Pap tests - what are they?
The vast majority of women (more than 90%) over the age of 18 have had a Pap smear at least once. According to a study published in the Journal of General Internal Medicine, 20% of American women had abnormal Pap smear results that could indicate cervical cancer.
Screening for cervical cancer is an important aspect of health care worldwide. The Pap test's effectiveness in fighting cancer is recognized in many countries, and deaths from the disease have fallen by more than 70% since the 1950s. This is mainly due to the spread of screening programs, which have become more accessible.
What is a Pap test?
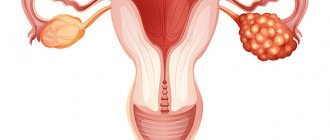
A Pap test, or Pap smear, is a procedure in which samples of cells are taken from the wall of the cervix and examined under a microscope. The test is needed to identify cellular abnormalities that may be a sign of cervical cancer and other diseases, such as infection and inflammation. A Pap test can detect precancerous lesions and small tumors that can cause cervical cancer.
The Pap smear is named after the Greek scientist Georgios Nikolaou Papanikolaou, who developed this method. Between 1917 and 1928, Papanicolaou was one of the first to bring attention to the diagnosis of diseases using cell samples. A number of studies have shown that mortality rates from cervical cancer have dropped significantly since the 1950s, when Pap smear screening programs were introduced.
To do a Pap test, the gynecologist examines the cervix and vagina, then takes samples of cells from the walls of the cervix, which leads to the vagina, and the cervical canal, which goes into the uterus. Next, these cells are placed in a solution, transferred to a small glass slide and sent to the laboratory for cytological examination.
Cytology examines the appearance, structure and function of cells under a microscope. If abnormalities are detected in the cells, the smear is sent for further examination to determine the degree of danger of the abnormalities.
How is it carried out?
To carry out the analysis the following are used:
- gynecological chair and lamp;
- metal or plastic vaginal dilator;
- examination gloves;
- cervical spatula and special brush;
- test tube or slide.
How is a Pap smear performed?
The patient is positioned on a gynecological chair. Her tailbone should be at the edge of the chair to ensure a good view when inserting the dilator.
A speculum is placed into the vagina. It is first recommended to warm it in warm water for the woman’s comfort. Some clinics use a small amount of special lubricant if necessary to facilitate insertion of the dilator.
The surface of the cervix should be completely open and thoroughly examined by the doctor. It is necessary to visualize the squamous epithelium, transition zone and external os. The transition zone is the area where squamous epithelium transforms into glandular epithelium. HPV affects this area. Therefore, cell selection is carried out in this zone. In addition, material is taken from the surface of the cervix and from the area of the external pharynx.
If necessary, the cervix is cleaned of secretions with a soft swab. The material is taken with a spatula or a special brush, turning them around its axis.
Depending on the equipment used, the resulting material is either placed in a special solution, which is in a test tube, or on a glass slide, onto which a fixative is then applied and placed in an alcohol solution.
The study is completed within a few minutes. It's painless. After the analysis, it is better to avoid sexual intercourse, use of tampons and douching for 5 days.
Can I take a bath after a Pap test?
It is recommended to do this no earlier than 5 days after the procedure.
Basic recommendations
In 2004, a group of scientists collected data on cervical cancer screening rates in the United States. They found that among women whose Pap test results were normal, 55% had Pap smears regularly, 17% every two years, 16% every three years, and 11% had them screened occasionally. The researchers found that even older women reported getting screened regularly (38% of women ages 75 to 84 and 20% of women over 85). About 20% of all respondents reported that they had received unsatisfactory test results at least once, while 80% of them regularly took Pap tests. Based on the findings, the scientists suggested that doctors perform Pap tests in women over 21 years of age who are not at risk of developing cervical cancer every 2-3 years.
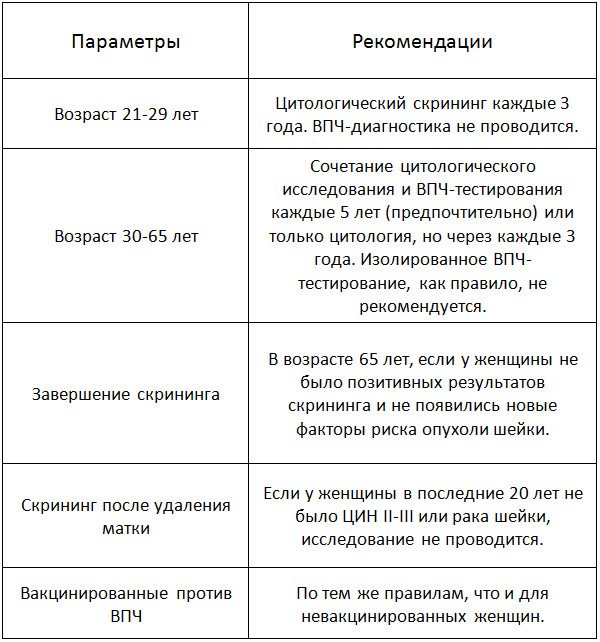
The American Society of Obstetricians and Gynecologists recommends that women get a Pap smear every two years after age 21. After 30 years of age, screening can be performed every 3 years if the woman is not at risk and has received three satisfactory Pap tests in a row. The American Cancer Society suggests that women aged 30-65 should have both a Pap test and an HPV test every 5 years. Women who are at high risk of developing cervical cancer due to a weakened immune system due to infection, organ transplantation, or long-term steroid use should be screened more frequently.

