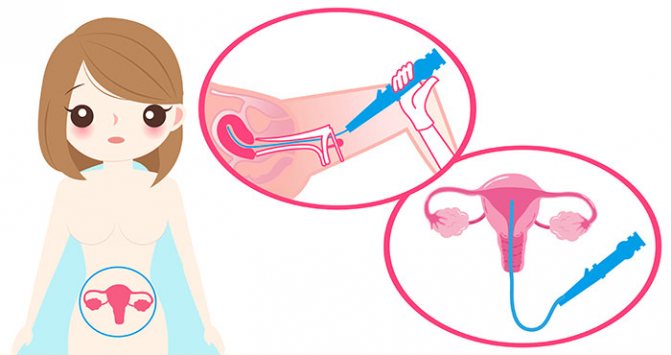
Hysteroscopy of the uterus is both a diagnostic and therapeutic procedure that allows you to examine the uterine cavity from the inside and, if necessary, perform various medical procedures, for example, remove foreign bodies, polyps, etc. Hysteroscopy is performed using special instruments that are inserted through the vagina.
- Types of hysteroscopy of the uterus
- Indications for performing hysteroscopy of the uterus
- How to prepare for hysteroscopy of the uterus
- How is hysteroscopy performed?
- Contraindications
- Recovery after hysteroscopy of the uterus
- What complications can hysteroscopy cause?
- What procedures can a gynecologist perform during hysteroscopy?
- When can hysteroscopy be performed?
- Risks of hysteroscopy
- What alternatives are there to hysteroscopy?
Types of hysteroscopy of the uterus
- Diagnostic hysteroscopy. As the name implies, this procedure does not involve therapeutic interventions. During diagnostic hysteroscopy, only a visual examination of the internal cavity of the uterus and cervical canal is performed using a special optical system. Since no surgery is performed, significant anesthesia is not required. In most cases, local anesthesia and sedation are sufficient. The recovery period after the procedure is short. No hospitalization required.
- Surgical hysteroscopy is already a therapeutic and diagnostic intervention. It allows you to detect the problem and immediately treat it. This procedure is prescribed when the diagnosis has already been established, or in cases where its probability is maximum. This is already a full-fledged operation, albeit a low-traumatic one. It requires anesthesia and is therefore performed in a hospital setting.
- Control hysteroscopy. It is carried out to monitor the condition of the uterus after surgical treatment.
Hysteroscopy of the uterus for polyp removal: postoperative period
Reviews about this procedure are mostly positive. The postoperative period after hysteroscopy of the uterus to remove a polyp passes quickly and is rarely accompanied by complications. Most often, the patient can go home on the same day. In some cases, hospitalization for up to 3 days is possible.
After the procedure, at first you may feel pain and cramping in the abdomen, which should go away soon. Bleeding may occur and is considered normal to last up to a week. If they do not go away 7 days after surgery, you should inform your doctor.
A control ultrasound is performed 3-4 days after the procedure. The doctor evaluates the condition of the uterus and endometrium after hysteroscopy.
To eliminate the cause of the pathology and prevent its relapse, hormone therapy is prescribed. It is not indicated for all women and is compiled individually. Treatment may include oral contraceptives, a hormonal intrauterine device, and other hormone-containing drugs.
Indications for performing hysteroscopy of the uterus
- Infertility of unknown etiology.
- Habitual miscarriage.
- Polyps of the uterus and cervical canal.
- Foreign bodies in the uterine cavity, for example, intrauterine contraceptives.
- Pathology of the endometrium - hyperplasia, synechiae.
- Suspicion of uterine malformations.
- Metrorrhagia is non-cyclic uterine bleeding.
- Bleeding after menopause.
Currently, there is a trend away from carrying out invasive techniques purely for the purpose of examination, since this is one way or another associated with certain risks, and the necessary information can often be obtained using safer methods. The same applies to diagnostic hysteroscopy. The procedure is prescribed only if it is impossible to establish a diagnosis using other non-invasive methods.
