STIs have been known to humanity since ancient times, but over time the number of cases of infection does not decrease, but rather increases. As “familiar” infections are overcome, new ones appear. Almost every person is at risk, regardless of gender and social status.
Modern medicine lists about 30 infections that can be classified as STIs. Most of them can be asymptomatic, and this makes them very dangerous for the health of various organs and systems.
Reasons for the spread of STIs
- the lifestyle of modern people (promiscuous sex, frequent changes of partners, smoking, alcohol abuse), which creates favorable conditions for infection;
- unfavorable environmental conditions, decreased quality of food, high levels of stress negatively affect the functioning of our immune system, facilitating the task of pathogenic microorganisms;
- The general availability of antibacterial drugs in pharmacies and information about recommended treatment regimens on the Internet often leads to patients self-medicating.
I want to talk about the last reason separately! Incorrect self-prescriptions transfer the course of the disease from the acute stage to the chronic stage, which is difficult to detect and subsequently treatable.
In light of the above, I ask you to entrust the prescription of medications, even the most harmless ones, to professionals who have basic and specialized knowledge, who care and regularly improve their level of knowledge.
Incorrect regimens and long-term use of the same drug have already led to the fact that many drugs that have proven themselves to be successful in the past are no longer able to perform their functions. The scientific community is talking about the beginning of the “era of antibiotic resistance” - the immunity of microorganisms to antibiotics, which makes us think about the search for new effective methods of treating infectious diseases.
Nowadays, there are no longer diseases caused by just one microorganism!
Therefore, there is almost always a need for an integrated approach to prescribing therapy, with the goal of simultaneously influencing all pathophysiological processes. It is in order to obtain complete information about you that a medical examination is necessary, which, unfortunately, cannot be performed within the framework of telemedicine.
Basics of polymerase chain reaction
The PCR method is carried out exclusively in laboratory conditions. To carry it out, special enzymes are used that increase the structure of the patient’s DNA and RNA several times. Such a quantity of DNA and RNA must be formed so that visual analysis can be carried out. During the examination, the section of RNA or DNA that is ideally suited to the required conditions is copied.
The laboratory has a corresponding database, which indicates the exact structure of various infectious agents. Thanks to the PCR method, you can not only see the pathogen, but also calculate its quantitative ratio.
PCR diagnostics also involves certain innovations, among which are the following:
- introduction of mutations;
- connection of individual DNA fragments;
- determination of paternity, etc.
A common problem when self-medicating STIs
When pathological discharge from the genital tract appears, the first thing patient N does, deciding that she has an exacerbation of thrush, independently uses suppositories, which:
- once helped in a similar situation;
- recommended by friends;
- were advertised on the Internet.
Will the smear required by the doctor to make a diagnosis, performed after using the drug, be adequate? Of course not! And now, if an antibiotic was used, a break from using the drug for 14 days is necessary to obtain biomaterial and make a diagnosis!
And patient N has itching and burning (the drug did not help, otherwise she simply would not have come)! So it turns out that the doctor is forced to treat the disease he suspects, based on the patient’s complaints, which is unacceptable in the 21st century.
Dear girls, women, pathological discharge from the genital tract can hide not only thrush (vulvovaginal candidiasis), bacterial vaginosis and aerobic vaginitis, but also STIs that cannot be treated with “thrush” suppositories!
Decoding the analysis results
If you follow the recommendations, errors in the results of the PCR analysis are practically eliminated. Preparation of results can take up to 2 days, but in some modern laboratories the tests are ready within one working day.
The results of the PCR-12 analysis can be positive or negative. A negative result indicates that no infection has been detected. A positive result means that the test material contains infectious elements, and the patient requires high-quality treatment. Also, the result can be positive if you are a carrier of the infection, but there is no need to carry out therapeutic measures. What infections are included in PCR-12 and can be examples of such diseases? These include human papillomavirus infection, herpes and other diseases. However, it is important to know that a person who is a carrier can infect healthy people, even if he himself is not bothered by the disease.
If the analysis results in indicators with positive values, you must consult a doctor to prescribe effective therapy. There are situations when PCR shows a questionable result, in which case a repeat test should be done after 12-14 days.
In addition to qualitative characteristics, PCR analysis can also have quantitative characteristics. Using quantitative characteristics, a specialist can determine the activity, stage of development of the disease and choose the most suitable drug for treatment.
What is the danger of STIs?
The clinical manifestations of most STIs are nonspecific (do not have features characteristic of a particular disease), and no doctor can make a correct diagnosis without the use of laboratory research methods. Therefore, it is best to carry out diagnostic tests when complaints arise, the scope of which, based on your complaints and examination data, will be determined by the doctor.
The danger of STIs lies, first of all, in the formation of adverse consequences for a woman’s reproductive health.
Thus, infertility develops in 1 out of 12 cases of a single infection, in 1 out of 5 after the second episode, and in every second after the third episode. Ectopic pregnancy always occurs due to inflammation of the female genital organs. I'm not even talking about pelvic pain, menstrual irregularities and other consequences that often remain even when the pathogen is no longer present.