The American Cancer Society also suggests that women over 65 who have had regular screenings that have not shown any serious precancerous lesions in the past 20 years may stop getting a Pap test.
Women who have had a total hysterectomy may also not have a Pap smear if the surgery was done as part of treatment for a precancerous cervical condition.
Indications
For timely diagnosis of malignant tumors, a simple method that has no contraindications is needed. A cervical Pap test is a screening test that allows most women to be examined regularly.
According to the latest recommendations of the American Cancer Society and the American College of Obstetricians and Gynecologists, the test should be performed starting at age 21, regardless of the onset of sexual activity.
Table. When is the best time to do a Pap test?
Benefit
The main benefit of the Pap test is that it is an effective method for diagnosing cervical cancer and has saved the lives of many women. Cervical cancer occurs when healthy cells in the cervix turn abnormal and begin to grow uncontrollably. Cancer cells penetrate deep into tissues, and as they develop, cancer can spread to other organs.
According to a study published in the journal Obstetrics and Gynecology Clinics of North America in 2009, incidence and death from cervical cancer have decreased significantly in the United States since the 1950s, by more than 70%. This decline is primarily due to the introduction of Pap tests in the 1940s. Cervical cancer was once the leading cause of death among women (it is now number 12). Scientists have found that in most developed countries, cervical cancer accounts for only 7% of all cancers in women, while in developing countries the figure is 27%. This difference is explained primarily by a lack of testing and timely treatment of precancerous conditions.
A 1994 study published in the International Journal of Gynecology and Obstetrics assessed the effectiveness of a Pap smear screening program in reducing mortality from cervical cancer. The analysis showed a 53% reduction in mortality due to screening, supporting the hypothesis that the Pap test plays an important role in a woman's health.
How does a Pap smear differ from a regular smear for oncocytology?
Unlike oncocytological smears, which are done in antenatal clinics, when performing a Papanicolaou smear, a specially selected composition of fixatives and dyes is used, which makes it possible to identify early precancerous diseases of the cervix with the greatest degree of reliability. This technique is standard for developed countries in Europe and America, as it gives the least number of false negative results. When taking smears using the usual method, fixatives are not used, and the set of dyes is extremely simplified.
When taking smears, the Center for Immunology and Reproduction uses glasses and dye sets specially purchased in the USA. After the study, all glasses are stored in perpetual storage in the laboratory, which allows comparison of smears from the same woman over a number of years.
What to do if the Pap test shows abnormalities?
If the test is abnormal, it does not mean you have cancer, but it does indicate that there are abnormal cells in the cervix. Since a smear is not a method for diagnosing the disease, it cannot show for sure the presence of cancer. A poor test may be due to inflammation or minor cellular changes (such as dysplasia). Before cancer cells appear in tissues, healthy ones undergo some changes, this is called dysplasia. With dysplasia, the cells look different, but they may not become cancerous. Other reasons for a poor Pap test include the use of a vaginal diaphragm, sexual intercourse, or cellular changes associated with the menstrual cycle.
Most non-cancerous problems detected by a Pap smear go away on their own. If your doctor notices any minor abnormalities, he will likely recommend repeating the test a few months later. If the abnormalities do not disappear and the abnormal cells progress, more detailed diagnostics may be required.
The human papillomavirus (HPV) test detects the presence of human papillomavirus, which can lead to the development of genital herpes, changes in cervical cells, or the development of cervical cancer. If the Pap test is negative, your doctor may recommend an HPV test to see if the virus is causing the cellular changes. Most cases of cervical cancer are caused by infection with HPV, which is transmitted from person to person through sexual contact. HPV infections usually resolve on their own, causing minor cellular changes. But in some women, HPV remains and leads to serious problems with the development of cervical cells. The study, published in the journal Clinical Microbiology Reviews, suggests that Pap and HPV tests go a long way in identifying women at risk of developing cervical cancer.
If the Pap smear and HPV test are unsatisfactory, you may be scheduled for a colposcopy. During a colposcopy procedure, the doctor examines the cervix using a high-magnification instrument (colposcope). The doctor uses a weak acetic acid solution on the cervix to make abnormal areas more visible. If abnormalities are noticed, a tissue sample (biopsy) is taken from the suspicious area. A biopsy is the only way to know whether the changes are cancerous or precancerous.
In the case of precancerous changes, the abnormal tissue is removed and the tumor stops growing. Regular Pap tests are due to the slow progression of cervical cancer. Preventing the development of abnormal cells will protect against the development of more serious diseases.
What to do if the biopsy indicates abnormalities?
Medical recommendations will depend on the histological report. At the “For Birth” clinic, experienced doctors who are experts in cervical pathology will prescribe appropriate treatment and a follow-up plan with repeat Pap smears at certain intervals. It is possible that procedures using electrowave therapy or laser therapy will be prescribed to remove the changed cells.
Dear women, remember that undergoing a cervical examination procedure once a year COLPOSCOPY WITH ONCOCYTOLOGY will relieve you of fears of cervical cancer!!!
Articles on the topic All about colposcopy. Diagnostics,... What is the thyroid gland?...

A little about women's rules of feminine hygiene Breast care before and during... Eat right during... How to increase immunity? Interview…