In this article, we are looking for a simple answer to a simple question that is now in the top searches on the Internet - “how to choose a research method to take a coronavirus test.” There is a lot of information on the Internet, it is complex because it is written mainly by doctors and laboratories. And also because not everything is clear about the coronavirus in principle, and therefore there are a lot of streamlined phrases. And this does not help the patient understand.
We are interested in 2 simple questions:
- How can I tell if I am currently sick/contagious?
- How do I know if I have been sick in the past/if I am immune?
We have briefly described the main types of coronavirus tests that clinics and laboratories now offer. It’s impossible to do without specific terminology, but we tried to describe them as clearly as possible. And what is most valuable, they told us what types of tests are indicative during what period of the disease, what the positive and negative results of a particular method mean, and in what cases it will be necessary to undergo repeated testing.
Molecular diagnostics of coronavirus (PCR)
The most important laboratory method is PCR in biomaterial taken from the respiratory tract (nasal and oropharyngeal swabs).
The essence of the PCR method is that the genetic information of the virus (RNA) is copied many times in the laboratory by a special device - an amplifier, doubling its concentration in each copying cycle. This makes it possible to detect a virus or bacteria even in cases where its number is only a hundred cells per milliliter of blood. If the genetic information of the tested bacterium or virus is not present in the sample, it is not copied and is not detected.
PCR testing is usually carried out for those who have symptoms of respiratory illness or who have had contact with a possible source of infection.
The absence of genetic material of the pathogen (negative result) means that the person is not infected at the time of taking the test. To confirm or exclude the presence of infection, the test is repeated at certain intervals.
PCR diagnostics are used to establish the fact of coronavirus disease. The virus can be detected immediately after infection, even if the patient does not yet show symptoms of the disease . It is appropriate to do the test if you have been in contact with a carrier of the infection or were in a place where infection was possible. It is also used to confirm the diagnosis.
However, molecular RNA tests are not completely reliable and may give negative results in a significant proportion of actually infected patients. This depends on the sufficiency of the virus content in the material of the selected localization at one or another stage of infection, the quality of the material taken, the sensitivity limit of the test, the presence of PCR inhibitors, etc. Therefore, in diagnosis, special importance is attached to the characteristic CT picture. In addition to these studies and clinical evaluation, studies aimed at detecting in the blood the specific antibodies produced by the body against SARS-CoV-2 may be useful.
No, we don't want to confuse you. If the test is negative, but symptoms are present, there is no need to read the articles, you need to consult a doctor. No one has canceled the specifics of the course of any infection. The doctor will use additional research methods and make a diagnosis. Don't self-diagnose. To do this, you had to graduate from medical school.
In our clinic, you can undergo RNA testing of coronaviruses SARS-CoV-2 (COVID-19), SARS-CoV and MERS-CoV using the PCR method (qualitative determination).
The test system was developed at the Central Research Institute of Epidemiology of Rospotrebnadzor. The sensitivity of the test system used is 103 copies of plasmids per milliliter (10*3).
Plague
The Black Death, the Black Pestilence (also bubonic and pneumonic plague) is a disease that was worse than war for people. Plague is an acute infectious disease characterized by a severe condition of the patient, severe organ damage and death. The causative agent of the infection, the plague bacillus, was discovered in 1894 by bacteriologists Alexandre Yersin (France) and Kitasato Shibasaburo (Japan).
Historical reference
The plague pandemic threatened humanity with global extermination three times. The first plague pandemic occurred in Egypt between 541 and 750 AD. e. The pandemic is called the Justinian Plague, as it arose during the reign of the Byzantine Emperor Justinian I. The peak of the epidemic occurred in 542. In Constantinople alone that year, thousands of people died every day.
The second outbreak of the Black Death occurred in Asia and Europe in 1347–1353. It was this plague epidemic that left an ominous mark on the European Middle Ages. About 25 million people became victims of the pestilence. In fact, the pandemic continued until the 19th century, reducing only the scale of its deadly onslaught.
The third pandemic began in 1855 in several Chinese provinces in central and southeastern China. Due to the flourishing production of steam engines at that time and successful trade between other continents, the plague spread to all parts of the world. However, it did not acquire the globalization of a medieval epidemic.
As a result of these epidemics, according to modern estimates, approximately 150 million people died.
Until the 20th century, there was no treatment for plague due to a lack of therapy. The patient was quarantined and sometimes they practiced cutting out the so-called purulent buboes that appeared on the patient’s body in the places of the lymph nodes.
