According to the recommendations of the World Health Organization (WHO), a patient with infertility cannot be considered fully examined if, if pathology of the uterine cavity is suspected, she has not undergone hysteroscopy.
Hysteroscopy is an endoscopic examination method, which is a direct visual examination of the walls of the uterine cavity and cervical canal in order to detect intrauterine pathology.
Visualization is achieved using an optical system - a hysteroscope, which is inserted through the cervical canal into the uterine cavity. The hysteroscope is equipped with a video camera, and using fiber optic technology, the image of the cervical canal and uterine cavity is transmitted to the monitor screen.
Externally, the hysteroscope looks like a metal tube with a diameter of 3-5 mm. This instrument is based on an optical fiber that allows you to transmit images from the uterine cavity through a video camera to a monitor. On the monitor, the doctor performing hysteroscopy observes the uterine cavity at a high magnification of X 20. Good visualization is ensured not only by the quality of the optical devices, but also by the fact that a sterile saline solution is constantly supplied into the uterine cavity through a special channel of the hysteroscope. Due to this, the walls of the uterus, which are normally in contact, move away from each other, all blood clots are washed away and a refractive index is achieved, ensuring good visibility.
There are two types of hysteroscopy: diagnostic and operational.
- Diagnostic hysteroscopy is performed to detect any pathology in the uterine cavity; it allows to identify the presence of septations, adhesions, polyps, hyperplastic process, submucous fibroids, developmental anomalies, foreign bodies and chronic endometritis.
- Operative hysteroscopy (resectoscopy) is performed to correct the identified pathology. The tube of an operative hysteroscope is thicker than a diagnostic one, up to 8-10 mm in diameter. During hysteroresectoscopy, additional instruments (microforceps, scissors, etc.) are inserted through it, allowing the doctor to perform various therapeutic manipulations: you can remove polyps, destroy synechiae (adhesions), dissect septa, coagulate the endometrium and polyp legs. Using endoscopic methods (hysteroresectoscopy), you can also remove submucous uterine fibroids by first cutting them into pieces. Diagnostic hysteroscopy and operative hysteroscopy may be performed simultaneously or as two different procedures, depending on the specific situation. Hysteroscopy is not only a diagnostic, but also a therapeutic procedure.
Currently, hysteroscopy is recognized as the gold standard for studying the uterine cavity if any endometrial pathology or intracavitary pathology of the uterus is suspected.
At the Family Center, hysteroscopy is performed as an outpatient procedure and does not require hospitalization. Therapeutic and diagnostic hysteroscopy is performed under general anesthesia. Before the operation, the anesthesiologist examines the patient and selects the optimal anesthetic for her. Depending on the complexity of the procedure, hysteroscopy can take from ten minutes to one hour. After the operation, the patient remains in the day hospital ward for 1 - 1.5 hours.
During the procedure, endometrial curettage is performed, and the resulting material is sent for histomorphological examination. The result of histological examination is usually ready in one week. After receiving the histology result, the patient must come to see a doctor to discuss a further treatment plan.
Indications for hysteroscopy:
- suspicion of endometrial pathology during ultrasound or GHA;
- infertility;
- dysfunctional uterine bleeding;
- painful menstruation;
- bleeding after the end of menstruation;
- irregular or unusually light periods;
- habitual miscarriage;
- pain in the pelvic area;
- removal of small submucous fibroids, polyps, dissection of the intrauterine septum, synechae, removal of foreign bodies (IUD);
- several unsuccessful IVF attempts:
- removal of the remnants of the fertilized egg after an unsuccessful abortion.
Cleaning the uterus after bleeding
Bleeding from the uterus can occur for several reasons:
- Endometritis - if after an abortion the fertilized egg remains incompletely removed or pathogens such as streptococci, staphylococci, gonococci have entered.
- Bleeding due to hormonal imbalance;
- Hematometra is an accumulation of blood in the uterus due to cervical spasm.
Cleaning is carried out if there are fetal remains or polyps in the uterine cavity. The task of gynecological curettage is to stop bleeding and eliminate the causes that cause it. Otherwise, anemia gradually develops. The doctor prescribes hemostatic agents and drugs that promote uterine contraction.
