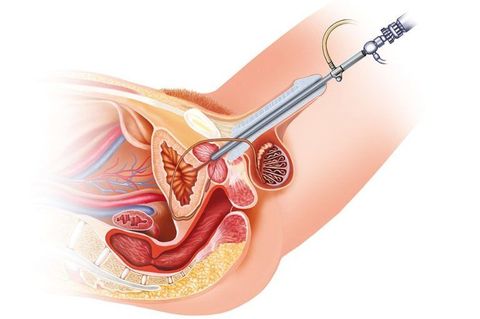
Cystoscopy is an endoscopic diagnostic method, during which the doctor examines the bladder from the inside. During the study, surgical manipulations can be performed in the organ cavity: removal of tumors, biopsy, destruction of stones, etc. To perform cystoscopy, special equipment is required - a cystoscope. Depending on the purpose of the study, a regular viewing or catheterization cystoscope can be used.
- Indications and contraindications
- How to prepare for cystoscopy of the bladder
- Execution method
- Possible complications
- Advantages and disadvantages of the cystoscopy method
Indications for cystoscopy
Cystoscopy is more informative than ultrasound of the bladder or x-ray.
The procedure can be prescribed at any age, but to examine children, a special pediatric cystoscope is required. Examination of pregnant women is allowed, but, if possible, the manipulation should be carried out after the baby is born. The uterus is in close proximity to the bladder, and even with the most delicate insertion of a cystoscope, there is a great danger of provoking premature birth. A cystoscopy examination of the bladder is prescribed by a urologist. The method is informative for diagnosing the following diseases:
- chronic cystitis, complicated by frequent relapses;
- urolithiasis disease;
- impaired urination, if other diagnostic methods have not clarified the nature of the pathology;
- urinary incontinence;
- the presence of a specific, pronounced odor of ammonia from urine;
- the appearance of blood in the urine, if the doctor excludes renal colic and stone passage;
- the presence in the urine analysis of atypical cells, red blood cells, leukocytes, protein, pus, schistosome eggs;
- frequently recurring pain in the pelvic area, heaviness in the perineum;
- urinary incontinence or frequent urge to urinate (especially in the case of nocturia - the urge to urinate at night);
- non-infectious cystitis;
- preparation for surgery on the uterus in case of oncological pathologies. In this case, using cystoscopy, the doctor clarifies whether the bladder is included in the tumor process;
- sexual disorders in men. During the procedure, the condition of the seminal tubercle is examined.
- suspicion of cancer in the urinary system. As a rule, cystoscopy is prescribed after the patient has had an ultrasound or CT scan.
During cystoscopy, it is possible to perform therapeutic procedures that alleviate conditions in diseases of the bladder and urinary tract. This way you can:
- remove bladder tumors – malignant and benign;
- stop the bleeding;
- take a tissue sample for a biopsy;
- crush and remove stones in the ureters;
- install catheters into the ureters;
- increase the internal lumen of the urethra or ureter by cutting the stricula (a place of narrowing of the internal lumen of the urethra);
- eliminate complete or partial obstruction of the urinary tract.
Cystoscopy capabilities
The use of cystoscopy provides the urologist with the following diagnostic and therapeutic options:
- Visual examination of the condition of the urethra and bladder, as well as observation of discharge from both ureters.
- Making an accurate diagnosis in a situation where the use of other methods (ultrasound, MRI, etc.) gives conflicting or unclear results.
- Taking tissue samples for histological examination.
- Extraction of urinary stones to study their composition.
- Collection of discharge from the ureters for laboratory study.
- Removal of small stones, polyps, blood clots, foreign bodies or small tumors.
- Carrying out electrocoagulation (cauterization) of ulcerative lesions of the mucous membranes.
- Rinsing the bladder and urethra (if blood or pus accumulates).
- Direct administration of drugs.
- Assessment of the degree of prostate damage due to inflammation or cancer.