References
1. Federal clinical guidelines. Dermatovenereology 2015: Skin diseases. Sexually transmitted infections. — 5th ed., revised. and additional - M.: Business Express, 2021. - 768 p. 2. Malova I.O., Primak N.B., Afanasyeva I.G., Zinovieva T.K. Acute vulvovaginal candidiasis: an old problem - a new solution. Clinical dermatology and venereology. 2012;10(4) 3. Belyaeva N.R. CYTOMEGALOVIRUS INFECTION AND REPRODUCTIVE HEALTH OF WOMEN. Journal of Obstetrics and Women's Diseases. 2016; 4, pp. 24 – 33.
List of STIs
STIs include:
- syphilis,
- gonococcal infection,
- urogenital chlamydial infection,
- urogenital trichomoniasis,
- anogenital herpetic viral infection,
- HPV (read more in the article “HPV discovered!”),
- HIV infection (infection caused by the human immunodeficiency virus),
- viral hepatitis.
Very often, when asked about past STIs, I hear the answer: “I was in the hospital and they checked me for all infections, they said that everything was fine.” Yes, that’s right, everything is fine, otherwise you would have been informed, but a negative result indicates the absence of HIV, syphilis and viral hepatitis - these are the tests that a person takes when hospitalized in a hospital, undergoing routine medical examinations, or any type of surgical intervention. But not more!
Most of the girls who have yet to become mothers, having more than one sexual partner, have never been tested to detect pathogens such as Chlamydia trachomatis and Mycoplasma genitalium - proven culprits of pelvic inflammatory diseases, infertility and ectopic pregnancies.
The incidence of infertility with previous and untreated chlamydial infection is 50%, and with infection with Mycoplasma genitalium - more than 30%.
I express my opinion: every new sexual partner can potentially be a source of infection, so you should carefully choose the person with whom you are going to have, I emphasize, any type of sexual contact. It is ideal to know about the state of his health in advance, as well as your own. But if the matter has already been done, it makes sense to check whether you have been given an STI, especially if you are planning to have children. And please do not forget that each infection has its own incubation period (until the moment of clinical manifestations and, as a rule, until it can be detected using laboratory diagnostics), which will depend not only on the pathogen, but also on the characteristics of the immune system human body.
With a high degree of probability, it is possible to establish the presence or absence of chlamydia, mycoplasma, trichomonas, gonococcus, Treponema pallidum (the causative agent of syphilis) and even HIV (human immunodeficiency virus) and viral hepatitis agents a month after unprotected contact. But the fact of infection with the human papillomavirus can be established for sure 3 - 6, or even 9 - 12 months after the moment of infection.
What infections are included in PCR-12
STIs develop as a result of the influence of opportunistic and pathogenic microflora on the organs of the genitourinary tract. Using the PCR method, it is possible to detect diseases that occur in both acute and chronic forms, and also long before the first symptoms of the disease appear. Patients are often interested in the question of what infections are included in PCR-12? Let's list these diseases:
- Gardnerellosis.
- Chlamydia (caused by the species Chlamydia trachomatis).
- Mycoplasmosis (caused by mycoplasmas hominis or genitalium).
- Gonorrhea.
- Candidiasis (caused primarily by the fungi candida albicans).
- Ureaplasmosis.
- Herpes types 1 and 2.
- Trichomoniasis.
- Human papillomavirus (including analysis of HPV types 16 and 18).
- Cytomegalovirus.
- Analysis for hepatitis of different groups.
- HIV infection.
An HIV test using PCR can detect infection within 3-4 weeks.
Gynecological smear as a method for detecting STIs
Every year, I hope, we all undergo a “flora smear” - an examination under a microscope of discharge from the urethra (urethra), cervical canal, cervix and vagina for the detection of pathogenic microorganisms (Neisseria gonorrhoeae, Trichomonas vaginalis), conditionally pathogenic (streptococci, staphylococci, enterococci, fungi of the genus Candida) and assessment of the predominant flora, which normally should be lactobacillary. Also, during microscopy, the number of leukocytes is determined; ideally, their number should not be more than 10 units in the discharge of the urethra, 20 from the vagina and 10 from the cervical canal. It is possible to identify key cells (vaginal epithelial cells surrounded by opportunistic microorganisms), frequent companions of bacterial vaginosis (Figure 1).
Figure 1 - Gynecological smear (collection tools and microscope view)
Let me remind you that the test is taken during the absence of bleeding, it is advisable not to have sexual intercourse for 1 - 2 days, and also not to insert suppositories, to take the test before a vaginal ultrasound examination. And, of course, don’t douche! I urge you not to do this at all!
So, microscopy of a gynecological smear can reveal gonorrhea and trichomoniasis. Unfortunately, this is not the entire list of STIs.
Meanwhile...
World statistics total 357,000,000 new registered cases of STI infection per year, which corresponds to 1,000,000 cases of infection per day!
The leading positions are occupied by trichomoniasis (about 142,000,000 cases of infection annually) and chlamydial infection (about 131,000,000 cases).
Contrary to popular belief about the low prevalence of gonorrhea and syphilis, statistics indicate 78,000,000 cases of infection with gonorrhea and 6,000,000 with syphilis annually.
What are the advantages and disadvantages of PCR diagnostics of infections?