If the pathology is infectious, a course of antibiotics is prescribed. And in case of hormonal disorders, consultation with an endocrinologist is necessary.
In addition to drug treatment, a nutritious diet is necessary, which contains foods that promote hematopoiesis. These are beef liver, buckwheat, red meat, pomegranate, beets, parsley.
Preparation for hysteroscopy:
- clinical blood and urine tests;
- bacterioscopy of a smear (smear for flora) from the vagina;
- Wasserman reaction, blood for HIV, hepatitis;
- determination of blood group and Rh status;
- ECG;
- biochemical blood test (total protein, glucose, ALT, AST, total bilirubin).
On the day of the procedure, you must arrive on an empty stomach. Registration for hysteroscopy at the Family Medical Center is carried out on the first day of the menstrual cycle by phone (347) 246-10-20.
It is most advisable to conduct the study in the follicular phase, on days 6–10 of the menstrual cycle, since on these days the condition of the cavity is optimal for visual examination. During this period, a more complete topical diagnosis of polyps, intrauterine synechiae, anomalies of the uterus, submucous fibroids, chronic endometritis, and foreign bodies is provided. In case of infertility of unknown origin, to clarify the secretory transformation of the endometrium, hysteroscopy is performed in the luteal phase of the cycle, on days 20–24.
Vacuum gynecological cleaning
Vacuum aspiration is one of the most common methods of abortion. Conducted during pregnancy up to 15 weeks. Manual vacuum aspiration – up to 9 weeks.
The advantages are:
- conventional medical instruments that are inserted into the uterine cavity are not used, as a result, the organ is not at risk of injury;
- in the early stages does not require general anesthesia;
- does not cause much damage to hormonal levels, since pregnancy is still in the early stages of development;
- the operation lasts only 3-10 minutes;
- return to normal life occurs within a few hours:
- minimal risk of complications.
As a rule, in this case it does not take much time to restore health. However, the method also has contraindications, the main one being exceeding the permissible gestational age.
Research technique
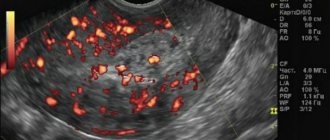
The external genitalia and inner thighs are treated with iodonate or alcohol. The cervix is exposed using vaginal speculum and treated with alcohol. The anterior lip of the cervix is retracted. The uterine cavity is probed and the length of the uterus is noted using the probe. Heger dilators consistently expand the cervical canal to ensure free outflow of fluid from the uterine cavity. Constantly washing the uterine cavity helps to quickly remove blood. The hysteroscope is connected to a light source and a sterile fluid supply system, after which it is inserted through the cervical canal into the uterine cavity.
The examination begins with a general overview of it, paying attention to the size and shape of the uterine cavity, the relief of its walls, the condition of the endometrium (color, thickness, folding, vascular pattern), accessibility and condition of the orifices of the fallopian tubes. While advancing the hysteroscope, the area of the uterine fundus, tubal angles, side walls, isthmic region and cervical canal are examined. The inspection is carried out in a clockwise direction.
During hysteroscopic examination, the uterine cavity normally has the shape of an oval, elongated in the transverse direction, in the area of the poles of which the mouths of the fallopian tubes are visible. The endometrium in the early proliferative phase is thin, pale pink, and a dense vascular network is visible through it. Gradually thickening in the proliferative phase, by the day of ovulation the endometrium forms longitudinal and transverse folds, and the vascular pattern becomes less noticeable. In the secretory phase, the endometrium is evenly colored, with a velvety surface; due to sharp thickening, it forms folds with flat tops. The spaces between the folds are in the form of narrow slits. A few days before menstruation, the color of the endometrium becomes more intense, and dark purple areas of hemorrhage appear in places where rejection begins.
The openings of the fallopian tubes are clearly visible in the first phase of the menstrual cycle. They are oval or slit-like passages located in the corners of the uterine cavity. In the second phase of the cycle, due to thickening of the endometrium and the formation of folds, the mouths of the fallopian tubes are difficult to visualize.
Hysteroscopic picture of endometrial atrophy: against the background of a thin pale pink mucosa, single vessels are visible, around which areas of hemorrhage may be located.
