2 Edition
With the onset of the coronavirus COVID-19 pneumonia pan-epidemic, the demand for the article has increased.
FOR DIAGNOSIS OF VIRAL PNEUMONIA, ULTRASOUND IS MORE SUITABLE THAN X-RAY.
In acute respiratory failure, the ultrasound method is equal to CT in terms of diagnostic accuracy.
For pinpoint diagnosis, it is useful to target using auscultation and percussion of the lungs.
Structure of the lungs and pleura
The pleura is a serous membrane made up of a layer of flat mesothelial cells on a basement membrane.
The outer layer - the parietal pleura - lines the internal space of the chest.
The inner layer - the visceral pleura - fuses with the lung everywhere, excluding the hilum area.
The gap between the parietal and visceral sheets of the pleura is called the pleural cavity.
A small volume of serous fluid increases the sliding of the pleural layers during inhalation and exhalation.
The lungs fill most of the chest cavity; There is a cardiac notch in the left lung.
The costal surface of the lung is convex, the diaphragmatic and mediastinal regions are concave.
The root of the lung is located in the posterior mediastinum at the level of attachment to the sternum of the III-V ribs.
The root consists of the main bronchus, arteries, veins, nerves, lymphatic vessels and lymph nodes.
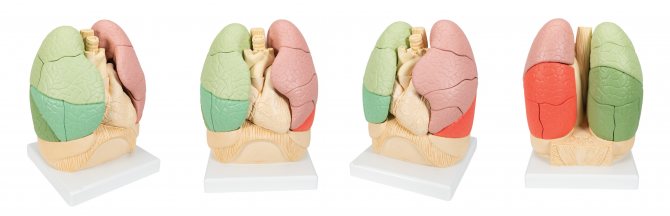
A lobe is an anatomically autonomous unit of the lung with a lobar bronchus, vessels and nerves.
In the right lung, oblique and horizontal grooves separate the upper, middle, and lower lobes.
The left lung is cut by the main interlobar groove; here the upper and lower lobes are distinguished.
The lung consists of 10 bronchopulmonary segments with a segmental bronchus, vessels, and nerves.
Intersegmental veins are stretched along the connective tissue intersegmental septa.
According to the course of branching of the bronchi and blood vessels, the lung segments diverge into subsegments and lobules.
The intralobular bronchus enters through the apex of the lobule; this one distributes terminal bronchioles.
The pulmonary lobule consists of acini (primary pulmonary lobules); gas exchange takes place here.
Ultrasound of the chest - what kind of procedure is it?

Lung ultrasound is not prescribed to all patients; many have not even heard of this type of examination. However, the technique exists and is used for the early detection of various diseases of the lungs, bronchi, pleura, lymph nodes and surrounding tissues. Ultrasound of both lungs is often combined with ultrasound of the pleural cavity. This is due to the need to examine the chest organs in more detail to identify a number of combined pathologies.
The advantages of ultrasound are:
- There is no pain or discomfort.
- There is no need for preparation, refusal to drink or eat.
- There is no effect on medication use.
- In children, the procedure can be performed even in their sleep.
- The duration of the examination is minimal, the price is affordable.
- There are no strict contraindications.
Ultrasound of the lungs and pleura
Ultrasound of the lungs and pleura is performed using abdominal scanning settings in the main B-mode.
Sector and microconvex sensors are convenient, but you can work with convex and linear sensors.
For superficial structures - 7-10 MHz, and for general inspection and distant foci - 2.5-5 MHz.
Acoustic shadows behind the ribs, sternum, and spine will significantly interfere with imaging.
Ultrasound is possible through the intercostal spaces, the upper and lower apertures of the chest.
Mark the anterior, lateral, and posterior areas; zones are additionally divided into v/3, s/3, n/3:
- anterior zone - from the sternum to the anterior axillary line;
- lateral zone - from the anterior to posterior axillary line;
- posterior zone - from the posterior axillary to the paravertebral line.
The posterior zone in v/3 corresponds to the upper lobe; c/3 and n/3 correspond to the 6th and 10th segments of the lower lobe of the lung.
The anterior zones are studied with the patient in the supine position, the posterior zones - on the side, stomach, sitting.
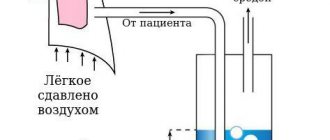
When the patient lies on his back, air accumulates in front, and fluid flows back.
Pneumothorax and pulmonary edema are visible from the front, pneumonia and pleurisy are seen from the back and sides.