Benefits of the study:
- you can study any biological material (epithelial cells, blood, urine, saliva, sperm, secretions, etc.);
- traces/parts of the infectious agent itself are detected, and not the products of its decay or the body’s responses;
- identification of a DNA fragment corresponding only to this specific pathogen;
- it is possible to detect only a few cells (preferably about 10 – 100 in the sample);
- the entire study takes no more than 5 hours;
- It is possible to diagnose both acute and chronic and asymptomatic forms of diseases, etc.
Relative disadvantages:
- not the cheapest method;
- does not allow to establish whether a living or non-living pathogen is detected;
- the detected microorganism is not guaranteed to be the cause of existing problems (due to high sensitivity, even minimal, clinically insignificant quantities are detected);
- false positive/false negative results are possible;
- places high demands on the accuracy of the technique and the qualifications of the personnel.
Who needs to be tested to identify STI pathogens?
- to both sexual partners at the stage of pregnancy planning,
- pregnant women,
- sexually active girls who want to become mothers in the deferred period,
- women who have had unprotected contact with a dubious partner,
- women who frequently change sexual partners,
- partners of persons infected with STIs,
- patients with inflammatory diseases of the pelvic organs and their sexual partners,
- patients with pathological discharge from the genital tract,
- patients with infertility and pregnancy loss,
- patients undergoing surgical interventions on the pelvic organs.
In this article I will briefly touch on bacterial infections that are in the department of gynecologists; STIs of viral etiology are discussed in separate articles (“HPV has been detected!” and HSV – I will write soon). Gonorrhea and syphilis are the domain of dermatovenerologists, while HIV and viral hepatitis are treated by colleagues who are infectious disease specialists.
Indications for prescribing PCR-12
PCR for twelve infections is carried out in the presence of symptoms of an inflammatory disease in the organs of the reproductive system or for preventive purposes. Considering what infections are included in PCR-12, the analysis can be prescribed by a urologist, gynecologist, or venereologist. Common reasons for getting tested:
- Suspicious or unpleasant symptoms. These symptoms include painful urination, itching, rashes, sores, or unusual genital discharge. It is a mistake to believe that STIs cannot be contracted through other means. This is a misconception - partners can be healthy and faithful to each other, but the infection occurred through sexual contact. The probability of this is small and does not exceed 5%, but this is still significant. For example, you can become infected with gonorrhea by using someone else's towel. The risk increases when living together with a carrier of the infection. Therefore, the household method of infection with pathogenic microorganisms should also not be excluded. It is important to contact a specialist promptly if you have any alarming symptoms. The period from the moment of infection to the appearance of the first symptoms can last from several days to a couple of weeks or even months. But it is also important to remember that the disease can also be asymptomatic.
- A large number of sexual partners and neglect of barrier contraception. In this case, it is recommended to carry out annual diagnostics to find out whether dangerous infections are present in the body.
- Conducting examinations when planning pregnancy. Every couple is recommended to undergo a PCR test before conception. This method will identify hidden diseases that can be transmitted from mother to child during pregnancy and childbirth and prevent infection.
- Infertility. Sexually transmitted infections can lead to fertility problems. If you are unable to conceive within a year under conditions of an active sexual life without contraception, it is recommended to do PCR for twelve infections.
- Surgeries on the bladder, prostate, uterus, ovaries and other pelvic organs. During surgery, the presence of infections can be very dangerous as they can lead to complications after surgery.
If at least one of the above symptoms is present, it is recommended to use the PCR diagnostic method. Infectious diseases that are not detected and treated in time can lead to serious complications, such as prostatitis, epididymitis in men and vaginitis, adnexitis in women. The causes of infertility in men and women in more than half of cases are STIs.
Chlamydia infection
In the Russian Federation in 2015, 41.3 cases of chlamydial infection were registered per 100,000 population, which, in comparison with the average in Europe - 184 cases per 100,000 population, indicates (according to leading experts of the Russian Federation) not about the real incidence, but that most infected people do not go to medical institutions for help, since in most cases the infection is asymptomatic.
When analyzing the incidence rate depending on age, the highest is in the category of young people: 44.7 per 100,000 in the age category from 15 to 17 years, and 49.7 in the reproductive period over 18 years. Meanwhile, frequent complications of asymptomatic chlamydial infection include infertility! The danger for infected pregnant patients is the high probability of premature rupture of the membranes and the development of premature labor, the birth of a low-weight fetus, and the possibility of transmission of infection to the fetus (in 50% of cases during natural childbirth).
The causative agent of the infection is Chlamydia trachomatis (Figure 2).
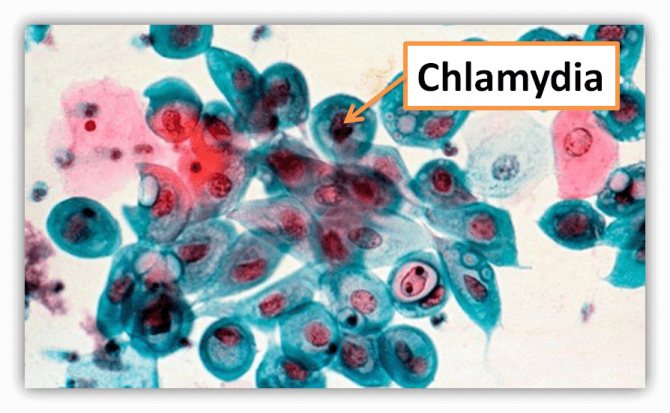
Figure 2 - Chlamydia trachomatis
The probability of transmitting a chlamydial infection with a single unprotected sexual contact with an infected person does not exceed 10%, while with regular sexual activity for two months it is already 55%. This is why it is necessary to treat both partners. The incubation period can last from 1 to 4 weeks.