Stages of gynecological cleansing
The operation takes place in several stages. At the appointed time, the woman comes to the small operating room and sits in the gynecological chair. The anesthesiologist will ask questions about allergies to anesthesia, previous illnesses, and chronic diseases.
The following is the operation itself:
- The woman is given anesthesia (usually intravenously), which is enough for the entire period of the surgical intervention - 15-20 minutes.
- The patient does not feel pain and does not remember the manipulations that were performed on her. She sees pleasant dreams (modern anesthesia is used) and wakes up in the ward after the procedure;
- The doctor determines the position of the cervix using a speculum and then fixes it with special forceps. The uterus remains fixed during the operation.
- Then a special stick is inserted into the uterine cavity, which measures the length of the cavity.
- Next comes the stage of cervical dilatation. This is done gradually and carefully, using a dilator. The cervix should open to such an extent that you can freely pass a curette - an instrument similar to a spoon with a sharp edge and a long handle - inside. Curettage is performed using a curette.
- Once the cervical canal has opened to the desired size, the cleaning phase begins. A curette is inserted and the doctor uses it to carry out the main work. If the procedure is needed for diagnostic purposes, scrapings from the uterine mucosa are collected in a jar.
- To prevent the doctor from acting blindly, our clinic uses a modern method - hysteroscopy. A hysteroscope is inserted into the uterine cavity - this is a tube with a camera at the end. Using this device, the doctor sees the uterine cavity and all its walls. Cleaning is carried out under the control of a video camera.
- When the scraping is completed, the camera shows whether everything is done. If anything remains, repeated scraping is carried out until the result is what it should be.
- If some formations cannot be removed with a curette, then other instruments are introduced to remove the pathological areas. We are talking about polyps, synechiae, myomatous nodules growing into the uterine cavity.
- The next stage is completion of the work. After curettage, the forceps are removed from the cervix, and then the doctor treats the area of the cervix and vagina with an antiseptic solution. Ice is placed on the abdomen to stop bleeding in the uterine cavity.
- The patient is transferred to a ward, where she sleeps a little and wakes up. It is recommended to spend several hours in the ward or stay overnight. But if the woman feels normal, she can leave the room some time after waking up. The woman does not feel any pain.
Hysteroscopic picture of intrauterine pathology
Submucous uterine fibroids. During hysteroscopy, a submucosal myomatous node is identified as a round formation of pale pink color with clear contours, protruding into the uterine cavity. It is important to clarify the growth pattern and size of the myomatous node. Interstitial nodes are a protrusion of one of the walls of the uterus without clear contours. The mucous membrane covering the myomatous node is thinned, sometimes with the presence of small hemorrhages. During hysteroscopy, it is necessary to evaluate the size and location of the node, the presence or absence of a stalk, in order to decide the possibility of its removal transcervically.

Internal endometriosis (adenomyosis) . Hysteroscopic diagnosis of adenomyosis is difficult and often gives false-negative or false-positive results. If adenomyosis is suspected, the study should be performed on the 6-9th day of the menstrual cycle. Endometriotic ducts in the walls of the uterus are defined as pinpoint or slit-like spots of white color, from which blood may bleed. If there are a large number of passages, especially if they are localized in a separate area, the structure of the uterine wall may resemble a honeycomb.
Hyperplasia and endometrial cancer. During hyperplastic processes, the endometrium is unevenly thickened, forms folds of various sizes and shapes, often polypoid. The color of the mucous membrane is bright pink. With prolonged bleeding, it is quite difficult to establish endometrial hyperplasia hysteroscopically. To a large extent, the pathology of the endometrium helps to clarify microhysteroscopy or histological examination of endometrial scraping.
Microhysteroscopy allows you to detect adenocarcinoma in the early stages of development. The hysteroscopic picture is presented in the form of characteristic growths that bleed when touched.
endometrial polyps look like pale pink single or multiple formations of irregular oval shape, hanging into the uterine cavity. Sometimes the stalk of the polyp is visible. Under the flow of fluid, polyps can move relative to their base and also change shape. The surface of the polyp usually has a well-defined vascular pattern. Hysteroscopy allows not only to clarify the location of polyps, but also to perform their targeted, thorough removal.