Book a consultation 24 hours a day
+7+7+78
Endometrial polyp
The uterine cavity is lined by the mucous membrane. This is the superficial layer of glands and connective tissue. As a result of various disorders, cells in one area begin to rapidly divide and a bulge appears. As it grows, a rounded body forms on an elongated thin stalk. This is a polyp. Sometimes it reaches such a length that it simply does not fit inside the uterus, then the tip can protrude from the opening of the cervical canal. Although formations are also formed there.
What causes polyps?
The reasons for the appearance are not completely clear, however, there are a number of factors that can provoke pathology:
- Abortion;
- Gynecological operations;
- Birth with ruptures;
- Inflammatory diseases of the uterus;
- Sexual infections.
In most cases, polyps occur against the background of an imbalance in the endocrine system, when there is a lack of progesterone and an excess of estrogen. This situation is typical for overweight patients with diabetes.

Attention! Scientists have identified a special gene that is responsible for the appearance of polyps, so the predisposition is inherited.
Classification
Types of formations in the uterus:
- Adenomatous are characterized by disturbances in the structure of cells and their internal elements. After some time, such a growth can become a malignant tumor;
- Fibrous formations are very dense because they consist of connective tissue. Occurs in women after 40 against the background of hormonal changes before menopause;
- Glandular polyps are soft, mobile, and resemble jelly. Rarely reach large sizes above 10 mm. Diagnosed in women under 30 years of age. Sometimes amenable to drug treatment;
- Glandular-fibrous formations contain equal parts connective tissue and endometrial glands. They often become inflamed, grow quickly, and are prone to bleeding. Such polyps are found in patients in the prime of reproduction - from approximately 25 to 35 years;
- Placental formations are a postpartum complication when parts of the baby’s place remain in the uterine cavity. From these fragments a polyp is formed, covered with connective tissue. Similar chorionic formations are built from the remains of the chorion, the precursor of the placenta after a miscarriage or early abortion;
- Decidual polyps occur during pregnancy. This is hyperplasia of the layer surrounding the amniotic sac. Does not require treatment. The problem resolves itself during childbirth.
Attention! Only histological examination can classify the formation with reliable accuracy.
Symptoms
Signs of pathology occur when the polyp reaches a size of more than 1-1.5 cm. The formation is injured, which leads to contact bleeding, especially for growths protruding from the cervical canal. During sexual intercourse or gynecological manipulations, the polyp is damaged and a little blood appears. Physical activity, such as lifting weights, can trigger discharge. In addition, a woman's menstrual cycle is disrupted. Menstruation is larger in volume and time. Education leads to pain during this period.

One of the signs of pathology is infertility. Polyps are often found by chance when trying to find out the cause of problems with conception. This does not mean that growths in the uterus are the cause of infertility. The eggs mature and can be fertilized, but the polyp interferes with this process and also provokes contractions of the myometrium, which leads to rejection of the embryo. Therefore, miscarriages occur in the early stages.
Discharge in the presence of a polyp in the uterus and cervical canal
This type of formation is accompanied by increased production of mucous secretions, so a woman may notice white or transparent odorless discharge. Combination with blood results in pink or brownish leucorrhoea.

If an unpleasant aroma appears, a yellowish-green color, a foamy structure, or an increase in volume, then this is a sign of infection. This can be indicated by very thin gray-green discharge with a musty odor.
Carefully! Black clots in a woman during menopause may indicate an oncological tumor.
How to prepare for hysteroscopy of the uterus
Hysteroscopy of the uterus is an invasive procedure that carries certain risks. To minimize them, it is necessary to undergo examination and, if indicated, treatment. As part of the examination, the following tests are prescribed:
- General and biochemical analysis of blood and urine.
- Smear for flora and oncocytology (if not performed within the last year).
- Test for STIs.
- Coagulogram.
- Determination of blood group and Rh factor.
- ECG.
- Determination of markers of infectious diseases: HIV, parenteral hepatitis, syphilis.
If inflammatory gynecological processes are detected, sanitation is carried out.