In 70–95% of cases, the infection is asymptomatic. Symptoms of infection are nonspecific and may include general weakness, increased fatigue, pathological discharge from the genital tract, pain in the lower abdomen, cycle disorders, contact bleeding (occurring after sexual intercourse), pain during urination, and frequent urination. Reactive arthritis may develop. When examined in the mirrors, the gynecologist often sees signs of cervicitis (inflammation in the cervical canal) and swelling of the cervical mucosa.
Blood testing should not be used for diagnosis. The method of nucleic acid amplification (NASBA, nucleic acid sequence based amplification), PCR (polymerase chain reaction) and real-time PCR (RT-PCR) is used; the material is discharge (scrapings) from the urethra and cervical canal, as well as the first portion of freely released urine.
Diagnostics
There are quite a lot of pathogens that are included in the group of STIs. Modern medicine offers many diagnostic methods that can be used to detect them and prescribe an effective treatment regimen. Conventionally, they can be divided into several groups:
- microscopic methods;
- blood tests;
- cultural methods or cultures;
- DNA diagnostics.
After detecting symptoms that indicate the presence of a sexually transmitted infection, you should immediately consult a doctor. Women should make an appointment with a gynecologist, male patients with a urologist. If there are obvious signs of a sexually transmitted disease (chancres or other rashes on the genitals), you need to go to a venereologist.
Despite the extensive choice of diagnostic methods, an accurate laboratory method does not yet exist. If you suspect an STI, you cannot use just one method; most often they are used in combination for the most reliable result. Diagnosis often takes a lot of time on the part of the patient.
The first thing a person who is concerned about the symptoms of a sexually transmitted infection should do is take a smear for microflora. This is a standard procedure, which is also performed during a routine examination by a gynecologist or urologist. In men, a smear is taken from the urethra, in women - from the vagina and urethra.
The simplest methods also include bacterial culture. The doctor takes a certain amount of genital secretions for analysis. The taken material is placed in a nutrient medium, which promotes the rapid proliferation of bacteria: both “correct” and pathogenic.
In addition to microbiological analysis, if necessary, an enzyme-linked immunosorbent assay (ELISA) is prescribed. With its help, you can identify antibodies with which the body fights STIs. For some diseases that affect the entire body (syphilis, HIV), a blood test is performed (HIV determination and Wasserman reaction).
The most accurate diagnostic method is PCR (polymerase chain reaction). It allows you to identify hidden diseases characterized by an asymptomatic course. The infection is detected using DNA testing. This method is effective in cases of suspected HPV and other diseases that can remain dormant in the body for a long time.
In addition to examination by highly specialized specialists, patients with STIs may sometimes need the help of other doctors. Some diseases affect not only the genitourinary system, but also other organs. This applies to infections such as:
- HIV;
- syphilis;
- HPV, herpes, etc.
They can affect vision, joints, skin, circulatory system, and anus. Depending on the type of complications, it is necessary to contact an immunologist, proctologist, dermatologist, infectious disease specialist and other specialists.
It is important to remember that in the case of an STI, only a doctor can make a diagnosis. Many diseases have almost identical symptoms, so self-medication can only aggravate the situation and lead to dangerous complications.
Diseases caused by Mycoplasma genitalium (mycoplasma infection)
The detection rate of Mycoplasma genitalium (Figure 3) in the general population ranges from 1 to 5%, while in women at high risk of infection it is up to 42%. Infection occurs through contact of the mucous membranes of the genital organs, anogenital area and oral cavity. In 40 - 70% of cases, the disease is asymptomatic, in other cases the clinical picture is the same as for chlamydial infection.
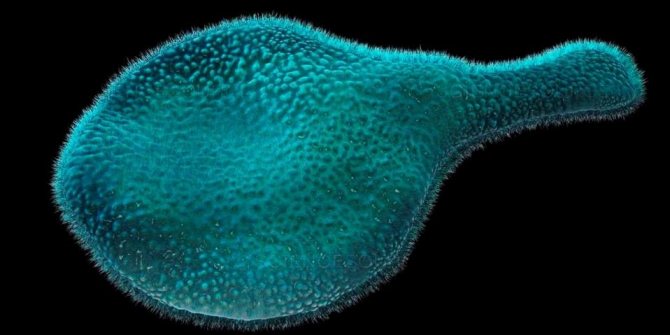
Figure 3 - Mycoplasma genitalium
Complications include pelvic inflammatory disease and ectopic pregnancy. Both chlamydia and mycoplasma damage the ciliated epithelium of the fallopian tubes, which is necessary for the advancement of the fertilized egg into the uterine cavity. Due to the fact that the fallopian tube simply has nothing to ensure the movement of the egg, pregnancy develops in the tube, resulting in a life-threatening condition.