Remains of the fertilized egg. During hysteroscopy, the remains of the fertilized egg can be identified in the form of polyps and bone fragments. A placental polyp is a purple-colored formation that bleeds when touched. Bone remains are determined in the form of dense whitish fragments embedded in the endometrium.
Foreign bodies in the uterine cavity are usually represented by intrauterine contraceptives (IUDs) or non-absorbable ligatures after uterine surgery. Hysteroscopy allows you to remove the IUD, having previously specified the location and degree of penetration of the spiral into the wall of the uterus. When a foreign body remains in the uterine cavity for a long time, fibrinous deposits are visible.
If non-absorbable suture material was used to suture the uterus, then during hysteroscopy in the isthmic part of the uterus one can detect the ends of the ligatures, often covered with fibrin.
Vesico-matonic fistulas. To clarify the fistula tract, indigo carmine solution should be injected into the bladder. In this case, a gap from which blue liquid is released will be determined hysteroscopically.
Perforation of the uterus. Small perforations are usually not detected hysteroscopically. If the perforation is large, hysteroscopy should be combined with laparoscopy.
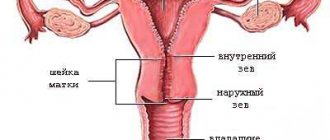
Unicornuate uterus. During hysteroscopy, it is determined in the form of a long cavity, gradually narrowing towards its distal section, with an oval depression, at the bottom of which the mouth of the fallopian tube is found. The folds of the mucosa are usually located in the longitudinal direction.
Intrauterine septum. Hysteroscopy allows you to clearly identify the presence and nature of the intrauterine septum. It is defined as a fibrous cord dividing the uterine cavity into two parts, each of which, tapering towards the distal part, ends at the mouth of the fallopian tube. The mucous membrane in the area of the septum is devoid of folds, thinned and paler in comparison with the mucous membrane of other parts of the uterus.
Intrauterine adhesions (synechia). They are determined by hysteroscopy as fibrous, avascular cords of varying density and length, often reducing the uterine cavity and closing the uterine angles.
There are several types of intrauterine synechiae: endometrial-endometrial adhesions, myofibrous and connective tissue adhesions.
Intrauterine adhesions come in three degrees:
I degree - at least 1/4 of the uterine cavity is involved, the fundus and orifices of the tubes are free.
II degree - 1/4-3/4 of the uterine cavity is involved, the fundus and orifices of the tubes are partially closed.
III degree - more than 3/4 of the uterine cavity is involved.
After the operation is completed and the scraping is removed from the uterine cavity, a control hysteroscopy is necessary.
Complication of gynecological cleansing
The professional actions of a doctor and anesthesiologist rarely lead to any complications.
However, there may be the following consequences:
- Perforation of the uterus (damage to the walls). It is theoretically possible to pierce the wall of an organ with any of the instruments used. Statistics show that they are more often perforated with a dilator or probe. This occurs when the cervix cannot dilate easily and excessive pressure is applied to the dilator. Or the structure of the uterine walls itself is loose and easily injured. If such an injury occurs, then thanks to special treatment, minor injuries heal on their own, and large ones are sutured.
- Cervical tear. If the fixing pliers fly off, a similar injury may occur. This is not always a doctor’s mistake; the cervix is sometimes loose, and it is difficult to hold the instrument—fixing forceps—on it. Treatment involves stitching a large tear, and a small one will heal on its own.
- Inflammation of the uterus. Such a complication is possible when there was inflammation, or violations of septic and antiseptic requirements were committed. For treatment, a course of antibiotics is prescribed. Typically, such a course is prescribed for the purpose of prevention.
- Hematometra. This is an accumulation of blood in the uterine cavity. Normally, after surgery, blood gradually comes out. But if a spasm of the cervix occurs, the blood remains inside and causes inflammation, which is accompanied by pain. This complication is treated therapeutically, and bougienage of the cervix may also be prescribed to relieve spasm.
- Damage to the mucous membrane. If the doctor scraped excessively and roughly, he could damage the germ layer of the mucous membrane. And this leads to the fact that the mucous membrane stops growing and regenerating. This is the worst complication because it cannot be treated.