When the procedure is contraindicated
In case of acute inflammation of the genitourinary system (cystitis, urethritis, prostatitis, orchitis), internal bleeding and obstruction of the urethra, the patient must undergo a course of treatment and wait for recovery. After which you can do cystoscopy. Otherwise, there is a high probability of causing microtrauma and aggravating the course of the disease.
The doctor will postpone the procedure if the patient:
- increased temperature or fever;
- poor blood clotting;
- signs of a viral or bacterial disease;
- injuries to the genital organs, urethral mucosa, bladder;
- chronic renal failure;
- heart attack;
- pathologies of the prostate gland and testicles.
How to prepare for cystoscopy
Before the procedure, the doctor will order an ultrasound of the abdominal cavity, write a referral for a coagulogram, general blood test and urine test. Women need to take a smear for vaginal flora.
In a preliminary conversation, the doctor will discuss with you the need for pain relief. Typically, local anesthesia is sufficient for women; short-term general anesthesia is used if it is necessary to perform cauterization, remove a polyp, or perform other procedures that may cause pain to the patient.
1–2 days before cystoscopy, you will need to stop taking painkillers and non-steroidal anti-inflammatory drugs, anticoagulants and some other medications, as recommended by your doctor.
On the eve of the examination, you need to shave your pubic and perineal hair, and wash your genitals directly on the day of the procedure.
The procedure is carried out only on an empty stomach, so you should have a light dinner the night before. In the morning, 4 hours before cystoscopy, you can drink water.
Immediately before the cystoscopy, you need to urinate to empty your bladder.
It is important not to be nervous and to be psychologically prepared for the procedure. Cystoscopy can cause discomfort and even pain during severe inflammation. The doctor will do everything possible to avoid causing discomfort to the patient, and the procedure lasts only 5–10 minutes. It is worth suffering a little from the inconvenience and peculiarities of the procedure in order to obtain the information necessary for a high-quality diagnosis.
Features of cystoscopy
- Carrying out the cystoscopy procedure requires compliance with the rules of asepsis and antisepsis.
- In addition, when carrying out the cystoscopy procedure, the qualifications of the doctor are extremely important - the speed and quality of carrying out the cystoscope along the entire length of the male urethra depends on his experience and training (the urethra of men, as is known, is long, divided into physiological sections and contains anatomical bends).
Typically, cystoscopy in men is performed with a flexible cystourethroscope (fibrocystourethroscope) due to the above bends of the urinary canal, and in women - with a rigid cystoscope - since the urinary canal in women is short and straight.

How is cystoscopy performed?

The procedure can be performed using a cystoscope with a rigid or flexible tube. In the first case, the doctor inserts a solid endoscope up to 30 cm long into the bladder and conducts an examination through a special optical system, looking directly through the device. During rigid cystoscopy, fluid is pumped into the bladder to flush it out of possible pus and blood. The resulting waters are then collected and sent for analysis. This type of cystoscopy is more painful and requires anesthesia.
A cystoscope with a flexible tube makes the examination almost painless. The device follows the physiological shape of organs and easily penetrates hard-to-reach places. True, the image is not as clear as when a rigid endoscope is inserted, but the video camera, which is built into the head of the device, displays the image on the monitor. When examining with a flexible endoscope, the likelihood of causing injury to the patient is minimal. In modern diagnostics, doctors prefer flexible cystoscopy.
The research takes place in the following sequence:
- The patient undresses, puts on a sterile gown and lies on his back, legs slightly apart and bent at the knees.
- The doctor explains the sequence of the procedure and what sensations the patient will experience.
- An assistant treats the patient's genitals with an antiseptic.
- The urologist performs anesthesia; for men, the anesthetic is injected directly into the urethra using a rubber tube and held in it with a clamp for up to 10 minutes. During this time, pain relief begins to take effect. For women, local anesthetic applied to the cystoscope is often sufficient.
- The doctor inserts a cystoscope through the urethra. For easy administration, it is treated with a special gel.