If pregnancy occurs, infection with Mycoplasma genitalium increases the risk of miscarriage and premature birth. Diagnosis is the same as for chlamydial infection.
In this article I deliberately do not present currently recommended treatment regimens, since I consider it necessary to visit a doctor in person. An assessment of the effectiveness of the treatment (confirmation of the absence of a microorganism) for both infections should not be carried out earlier than 2 weeks when using NASBA, or a month after the end of the course of therapy - PCR, RT-PCR; if the result is negative, re-screening is not necessary!
Symptoms
There are seven main signs that indicate an STI. If they are detected, you must immediately consult a doctor: a gynecologist or urologist. The doctor will conduct an initial examination and prescribe further tests and examinations.
The presence of an STI may be indicated by:
- burning and itching in the intimate area;
- pain or discomfort during sex;
- altered genital discharge;
- pain in the lower abdomen;
- frequent and painful urination;
- rashes and redness in the intimate area;
- enlarged lymph nodes.
There are quite a few sexually transmitted infections, and each of them manifests itself differently. To describe them you will need a whole medical reference book. Here we will consider only the most common STIs, which can be contracted by every person on the planet, regardless of gender, age and social status.
Syphilis is an infectious disease that has been known to mankind since ancient times. The causative agent is a bacterium called spirochete pallidum. You can become infected with syphilis through any sexual contact. The first symptoms appear 10 days after infection - a hard chancre appears on the genitals or perineum (less often, other parts of the body). Over time, similar rashes appear in the mouth and on the fingers. There is a significant increase in lymph nodes, especially in the inguinal and cervical ones.
There are three stages of syphilis in total. In the absence of timely treatment, the disease can develop into a more severe form. As a result, ulcers spread throughout the body, including the mucous membranes. The patient is worried about inflammatory processes, headaches, aching bones, and deterioration in general health. At the third stage, meningitis may occur - inflammation of the membranes of the brain. Complications of syphilis can lead to paralysis and even death.
Chlamydia is one of the most insidious sexually transmitted diseases. Most people in the early stages of the disease have virtually no symptoms. In women they are less noticeable than in men, and may not appear at all. However, chlamydia is one of the main causes that leads to ectopic pregnancy, inflammatory processes in the pelvic organs and female infertility.
In male patients, chlamydia manifests itself with a number of characteristic symptoms. They are bothered by cutting pain during ejaculation and urination. This is caused by inflammation of the epididymis and urethra, which is caused by bacteria.
Gonorrhea is another fairly common STI, especially among people aged 15 to 24 years. Like chlamydia, it can be spread through oral, vaginal or anal contact. And just like with chlamydia, most infected women do not notice any symptoms in the first stages. However, in men, gonorrhea appears almost immediately. Patients are concerned about purulent discharge from the urethra, painful and frequent urination, and discomfort in the anal area.
In the absence of timely treatment for gonorrhea, complications arise. Women experience spotting after sex and cutting pain during it, body temperature rises and the general condition of the body worsens. Gonorrhea at any stage requires quick and effective treatment.
Trichomoniasis is a bacterial infection caused by Trichomonas vaginalis. At first, the disease does not show itself at all. The first symptoms appear approximately two weeks after infection. Men feel a burning sensation in the urethra, and discharge from the penis may appear.
In women, trichomoniasis manifests itself more clearly. Patients are concerned about painful sensations during sexual intercourse, which is caused by inflammation of the mucous membranes of the genital organs. One of the characteristic symptoms is thick yellow-green vaginal discharge with an unpleasant odor.
Genital herpes is a viral disease with extremely high susceptibility. It is transmitted not only through sexual intercourse, but also through skin-to-skin contact. The causative agent is herpes simplex virus type 2 (HSV-2). A day after infection, small blisters appear on the external genitalia. They are accompanied by itching and slight tingling. Over the next few days, the blisters turn into painful sores, fever and enlarged lymph nodes are observed.
Rashes are only the visible part of the disease. Even after they disappear, the herpes virus remains in the body for life. Lack of treatment in pregnant women can lead to serious complications, including fetal death.
Human papillomavirus (HPV) is a sexually transmitted virus. HPV types 16 and 18 are one of the main causes of cervical cancer in women. Regardless of gender, the disease manifests itself in the same way - in the form of small warts in the perineum and anus. In men, they can be hidden behind the foreskin and in the urethra. An asymptomatic course of the disease is also possible. In this case, the presence of infection can only be determined using special tests.
Ureaplasmosis is a disease that tends to be chronic. The causative agent is a single-celled microorganism called ureaplasma. Modern medicine classifies it as a conditionally pathogenic flora. This means that a small amount of ureaplasma is present in a healthy person. The disease begins when microbes become active and multiply rapidly, thereby displacing healthy microflora.
The first symptoms appear after 14-20 days. Patients experience inflammation of the genitourinary system, burning sensation when urinating, cloudy vaginal discharge. Women may be bothered by pain in the lower abdomen and cervicitis. Over time, the disease becomes chronic, which entails many complications:
- colpitis;
- endometritis;
- stricture (narrowing) of the urethra;
- inflammation of the fallopian tubes;
- cystitis, etc.