Hysteroscopy is planned in accordance with the menstrual cycle. It is recommended to perform the procedure in the first days after the end of menstruation, since during this period there is no growth of the endometrium and it is easier to detect its pathology. However, if there are absolute medical indications, the procedure can be performed on any day of the cycle. Immediately before hysteroscopy, you must adhere to the following rules:
- Avoid vaginal sex 1-2 days before the scheduled procedure.
- The last meal should be at least 6 hours before the start of the intervention. This condition is necessary for safe anesthesia. Anesthesia can lead to muscle relaxation and the flow of gastric contents into the airways. This is fraught with the development of asphyxia or aspiration pneumonia, which is difficult to treat.
- You will need to shower on the day of surgery.
- Before the operating room, you must empty your bladder and remove jewelry, dentures, and contact lenses.
Removal of polyps using radio waves
Treatment with Surgitron is carried out in the first ten days of the cycle, best of all - immediately after menstruation. When treating after childbirth, you must wait until the bleeding stops.
Before the procedure, the doctor administers local anesthesia to reduce discomfort. The manipulation takes one to ten minutes. If the pain threshold is low or the number of polyps is large, the procedure may take longer.
After evaporating polyps with Surgitron, hospitalization is not required. The patient can return to her normal rhythm of life almost immediately.
How is hysteroscopy performed?
An hour before the patient is admitted to the operating room, premedication is administered, the purpose of which is to reduce anxiety, increase tolerance to anesthesia and reduce the secretory activity of the glands. For this purpose, a combination of drugs is prescribed, containing narcotic analgesics, antihistamines, anticholinergics and sedatives.
In the operating room, the patient is placed in a gynecological chair and anesthesia is administered. The type of anesthesia is discussed in advance, taking into account contraindications, recommendations of the anesthesiologist and the wishes of the patient.
Next, proceed directly to hysteroscopy:
- The cervical canal is expanded using special instruments.
- A sterile liquid or gas is injected into the uterus through an enlarged canal. This is necessary to expand its cavity and make it accessible for inspection and manipulation.
- Next, a hysteroscope is inserted through the cervix - a thin tube with a diameter of about 5 mm with an optical system that transmits an enlarged image to the monitor. As it is introduced, the cervical canal, intrauterine cavity and its angles are examined.
- After the diagnosis has been established, treatment is carried out using the same hysteroscope, which has a special channel for inserting surgical instruments. In this way, removal of polyps, submucosal myomatous nodes, dissection of synechiae, curettage of the endometrium, etc. can be carried out.
- After all interventions are completed, the hysteroscope and the injected liquid or gas are removed. The patient is sent to the intensive care ward, where she recovers from anesthesia under the supervision of medical staff.
Recovery after hysteroscopy of the uterus
The recovery period after hysteroscopy is divided into two stages. In the early recovery period, tissues damaged during the procedure are restored—the mucous membrane of the uterus, the muscular wall, and the cervical canal. This period lasts about 2-3 weeks.
The second period takes about six months. At this time, the new endometrium will be regenerated, which must meet the functions assigned to it - grow and be rejected in the process of changing the phase of the menstrual cycle.
Bloody discharge after hysteroscopy
Moderate bleeding is possible in the first 2-3 days after hysteroscopy. This is normal, since during the procedure the cervical canal, endometrium and muscular layer of the uterus are injured. Gradually, the discharge lightens, acquires a yellowish color and continues for about 2-3 weeks. If heavy bleeding develops, you should immediately consult a doctor, as this may be a symptom of serious complications.
Painful sensations after hysteroscopy
Mild to moderate pain after hysteroscopy is normal. They are localized in the lower abdomen and can radiate to the sacrum or lower back. They arise due to stretching of the uterine cavity and injury to the cervix. To alleviate the condition, it is recommended to prescribe “strong” NSAIDs such as ketorol or indomethacin. If the pain increases and becomes unbearable, you should seek medical help immediately, as this may be a sign of serious complications.

In order for the recovery period to go smoothly, you must adhere to several rules:
- Take all medications prescribed by your doctor. As a rule, we are talking about antibiotics that are prescribed prophylactically to prevent the development of infections.
- Avoid vaginal sex until your next period.