Russian scientist Vladimir Khavkin developed the world's first vaccine against plague at the beginning of the 20th century, but the infection has many strains, making it impossible for everyone to develop antibodies. Plague can be treated with antibiotics: the earlier the disease is detected, the easier the treatment. Unlike smallpox, plague still occurs throughout the world. It kills about 2,500 people every year. In Russia, the last case of plague infection was recorded in 1979.
Source of disease
The source of infection is rodents, cats, camels, squirrels, lagomorphs, insects and fleas (about 55 species). It was fleas that became the main carrier of the plague pathogen in the Middle Ages. The incubation period of the disease lasts from 2 to 6 days. Before the advent of therapy, the mortality rate for bubonic plague reached 95%, and for pneumonic plague - 100%. Currently, death is possible in 5–10% of cases of infection.
In 2021, an American boy scout fell ill with the plague after living in the forest for several days.
Symptoms
- high fever;
- headaches and dizziness;
- chills;
- weakness;
- a swollen lymph node in the groin, armpit, or neck;
- muscle pain and aches;
- severe weakness;
- loss of consciousness;
- insomnia;
- high body temperature.
Prevention
- avoid contact with rodents and wild animals;
- get rid of rodents that live in the house or its surroundings;
- use gloves when interacting with potentially infected animals or their skins;
- When going outdoors, use special insect repellents (mosquitoes, ticks, fleas);
- Check your pets and take steps to treat your pets for parasites if any are found.
Testing for the presence of antibodies to coronavirus COVID-19
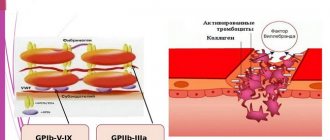
Similar to other viral infections, Coronavirus stimulates humoral and cellular immune responses (IgM and IgG). After the virus invades the body, immunoglobulin class M (IgM) first begins to appear in the patient’s blood, and later immunoglobulin class G (IgG), after which the immune system is activated and the cells of the immune system attack their own cells infected with the virus.
To answer the question of whether the patient is currently infected, whether the person has been exposed to the virus and whether he or she has developed an immune response, it is necessary to use tests to detect antibodies (Ig G, Ig M, Ig A) to a specific virus. Such tests are based on the methods of enzyme-linked immunosorbent assay (ELISA), immunochromatography (ICA) and their analogues .
Antibodies of class M appear in the acute phase of the disease and decrease after recovery. Antibodies of class G appear on the 7th day from the onset of the disease and last a long time, the duration of this time is still unknown.
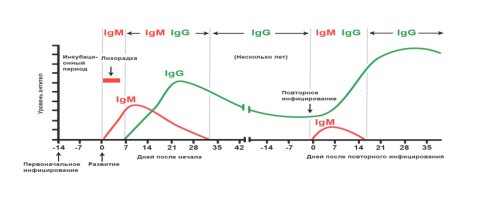
The presence and level of IgM antibodies in the blood can indicate a current or recent infection. IgM antibodies appear within a few days after the first manifestations of the disease (2-3 days from the onset of the disease), their concentration reaches a maximum on 7-10 days from the onset of the disease and are detected in the blood for 1-1.5 months. IgM is the first to be produced among all immunoglobulins when the body comes into contact with an infection, which is why they are called immunoglobulins of the primary immune response. Their presence in the blood indicates an acute stage of the infectious process.
Specific IgG antibodies are usually present in the blood for a long time and after recovery and can play a protective role. Therefore, testing the level of specific IgG to SARS-CoV-2 can help predict the likely presence of immune protection as a result of infection. Thus, the determination of IgG is not used in the early diagnosis of infection - it is detected in the blood two weeks after the onset of the disease, its peak is determined after a month and the duration of its determination is still unknown. IgG determines the appearance of immunity in the future.
For the initial antibody test, it is recommended to detect both IgM and IgG antibodies in the blood.
At our clinic, you can undergo rapid testing in 15 minutes using the ICA method or donate blood for an antibody test using the ELISA method. We work only with laboratories accredited by Rospotrebnadzor.
Smallpox
Natural, or smallpox, is known to mankind as a deadly disease that could be defeated. Smallpox is a dangerous viral infection with a high level of contagiousness. People who have had smallpox acquire lasting immunity to the infection. However, after an illness, scars and scars from painful smallpox ulcers often remain on the skin. Some smallpox outbreaks around the world have had a high mortality rate (up to 90%), but scientists and doctors have made every effort to destroy the smallpox virus.