Untimely treatment of the infection often leads to infertility, missed abortion and premature birth.
Mycoplasmosis - like ureaplasmosis, is caused by opportunistic microorganisms that can be in a “dormant” state in the body of a healthy person. However, sometimes mycoplasmas provoke a number of diseases of the genitourinary system. In women, they manifest themselves as nagging pain in the lower abdomen, burning during urination and pain during sexual intercourse.
HIV or human immunodeficiency virus is the most dangerous sexually transmitted disease. HIV does not make itself felt immediately - the incubation period of the disease lasts from 21 to 90 days. Symptoms appear only at the stage of manifestation of the infectious process.
Patients complain of inflammation of the lymph nodes, chronic weakness, headaches and loss of appetite. A characteristic symptom of HIV is inflammation of the tonsils (tonsillitis), which does not go away for a long time. In patients, the body temperature rises to 37-37.5 degrees, but it is not possible to normalize it with the help of antipyretic drugs.
The lack of antiretroviral therapy has an extremely negative impact on the patient’s condition. The body is attacked by all kinds of viral and bacterial diseases: pneumonia, herpes, tuberculosis, candidiasis. As a result, AIDS develops.
Diseases caused by Mycoplasma hominis and Ureaplasma species
As for such frequently detected microorganisms as Mycoplasma hominis and Ureaplasma species (Figure 4), they are classified as opportunistic, that is, their presence in small quantities in a healthy person is acceptable. In the absence of clinical manifestations, patients suffering from infertility, women with a history of pregnancy losses, as well as sperm donors are subject to treatment. But signs of cystitis, urethritis and cervicitis, as well as ascending infection, are an indication for therapy. In this case, effective treatment is considered to be the absence of clinical and laboratory signs of the inflammatory process, and not the absence of microorganisms.
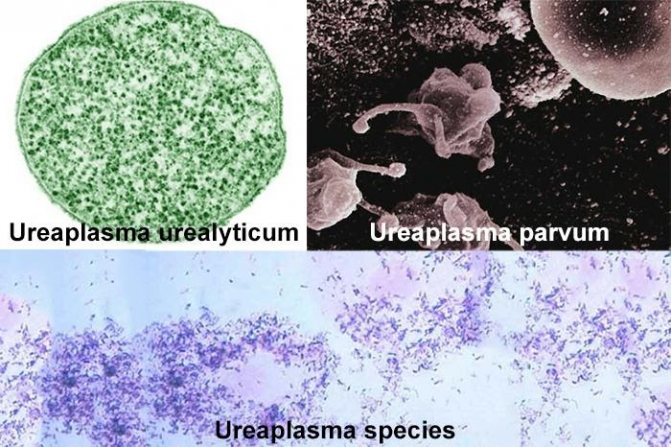
Figure 4 - Ureaplasma species
Detection methods are the same as for chlamydial and mycoplasma infections; vaginal discharge can also serve as material for research.
Methods of transmission of STIs
STIs are spread through sexual contact—vaginal, oral, or anal. The gender of a person does not matter - they can go from a man to a woman, from a woman to a man, from a man to another man, or from a woman to another woman.
Many sexually transmitted infections can be spread through any contact between the genitals, mouth and anus, even if there is no penetration. For example, genital herpes is transmitted through direct skin-to-skin contact - microdamages on its surface are enough for infection.
Some STIs are transmitted in other ways. For example, HIV and hepatitis B are transmitted through sharing of injection needles and blood transfusions.
The use of barrier methods of contraception does not always guarantee safety. When using condoms for safe sex, it is important to follow the instructions on the package. Proper use of condoms makes them more effective. The following precautions must be observed:
- check the expiration date and integrity of the packaging;
- wear a condom before sex, not during it;
- use lubricant during sexual intercourse with a condom;
- remove and dispose of condoms correctly;
- never remove a condom and try to put it on again;
- never reuse a condom.
Preparation for PCR for 12 STIs
Before being tested for STI 12 infections, the patient must:
- refrain from urinating for 3 hours (for men) or 1.5 hours (for women);
- do not take antibacterial drugs for 2 weeks;
- abstain from sex for 36 hours before the study;
- on the day of testing, do not use disinfectants and antibacterial agents;
- refrain from drinking alcohol 3 days before the test.
Women should also take into account that the procedures are not possible during menstruation, and on the day of the test they cannot insert suppositories or tampons, undergo colposcopy, douching, biopsy, or ultrasound with a vaginal probe.
Types of PCR
To date, more than a dozen different types of polymerase chain reactions have appeared in medicine: recombinase, nested, inverted, asymmetric, stepwise, group-specific, reverse transcription, “hot start” and so on - all of them are designed taking into account specific diagnostic requirements . It would be difficult and boring for a person ignorant of molecular biology to understand the intricacies of this typology. The truly interesting types of PCR are those that are widely used in practice and are actively offered to patients. Let's talk about these analyzes in more detail.
PCR 12
The record holder for popularity is deservedly held by the so-called comprehensive PCR 12 analysis - it is so called because it includes the 12 most common sexually transmitted infections, as well as a control test for the quality of the materials taken (QVM).