- Urine is forcibly removed from the bladder and washed with furatsilin. Then 200 ml of saline is injected, which straightens the bladder and allows you to examine it in detail from the inside.
- The doctor examines the walls of the organ, the color of its mucous membrane (normally it should be yellowish-pink), checks for ulcers and tumors. Particularly carefully examines the place where the opening of the urethra and ureters are located.
- The device is carefully removed.
- If general anesthesia was not used, the patient can go home. However, immediately after the procedure he should not drive himself. If general anesthesia has been administered, the person remains in the recovery room until consciousness is fully restored.
Features of the procedure
During cystoscopy, the doctor conducts a visual examination of the bladder, paying special attention to the bottom of the organ and the orifices of the ureters. In addition, the specialist has the opportunity to administer the drug directly to the site of inflammation, perform tissue excision, and remove small stones or tumors. All pain that occurs in the urethra after the procedure disappears within a few days.
If we compare cystoscopy with ultrasound, x-rays and other non-invasive examination methods, it wins in terms of information content, since it allows us to obtain the most complete picture of the disease. During the procedure, the doctor can examine the inner surface of the bladder and urethra, which will clarify the diagnosis, establish the location and extent of the pathological process, and determine further treatment tactics.
Why is it worth having a cystoscopy?
The method allows you to obtain the most complete and reliable information about the condition of the patient’s urinary system.
Modern cystoscopes cause minimal discomfort and are not capable of causing chronic inflammation or infection.
Diagnosis is carried out by qualified doctors. Specialists act very delicately and carefully, so there is no risk of injury to the urethra or bladder.
Cystoscopy of the bladder has an affordable cost. You can check the current price by phone or through the website.
Features of the procedure in men and women

The length of the ureter in women is only 3–5 cm, which is almost 6 times shorter than in men. Therefore, in women, the procedure is faster, less painful, and even, by agreement with the patient, can be performed without pain relief.
True, in ordinary life, infection penetrates into the urinary system of women just as easily. Therefore, they need cystoscopy examinations more often than men.
If during cystoscopy it becomes necessary to perform any medical procedures on the patient, the anesthesiologist will administer general anesthesia to her.
The male urethra is longer - 15–22 cm. When inserting a cystoscope, men experience pain, and anesthesia is always used. The cystoscope is inserted gently and non-violently, with a possible spasm of the external sphincter waiting for this moment. Sometimes the doctor may ask the patient to take several breathing movements. At the first stage, the penis is lifted upward and an endoscope is inserted to the level of the sphincter ring. Then the penis is lowered and the endoscope overcomes the obstacle in the form of the sphincter.
The procedure is also complicated by the fact that the cystoscope must pass through the location of the prostate. Therefore, the procedure must be carried out extremely delicately and sparingly, otherwise the device can injure the mucous membranes of the urethra, the seminal tubercle, and even temporarily impair potency.
Features of well-being after cystoscopy
As soon as the anesthetic wears off, patients may experience discomfort, aching pain, and a burning sensation in the urinary tract that increases with urination. This symptom is especially pronounced in men. The urge to urinate becomes more frequent. If the cystoscopy was performed using a rigid endoscope, the patient may notice a small amount of pink mucus protruding from the urethra. This is a common occurrence and is not a sign of an incorrect procedure.
To make the discomfort go away faster, the patient needs to drink more fluid - up to 2-3 liters per day. This will make the urine less concentrated and help naturally “ soothe ” an irritated bladder. You can take a painkiller once.
If the pain does not go away within three days, droplets of fresh blood appear when urinating, chills or fever appear, you should immediately consult a doctor. The likelihood of complications during cystoscopy is only half a percent of all procedures performed, but only a doctor can evaluate your condition.
To avoid possible troubles, after cystoscopy, be especially careful about the hygiene of the external genitalia. Men can have sex only 10 days after the manipulation. Women should abstain for 5–7 days.
If the patient does not have any unpleasant symptoms, he returns to his usual lifestyle after 2-3 days.