnancy, bad habits, low physical activity, poor diet.
The level of hemoglobin decreases significantly during the baby’s illness.
Feeding the baby also matters. Breastfed babies receive all the necessary substances from their mother's milk, so their hemoglobin levels are normal. Artificial babies are more susceptible to changes in iron levels. So the choice of nutritious nutrition plays a very important role in the formation of the child’s body, in particular, the hematopoietic system.
Treatment of elevated hemoglobin in a child
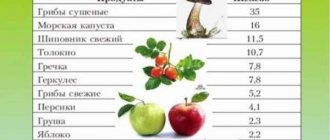
If hemoglobin is higher than normal in a child, then appropriate treatment is necessary. First of all, you need to give him fluids more often. Secondly, you will have to exclude from your diet foods that increase the level of hemoglobin in the blood. These include foods high in iron: beef, liver, apples, pomegranate, buckwheat porridge. It is best to give your child more chicken (especially white), seafood, and lean fish.
It is necessary to ensure that the child has minimal physical activity. A normal level of humidity in the room is also important. In more severe cases, the doctor will select special medications that will thin the blood. If the increase in the indicator is associated with any pathology, then treatment of the underlying disease is required.
Early anemia of premature babies
Early anemia occurs in healthy premature babies in the second month of life and usually ends by the end of the third. In sick children, anemia develops earlier. In mild cases of anemia, hemoglobin decreases within the range of 83–110 g/l, red blood cells – to 3,000,000–3,500,000. It is manifested by pale skin, but the child’s behavior does not change, he sucks actively, and gains weight well.
Moderate anemia is characterized by a decrease in the amount of hemoglobin to 66–82 g/l and is accompanied by pallor of the skin and mucous membranes, weakness, and loss of appetite. In severe anemia, the hemoglobin level drops below 66 g/l, the number of red blood cells drops below 2,800,000. The child gains weight poorly, becomes lethargic, has shortness of breath, and the pallor of the skin increases.
The severity of anemia depends on the degree of maturity of the child - the lighter the child at birth, the more severe it is. In children weighing less than 1.5 kg, anemia is more pronounced.
In severe cases, blood transfusion is indicated. In mild cases, rational feeding, regular long walks in the fresh air, massage, and daily bathing are sufficient.
In premature babies, anemia develops due to:
- increased destruction of red blood cells in premature infants in the first months of life;
- faster increase in blood volume compared to full-term babies;
- functional immaturity of the bone marrow.
What is hemoglobin?
Hemoglobin is a very complex protein that consists of four separate proteins - subunits, the holding element of which is an iron atom (Fe). Hemoglobin is contained inside the formed elements of human blood - red blood cells, which in turn make up the main volume of circulating blood, and iron, which is part of hemoglobin, colors the blood of all mammals and humans red. The only function of hemoglobin is to bind oxygen atoms in the lungs and transport this vital element to absolutely all organs and tissues.
This, to briefly explain, is why a person cannot live without hemoglobin, and, accordingly, without the iron that is part of it.
What is the normal hemoglobin level for a child?
A child is normally born with a high hemoglobin content from 150 g/l to 200 - 240 g/l, which is partly caused by the flow of blood from mother to baby during childbirth even before cutting the umbilical cord. But most of the hemoglobin in a newborn is his own fetal hemoglobin, which must be completely replaced with “adult” type hemoglobin by the 3rd month of the child’s life. That is why, by the end of the third month of a baby’s life, the hemoglobin level decreases to 100 - 110 g/l, and this process is a physiological norm, which, as a rule, does not require drug intervention. It is enough to recommend that a nursing mother remember to eat beef or lean pork, or lamb, every day, and also continue to take special vitamins for pregnant women for at least another 3 months after giving birth.
A separate problem is that a number of babies are born premature. Since these children were born earlier than nature’s due date, they did not have time to receive the full norm of necessary vitamins and microelements from their mother, which means that children born prematurely, as well as children whose mothers had low hemoglobin before and during pregnancy, will be in group at risk for developing iron deficiency anemia. An experienced pediatrician will, of course, prescribe iron supplements in the form of drops in a prophylactic dosage to children from the groups I have listed from 2 to 3 weeks of life, without waiting for a strong decrease in hemoglobin.
Starting from the age of 6 months, the lower norm of hemoglobin in a child is 110 g/l. If after this age a child has a hemoglobin level of, for example, 100 or 95 g/l, this is already a reason not only for the earlier introduction of complementary foods, but also for the prescription of iron supplements for replacement purposes.
Low hemoglobin in a child. Prevention of iron deficiency.
In the previous paragraph, we discussed in which cases prophylaxis with iron supplements is indicated for a child.
Now let's touch on the issues of rational nutrition of a child who was born full-term, with a normal hemoglobin level, but after 3 - 4 months his hemoglobin did not exceed the level of 110 g/l.
As we know, the first complementary foods are normally introduced to a child at the age of 4 - 4.5 months with fruit and vegetable purees. If by the age of 5 months we do not see a restoration of the hemoglobin level to 120 g/l, then in order to prevent anemia, we can begin to introduce meat purees from beef, veal or horse meat, lamb into the child’s diet from 5.5 to 6 months (if the child developed an allergy to cow's milk protein).
This is a modern, scientific approach, when, if there is a threat of developing anemia (a decrease in the level of red blood cells and hemoglobin below acceptable values), the child can begin to introduce meat purees as a second type of complementary food as a source of the most easily absorbed heme iron. And thus, by the age of 7 months, our baby can already receive up to 50 grams of meat puree once a day, and after 6 months, he can begin to be introduced to special cereals fortified with iron. I think that this would be more correct than immediately feeding the child a concentrate of iron salts in the form of special drops.
I would also like to warn young mothers, in case the child has low hemoglobin, against the early introduction of chicken and quail eggs. In general, I personally recommend introducing the yolk no earlier than 6.5 - 7 months. But in our case, you need to know that egg yolk, like no other product, reduces the absorption of iron in the intestines due to its high cholesterol content. In other words, feeding your baby yolk and trying to increase iron levels at the same time means throwing good things down the drain. It will not enter the body.
Conversely, fruit complementary foods and vegetable purees such as zucchini or pumpkin significantly improve the absorption of iron. This is due to the presence of vitamins C and folic acid in their composition, which help iron maintain its correct valency and enter our body in a non-oxidized form. But carrot juice should not be given to your baby along with iron.
In addition, milk porridges, especially semolina porridge, also interfere with the absorption of iron. And the worst thing a mother can think of with an infant is to feed him whole cow’s or goat’s milk for up to a year. In this case, if not an allergy, then iron deficiency anemia is definitely guaranteed, since iron from animal milk is practically not absorbed by a human child.
Treatment of anemia in children
However, if by 6 - 8 months the hemoglobin level cannot be normalized, then what should the pediatrician do next? If the doctor is sure that this is definitely iron deficiency anemia, and this can be practically 99% determined by a detailed clinical blood test, calculating the color index, the average hemoglobin content in the erythrocyte, etc., then the only correct decision is to adequately calculate the dose of the drug containing iron, and prescribe a drug such as actiferrin or maltofer for at least 6 weeks.
If the pediatrician is not 100% sure, or if long-term treatment with iron supplements in an adequate, correctly calculated dosage does not lead to normalization of hemoglobin, then in this case I strongly recommend that you consult a pediatric hematologist to establish an accurate diagnosis and exclude hereditary (not associated with iron deficiency) forms of anemia.