- During the period of bleeding, it is better to use pads. Tampons are strictly prohibited.
- Also, during the recovery period it is not recommended to use vaginal suppositories, tablets and creams.
- Refrain from intense physical activity.
- Don't forget about personal hygiene. Toilet of the genital organs should be performed at least 2 times a day, and ideally after each urination and defecation.
- To prevent the development of constipation, follow your diet. Don't forget to empty your bladder in a timely manner.
After hysteroscopy, the polyp grew again
What to do if the polyp grows again after surgery? Polyps often appear due to hormonal imbalance in a woman’s body. Removing a polyp does not guarantee the cessation of their formation elsewhere in the uterine mucosa. Endometrial polyps are a disease characterized by the proliferation of the basal (inner) layer of the endometrium. The most common cause of the development of polyps is an excess of estrogen, a lack of progesterone; abortion, premature termination of pregnancy, and childbirth with incomplete delivery of the placenta can also cause the growth of polyps. It is possible to develop polyps after stress, with diseases: diabetes, thyroid disease, hypertension. Chronic inflammatory processes in the female genital area and a sharp drop in immunity play a negative role. If the polyp has grown again, you should be tested for sex hormone levels. When hormone levels are disrupted, polyps will reappear even after surgery. In this case, treatment with OCs (oral contraceptives) is prescribed, which will affect hormonal levels and stop the development of polyps. If hysteroscopy was used to remove a polyp, bloody discharge will persist for several days. You should monitor the condition of the discharge - it should not be abundant, change color, or have an unpleasant odor. If such symptoms appear, consult a doctor immediately.
What complications can hysteroscopy cause?
As with any invasive intervention, complications may develop after hysteroscopy. The most formidable and dangerous of them is perforation of the uterine wall, which is accompanied by bleeding. To eliminate the perforation, repeated surgery is required to suturing the defect. If left untreated, peritonitis may develop.
There may also be other complications:
- Hematometra is the accumulation of blood in the uterine cavity due to the impossibility of its drainage. Clinically manifested by increasing spasmodic pain in the lower abdomen and deterioration in general well-being. For treatment, conservative methods can be used (prescription of drugs that improve uterine contraction or antispasmodics for pathological contraction of the cervix), or surgical methods, in which repeated intervention is performed with evacuation of the intrauterine contents.
- Infectious complications. They are manifested by an increase in body temperature, symptoms of intoxication, and pain in the lower abdomen. A little later, pathological discharge appears, which may have a foul odor.
- Bleeding. Possible after therapeutic hysteroscopy, when, for example, myomatous nodes or polyps are removed. If you experience heavy bleeding, especially if it lasts several days, you should consult your doctor.
In general, hysteroscopy is a low-traumatic intervention and the likelihood of complications after it is much lower than with other, more extensive treatment methods.
Normal discharge
After hysteroscopy, scanty discharge from ichor and mucus usually appears. Their characteristics and appearance depend on the type of study, blood clotting, existing diseases and the ability of tissues to regenerate. If only the uterus is examined, then after the procedure there is little discharge. They are usually watery and streaked with blood. When a smear or scraping is taken from the endometrium, smearing fractions may appear.
A special feature of hysteroscopy is the ability to remove small tumors. Like any surgical intervention, this is always accompanied by tissue damage and bleeding. However, with hysteroscopy it is small.
If polyps, various neoplasms, and fibroids are removed during the procedure, this is accompanied by bright red discharge. This is normal, since after tissue damage the vessels bleed for some time. The discharge after hysteroscopy is at first very similar to menstruation, but after a few days it will turn brown, which indicates healing.