- Incomplete removal of tumors and polyps. If something remains, then the pathological process continues. Requires re-cleaning. More often this happens when hysteroscopy is not used and curettage is performed blindly.
In general, such complications rarely occur if the operation is performed by competent and experienced doctors.
After surgery, a course of antibiotics is usually prescribed to prevent inflammation.
Spotting and spotting lasts from 3 to 10 days after surgery. If this does not happen, there is no discharge, you need to contact your doctor to prevent complications in the form of a hematomera. To prevent this complication, nosh-pa tablets may be prescribed.
After surgery, it is advisable to rest more and reduce physical activity to a minimum. You should be alert to such manifestations as increased body temperature, severe bleeding, severe pain in the pelvis, and a putrid smell of discharge.
Headaches, muscle pain, and panic attacks may result from the body's reaction to anesthesia.
Postoperative period
After a hysteroscopy, women may experience mild cramping and spotting for two to five days after the hysteroscopy. The doctor may prescribe painkillers and antibiotics for 5-7 days.

To minimize the risk of infection or the development of an inflammatory process, the use of tampons and douching should be avoided. After diagnostic hysteroscopy, patients are also advised to abstain from sexual intercourse for two days.
After surgical hysteroscopy, the period of abstinence ranges from one to three weeks, depending on the extent of the surgical intervention performed.
Why do gynecological cleansing?
Gynecological cleansing is prescribed in the following cases:
- prolonged bleeding with the presence of blood clots;
- bleeding between periods;
- incomplete removal of the fertilized egg during abortion;
- frozen pregnancy, miscarriage;
- infertility;
- endometriosis;
- polyps, fibroids;
- changes in the uterine mucosa, changes in the cervix.
Cleaning is also prescribed when it is necessary to obtain biomaterial for research - mucous membrane from the walls of the uterus.
Treatment after curettage
A large number of women, after curettage, feel pain in the lower abdomen during menstruation. This is a fairly common situation, so to reduce pain and prevent the accumulation of blood clots in the uterus, the doctor may prescribe antispasmodics - for example, no-spa. It is taken one tablet three times a day.
Quite often, to prevent various infections from entering the body and for a quick recovery, doctors prescribe antibiotics. To prevent severe uterine bleeding that may occur after the procedure, the gynecologist may prescribe the patient a course of oxytocin injections. Two weeks after the operation, you must visit the doctor for a re-examination.
Within 14 days after curettage, sex, douching, the use of vaginal tampons, and heavy physical activity are contraindicated.
Scraping
Gynecological cleansing during frozen pregnancy
Gynecological cleansing in the event of a frozen pregnancy is the most reliable way to remove a dead embryo. Used for many years all over the world. However, the appropriateness of this procedure is determined by the doctor.
A frozen pregnancy is also determined by a doctor based on indications.
Cleaning is carried out on a gynecological chair using general or local anesthesia. The patient does not feel pain or discomfort. She falls asleep during the procedure and wakes up in the ward after all the manipulations.
The doctor’s task is to remove the dead embryo before infection of the woman’s blood begins. Curettage is performed using a curette inserted into the uterine cavity.
Before the operation, the woman donates blood for analysis, and also undergoes an ultrasound examination, possibly MRI and fluorography.
After a high-quality operation, the woman’s health is completely restored within a month.
The rehabilitation period depends not only on the quality of the operation performed, but also on the state of health of the woman herself and on the duration of the frozen pregnancy. The shorter the period, the lower the risk of complications.
In what cases is hysteroscopy necessary?
Hysteroscopy is performed in many cases related to the following points:
- with bloody discharge;
- in case of menstruation failures;
- for infertility, before IVF;
- while taking hormonal drugs to determine their effect on the body;
- to determine the location of the intrauterine contraceptive;
- for postpartum complications;
- for some diseases and complications.
So, a woman came to the clinic with a complaint, and after examining her, a specialist concluded that it was necessary to use hysteroscopy in this case. After this, the woman must undergo tests that will allow us to conclude that there are contraindications.
Testing is also important to identify any infections that may enter the uterus, since the path of the hysteroscope passes through the vagina and cervix - elements of the reproductive system with its own microflora.