Historical reference
The first mention of smallpox outbreaks dates back to the 6th century. However, historians suggest that a prototype of smallpox raged in the Roman Empire in the 2nd century.
At the end of the 18th century, scientists began to monitor the course of cowpox, which occurred in cows and horses. Visually, the disease resembled smallpox in humans, but it was milder and more benign. Observers noted that milkmaids also became infected with cowpox, which they tolerated easily and without consequences, and later turned out to be resistant to smallpox. The same was true of many cavalrymen in the 18th century English army, who were infected with smallpox from horses and subsequently became immune to smallpox. It was this principle that led scientists to develop the first vaccines.
In the 20th century, smallpox outbreaks worldwide killed more than 300 million people. Smallpox has also been used as a biological weapon. American colonists gave the Indians blankets infected with the virus, and while the inhabitants of the New World were dying from the infection, the colonists took over their lands.
The distribution of the vaccine reduced the spread of the virus, but epidemics continued to occur in Asia and Africa. In the late 50s, a smallpox outbreak hit Russia and claimed the lives of three people.
At the 11th session of the World Health Assembly in 1958, academician Viktor Zhdanov proposed global vaccination on a planet-wide scale. Initially, his idea did not find a positive response from the WHO, but the Soviet Union made the decision and supplied millions of doses of the smallpox vaccine to the WHO free of charge. In 1966, Zhdanov's idea of mass eradication of the smallpox virus was accepted.
The last case of infection occurred in October 1977 in the East African state of Somalia. The smallpox victim was a 40-year-old English woman who came to Africa as a medical photographer.
Today in the world there are two test tubes with the smallpox virus, which are stored in laboratories in Russia and the USA. In 2014, under WHO supervision, 6 test tubes with the deadly virus found in the university laboratory were already destroyed. Some scientists believe that due to climate change and other environmental problems, smallpox infection may make a comeback.
Source of disease
The incubation period is up to two weeks. The source of smallpox for humans is an infectious person and things with which the patient has been in contact. The virus penetrates the upper respiratory tract and skin, enters the bloodstream and spreads throughout the body. A person without immunity to smallpox has about a 100% chance of getting sick.
Symptoms
- increased body temperature;
- skin rashes (including on mucous membranes);
- nausea, vomiting;
- headache;
- muscle pain;
- weakness;
- fever.
Smallpox infection has been considered a forgotten disease for 43 years. But in view of the concerns of environmental and health organizations, it is better to get a vaccination in time that develops immunity to smallpox.
Rapid test for coronavirus (ICA)
Rapid tests are qualitative or semi-quantitative diagnostic methods that answer only the question of whether there are signs of the presence of coronavirus in the patient’s body and, in fact, do not make it possible to assess the amount of the pathogen.
Express tests are carried out using the immunochromatography (ICA) method; they do not require the use of special equipment, but require the presence of a nurse, since blood is drawn from a finger. The duration of the analysis procedure is within 10-30 minutes
A positive result of such a test requires mandatory verification using the PCR (polymerase chain reaction) method.
There are two types of rapid tests for COVID-19:
- SARS-CoV-2 direct antigen detection tests, which will determine the presence of components of the virus itself (for example, the protein coat)
- antibody detection tests (they are the most common in rapid diagnostics) are indirect tests for detecting immunoglobulins in the blood - IgM and IgG.
The analysis procedure is extremely simple:
- Collect a sample of blood or plasma or serum in a tube.
- Add a drop of sample to the special recess on the panel with the test tape.
- Place 2-3 drops of buffer solution into the recess.
- After 15 minutes we get the result - the appearance of colored areas on the test tape. The areas show either a negative result or the presence of IgM and IgG immunoglobulins, either separately or both together.
Antibody test for coronavirus (ELISA)
Indirect enzyme-linked immunosorbent assay (ELISA) is a semi-quantitative analysis that determines the amount of detected IgM and IgG antibodies. Venous blood is taken, and blood serum is used for research.
Indications for testing for antibodies to coronavirus COVID-19:
- Diagnosis of the disease.
- Definition of immunity.
- Obtaining information about a past illness with an asymptomatic course.
- Selection of donors for blood transfusions in patients with severe forms of the disease.
- Determining the stage of the disease and the period of contagiousness for others.