Why is this type of diagnosis so relevant?
Firstly, because it corresponds to the sad realities of the present time, when one patient with a dermatovenerologic profile is diagnosed with a whole “bouquet” of bad sores. Secondly, because it is easier for laboratories to use a ready-made cartridge, which contains all the necessary primers at once. Thirdly, this is more beneficial for the patient himself, since a comprehensive analysis will be cheaper than testing for each STI separately.
How is PCR 12 tested?
In men, a swab is taken from the urethra. This is not a very pleasant, but quite tolerable and quick manipulation. In women, an epithelial scraping is taken from the vagina or cervix. This procedure usually does not cause pain. Read below about the rules for preparing for a visit to the laboratory.
The standard PCR kit 12 looks like this:
- Herpes viruses type 1 and 2;
- Papillomoviruses types 16 and 18 (oncogenic);
- There are two types of mycoplasmas - human and genital;
- Cytomegalovirus;
- Ureaplasma;
- Chlamydia;
- Trichomonas;
- Gonococcus;
- Candida.
Thirteenth on this list is KVM - control of smear taking, which is carried out by searching for the HMBS gene. It is possessed by the epithelial cells lining the urethra. When a smear is taken from a different location, a different gene is looked for. If 250 or more copies of the desired gene are detected in the sample, then the PCR 12 analysis was taken correctly, and its results can be trusted. If there are fewer copies of a specific gene than normal, it is better to undergo re-diagnosis to avoid a false negative result. As for positive answers, they are accepted as true in any case.
The list of pathogens examined as part of the PCR 12 analysis may differ in different laboratories. For example, additional types of herpes virus or papillomavirus may be included, then the analysis will be called “PCR 13” or “PCR 14”. Sometimes the list, on the contrary, is shortened to “PCR 4” (gonorrhea-trichomoniasis-chlamydia-mycoplasmosis).
Qualitative PCR and quantitative PCR
These two types of PCR diagnostics have fundamentally different goals: a qualitative analysis gives an answer to the question of whether the patient has the desired microbe at all, that is, simply “yes” or “no.” The PCR 12 complex just discussed falls into this category.
But there is also quantitative analysis, or real-time PCR. The method is based on the fact that the number of new amplicons (copies of a given DNA section of the pathogen) is directly proportional to their original number. That is, if there were a lot of harmful DNA molecules in the sample from the very beginning, then with each cycle of the polymerase chain reaction there will be twice as many of them, and by the end of the process millions will have accumulated. Modern amplifier devices monitor how the copy number changes, and based on the results of the study, they calculate the approximate concentration of the pathogen in the patient’s body.
What is it for? In the case of bacteria, protozoa or fungi, such information is of questionable diagnostic value, since the number of colonies is constantly changing under the influence of a variety of factors, and it is relatively easy to destroy such microorganisms. Another thing is the virus. It is a noncellular life form that cannot be exterminated in the same way that antibiotics kill bacteria. In the fight against viruses, a person can firmly rely only on his immunity, and the capabilities of antiviral agents are very limited. It is when it comes to viruses that the real-time PCR technique becomes especially relevant.
Viral load or viremia is the severity of the virus affecting the body. The indicator is calculated by determining the number of virions in biological material, measured in IU or the number of copies per 1 ml of blood and serves to monitor the progress of therapy and prevent the spread of the virus.
Quantitative PCR is critically necessary for carriers of the following infections:
- Human immunodeficiency virus (HIV);
- Hepatitis B and C.
But in the case of other viruses, determining the load can be useful - for example, when it comes to cytomegalovirus, herpes or papillomavirus. The analysis will help to understand whether a person is at risk of another exacerbation of the disease, and how high the likelihood of transmitting the infection is.
HIV-infected people are prescribed antiretroviral therapy. Its goal is to reduce the viral load as much as possible, and ideally to make it undetectable. But even in this case, there is a risk of infecting your sexual partner, so you should not neglect the use of condoms.
[Video] Viral load and its tracking for HIV-infected people:
Where and how is material taken for PCR research 12
PCR testing can be carried out for almost any biomaterial.

To obtain a sample, scrapings are taken from the urethra, vagina, and uterine cervix.
In this case, the correct technique for taking biomaterial is very important.
Since PCR is a very accurate method, the entry of foreign impurities into the test sample can distort the final data (false positive result).
Likewise, if the sampling technique is incorrect and the material is not taken from a suitable area, the pathogen will not get into the sample and the result will be false negative.
For example, in women, the causative agents of gonococcal infection are usually located in the cervical canal, but may not be present in the vagina.
In men, infectious agents can exist in the prostate gland and epididymis with complete absence in the urethra.
It is worth noting that the previously used provocation techniques (the supposed increase in the number of pathogens under the influence of various factors) are now not used due to ineffectiveness.