The norm includes several situations when factions appear
| Type of hysteroscopy | Characteristics of discharge are normal |
| Removal of polyps | The discharge may be bloody or watery with ichor. It depends on the excised tumor: 1. If the polyp is on a thin stalk, then almost transparent, slightly blood-stained mucus comes out. Disappears on its own within 3 days. 2. When a polyp with a thick stalk is removed, slight bleeding occurs. After a couple of days, it turns into watery mucus or smears. 3. Removal of a polyp with a wide base is accompanied by the release of approximately 50 ml of blood in the first three days. There is no reason for alarm, even if a clot comes out in the first 24 hours after hysteroscopy. The blood could simply have clotted, which often happens after a polyp is removed. |
| Scraping | After it, the discharge is similar to menstrual. During curettage, the entire inner surface of the uterus is damaged and after the procedure it appears as a large open wound. Naturally, this is accompanied by bleeding and mucus release. Normally, this process lasts up to five days, much less often – up to ten. During this time, the bleeding gradually stops and eventually turns into a brown spot. |
It is also normal when there is little discharge during survey hysteroscopy. If they are not present at all, then this indicates a minor gynecological problem. For example, uterine spasms, when its contents do not come out, but accumulate. The same happens with atony due to clots blocking the cervical canal. Then the scraping is done again.
What procedures can a gynecologist perform during hysteroscopy?
Hysteroscopy is a diagnostic procedure, however, during it some additional manipulations can be performed, including therapeutic ones:
- Biopsy is a procedure during which a piece of pathologically changed tissue is removed and sent to the laboratory for histological and cytological examination. This allows you to establish a more accurate diagnosis, confirm or exclude the presence of a malignant tumor in the uterus.
- Hysteroscopy allows you to remove various pathological formations protruding into the uterine cavity, such as polyps and fibroids.
- The source of bleeding can be eliminated using electrocoagulation and low temperature (cryosurgery).
- Place contraceptive devices in the fallopian tubes.
The Euroonko clinic in Moscow offers special comprehensive programs for women, for example, hysteroscopy with separate diagnostic curettage of the cervix and uterine body. The cost of the service includes a 6-hour stay in a comfortable hospital, meals, and all related procedures.
When can hysteroscopy be performed?
Most often, gynecologists prescribe hysteroscopy in the following situations:
- Detection of atypical cells based on PAP test results.
- Vaginal bleeding between periods, postmenopause.
- Infertility is when you cannot get pregnant after a year of regular sexual activity.
- Frequent miscarriages.
- The need to clarify the condition of the uterus with scars and fibroids.
- The need to confirm or rule out certain diagnoses using biopsy.
Risks of hysteroscopy
Overall, this is a safe procedure. For two days after hysteroscopy, you may experience slight bleeding from the vagina and cramps in the lower abdomen - this is normal. More serious complications are very rare, occurring in no more than 1% of cases.
At Euroonko, the research is carried out by a highly qualified specialist - Natalya Evgenievna Levchenko, oncogynecologist, professor, doctor of medical sciences. The clinic uses equipment for hysteroscopy from the world's leading manufacturers, which allows the examination to be carried out as comfortably and safely as possible.
What alternatives are there to hysteroscopy?
Hysteroscopy can be replaced by some other diagnostic procedures, but not in all cases:
- Transabdominal ultrasound of the pelvic organs through the anterior abdominal wall helps to identify diseases that lead to pelvic pain, menstrual irregularities, vaginal bleeding, and infertility.
- Transvaginal ultrasound is performed with a special probe inserted through the vagina. It allows you to obtain more informative images of the uterus and its appendages.
- Aspiration biopsy of the myometrium. This procedure does not require hysteroscopy: using vaginal speculum, the cervix is visualized and a tube connected to an aspirator is inserted through it.
All these studies are not as informative as hysteroscopy. However, if you start the diagnosis with them, in some cases endoscopic examination of the uterus may not be required. Sometimes these diagnostic methods are used as an alternative if there are contraindications for hysteroscopy for one reason or another.
Book a consultation 24 hours a day
+7+7+78
Contraindications
The study is not carried out if:
- inflammatory diseases of the pelvic organs in the active phase, or during exacerbation of chronic diseases;
- general diseases (acute or chronic during exacerbation);
- diseases of the liver, kidneys, lungs, heart (severe);
- desired intrauterine pregnancy;
- ectopic pregnancy;
- submucosal (submucous) uterine fibroids more than 5 cm;
- common cervical cancer;
- blood clotting disorders.