In a nutshell, what is the difference between ELISA and ICA? In what case is an expert test (ICA) sufficient, and when is it necessary to do a quantitative test (ELISA)?
It's a difficult question. Express tests - high specificity (almost 100%), i.e. works only for COVID-19, but low sensitivity (71%). And the ELISA method is more sensitive, but less specific. These are very subtle differences and the patient does not need them. An express test is fast, you can cover a large team, and quickly get an answer. And analysis from a vein is more thorough.
Briefly about all methods of diagnosing coronavirus
The test for coronavirus and antibodies to it are complementary diagnostics.
The coronavirus test is the detection of the virus in an oropharyngeal swab using the PCR method. It is used to detect the presence of coronavirus in the earliest stages, even if you do not have any symptoms of the disease. But it is usually used when symptoms are present, or when a positive test for M antibodies is present.
Analysis for antibodies to coronavirus allows us to identify both patients in the acute stage and those who have already recovered from the COVID-19 coronavirus.
The presence of specific class M antibodies (IgM immunoglobulins) are detected in the blood in the acute phase of the disease and decrease shortly after recovery. The presence of specific class G antibodies (IgG immunoglobulins) in the blood serum indicates the fact of infection with the SARS-CoV-2 virus in the past and the formation of a specific immune response (presence of immunity).
How can I tell if I’m sick now and if I could be contagious?
- If there are no clinical symptoms, then for the initial analysis, it is recommended to detect both IgM and IgG antibodies in the blood. By any method: ELISA (blood from a vein) or ICA (finger prick test). It is enough to do one test and get a negative result. In this case, there is nothing to worry about.
- If you decide to undergo a rapid test and class M antibodies have been detected, then you must do a smear test using the PCR method, even if there are no symptoms.
- If you donated blood (ELISA) and class M antibodies were detected, then you also need to do a smear test using the PCR method, even if there are no symptoms.
- If there are clinical symptoms, then first of all a smear diagnosis is needed using the PCR method, and a diagnosis for antibodies using the ELISA method (blood from a vein) is also desirable.
How can I tell if I have been sick in the past and if I have immunity?
- If there are no clinical symptoms, then for the initial analysis we still recommend taking a test to detect both IgM and IgG antibodies in the blood. By any method: ELISA (blood from a vein) or ICA (rapid finger prick test),
- to exclude the acute stage of the disease without symptoms (negative result - absence of immunoglobulin M)
- to find out if you have immunity after a previous illness (positive result - the presence of immunoglobulins G)
Marburg
One of the most dangerous viruses known to mankind, named after the German city of Marburg, where it was discovered in 1967. The Marburg virus is close in its symptoms to the modern Ebola virus. It also causes hemorrhagic fever and numerous bleedings. The fatality rate in the case of Marburg is close to 90%.
Historical reference
In 1967, an outbreak of a fatal infection occurred among workers in one of the laboratories in Germany. People contracted the virus from African green monkeys brought from Uganda for study.
History knows of 7 outbreaks of Marburg infection, the largest of which occurred in 2004–2005 in Angola. According to the Ministry of Health, 150 of the 163 cases of infection were fatal. According to some reports, cases of infection with the virus occur in isolated cases to this day.
In 2007, the virus was discovered in Egyptian flying dogs. Scientists suggest that this is one of the species that transmits the infection.
Source of disease
The incubation period for Marburg virus infection lasts from 3 to 9 days. The disease is not transmitted if a healthy person is in the same room as an infected person. Infection occurs through blood, saliva, feces, vomit, and contact with the patient’s personal and contaminated belongings. The virus can persist in seminal fluid for up to 2 months after recovery.
Symptoms
- fever;
- headache;
- muscle pain;
- skin rash;
- jaundice;
- pancreatitis;
- bleeding;
- organ failure.
Prevention
As a preventive measure, it is better to avoid traveling to African countries with a low level of development, where there is a high probability of infection due to the epidemic.
Interpretation of IgM and IgG results separately
| Positively | Negative | |
| IgM antibodies | presence of current or recent infection | presence of infection (early period) or absence of infection |
| IgG antibodies | presence of current or past infection | presence of infection (early period), absence of infection or recovery from infection in the distant past |
It is clear that nothing is clear. Everything can happen at the same time. It is for this reason that we recommend starting with a test to detect both IgM and IgG antibodies in the blood. By any method: ELISA (blood from a vein) or ICA (finger prick test). When these two indicators are combined, everything becomes much clearer.