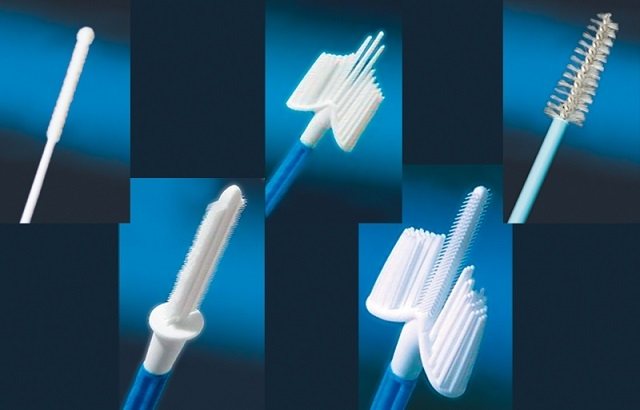
To collect material from the organs of the urogenital tract, vaginal tampons and special probes are used.
Preparation for PCR testing for 12 infections depends on the material being studied.
PCR - what is it?
Any living creature on Earth, be it a person, an animal or a microbe, has genes - carriers of hereditary information, which are sections of DNA or RNA with a specific nucleotide sequence, unique for each organism. DNA (deoxyribonucleic acid) and RNA (ribonucleic acid) form long molecules consisting of two strands twisted into a spiral relative to each other, and these strands are assembled from nucleotides like beads.
Let’s say you want to see whether the patient’s biological material contains DNA or RNA of an infectious pathogen or its fragments. But how to do this if the molecules are tiny and there are few of them? The PCR technique provides the answer: it is possible to artificially propagate harmful DNA or RNA in the laboratory in order to easily detect and identify it.
The essence of the polymerase chain reaction is to separate the strands of molecules and try to “plant” DNA or RNA fragments of pathogens at their opposite ends - if they fit, then this is the desired microbe. And an enzyme called “DNA polymerase” added to the test tube will trigger the synthesis of new copies of the desired sections of the molecules, they will multiply many times and become noticeable. Next, we will describe in simple words how this amazing process occurs and why it is necessary.
American scientist Carrie Mullis invented PCR in 1983, and ten years later, in 1993, he received the Nobel Prize in Chemistry for his discovery. However, the technique was imperfect and required significant improvements. Today, there are already more than a dozen types of PCR for various diagnostic purposes.
In the case of real-time PCR diagnostics (Real-Time PCR), the influence of the human factor on the results of the study is minimal - the tubes are placed in a modern high-tech device and are never opened throughout all cycles, including analysis of the results, which is also carried out by a smart machine. This method has only two obvious drawbacks: high cost and limited availability, since not every laboratory is equipped with new-generation amplifiers.
[Video] Visual information - what is PCR and how does the process work?
What is submitted for PCR analysis?
When choosing the type of biomaterial for diagnosis, doctors are guided by the specifics of the infection and its favorite localization. After all, whether harmful DNA gets into the sample determines whether a reliable analysis result will be obtained.
The following materials are taken for PCR:
- Smear
or epithelial scraping from mucous membranes. This can be the urethra, vagina, cervix, cervical canal, anus, oral, nasal and even eye cavity. Smears are most relevant in diagnosing sexually transmitted diseases. To take a smear or scrape, probes with different tips are used;
- Blood
taken from a vein when it is necessary to detect HIV, hepatitis, cytomegalovirus, mononucleosis or any disease of bacterial etiology, for example, syphilis, cholera or borreliosis;
- Biological fluids
(urine, saliva, semen, sputum, prostate secretions, gastric juice, pleural, joint, cerebrospinal or amniotic fluid, as well as bronchoalveolar lavage) are taken according to indications. For example, PCR analysis of sputum is used in the diagnosis of tuberculosis;
- Points and biopsies
organs and tissues are usually taken when cancer is suspected. The exception is a gastric biopsy, which is performed to determine the presence of Helicobacter pylori, a bacterium that causes gastritis and peptic ulcers.
Storage and transportation of biomaterials
Samples must be sent to the thermal cycler no later than 2 hours after collection if they are kept indoors at room temperature. When PCR analysis needs to be postponed for some reason, the tubes with biomaterials can be left in the refrigerator for one day at a temperature of 2 – 8°C. The maximum shelf life is 14 days, but then the samples are deep frozen (-20°C). Once thawed, they must be used immediately; re-freezing is prohibited.
In the vast majority of cases, PCR diagnostics are carried out “day to day”: the patient comes to the clinic, where a smear or blood is taken from him and the biomaterial is immediately sent to the laboratory, so there is no need to worry about storage rules.
Results of PCR analysis
Above we mentioned qualitative and quantitative PCR diagnostics, and so, in the first case, deciphering the results does not present any difficulty: the answer is either positive or negative. And if the conditions of preparation, collection of biomaterial, analysis and evaluation of the results were not violated, then there is no reason to doubt the reliability of the data obtained.
The situation is different in the case of quantitative PCR. The result is a number indicating the viral load. Viremia is measured in IU/ml or in copies/ml, with one IU (international unit) containing approximately 4 copies of the virus (the exact figure must be found in the laboratory that performed the analysis, since everyone’s equipment is different).
For example, for hepatitis C, a viral load of up to 600,000 IU/ml is considered low, 800,000 IU/ml is considered medium, and 1,000,000 IU/ml is considered high.
In some clinics, to make the results of quantitative PCR analysis more compact, the following entries are used: 3*103 IU/ml, 4*104 IU/ml, 5*105 IU/ml, and so on. To understand what number we are talking about, it is enough to multiply.