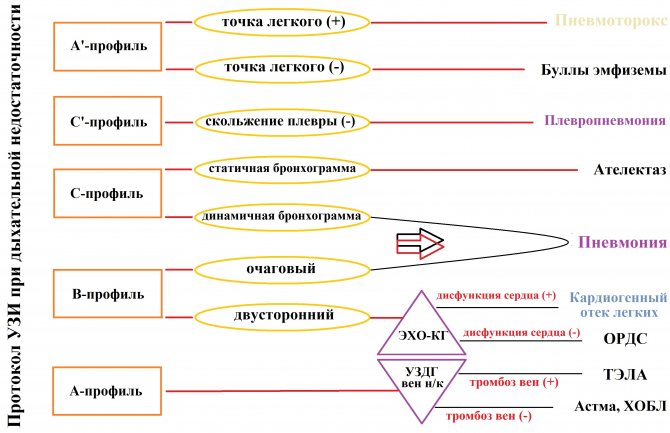
Every disease with acute respiratory failure has its own special echo picture.
Echo image of a normal lung
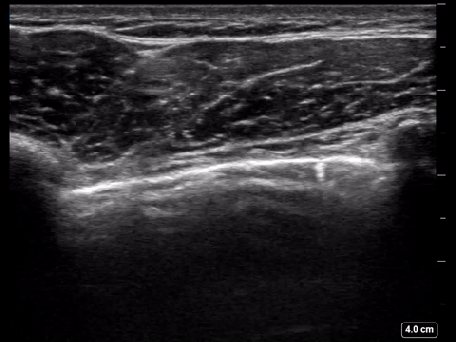
A standard cross section shows the shadows of 2 adjacent ribs and the intercostal space.
Below the ribs there is a hyperechoic line of the pleura, and the visceral sheet slides synchronously with breathing.
In the chest cavity there is an obstacle that is insurmountable for the ultrasound beam - the airy lung tissue itself.
Ultrasound does not show normal lung tissue, only an echogenic pleural line with artifacts.
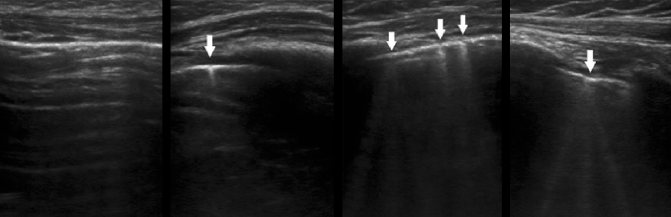
A-lines - horizontal lines occur exactly at a distance equal from the skin to the pleura.
In a normal lung, A-lines are slightly noticeable and bright, single and multiple.
B-lines are vertical lines of the “comet tail” type that run synchronously with the visceral pleura.
B-lines are burned from the echogenic line of the pleura to the end of the depth, crossing across the A-line.
Z-lines are short vertical lines of the “comet tail” type that do not reach the first A-line.
When touching the sheets of pleura, sliding of the visceral pleura, B- and Z-lines becomes visible.
In healthy lungs, in one intercostal space there are several short Z-lines, up to 3 long B-lines.
Rules for preparing for ultrasound in pulmonology
There are no mandatory preparation requirements for sonography, regardless of whether ultrasound of the pleura, lungs, mediastinum or bronchi is performed. Before the procedure, you can eat, drink non-alcoholic drinks, and take medications.
Respiratory sonography has two limitations. An ultrasound examination is performed on an empty stomach if general anesthesia is used or performed with an endoscopic scanner. For burns, injuries or diseases with deep damage to the epidermis, the procedure is carried out after granulation (healing) of the wounds.
Ultrasound protocol for respiratory failure
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A | A | A |
| Lateral | A | A | A | A | A | A |
| Rear | A | A | A | A | A | A |
| Conclusion: Echo picture of a normal lung (USDG of non-crystal veins is shown). | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A | A | A |
| Lateral | A | A | A | A | A | A |
| Rear | A | WITH | WITH | A | A | A |
| Conclusion: Echo picture of alveolar consolidation (pneumonia) in c/3 and n/3 of the posterior zone of the right lung (segments 6 and 10 of the lower lobe). | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A | A' | A |
| Lateral | A | A | A | A | A | A |
| Rear | A | A | A | A | A | A |
| Conclusion: Echo picture of partial pneumothorax of the left lung, the point of the lung at the level of the anterior axillary line. | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A' | ||
| Lateral | A | A | A | |||
| Rear | A | A | A | |||
| Conclusion: Echo picture of complete pneumothorax of the left lung, the point of the lung is not determined. | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | IN | IN | ||||
| Lateral | ||||||
| Rear | ||||||
| Conclusion: Echo picture of bilateral interstitial pulmonary edema (ECHO-CG shown). | ||||||
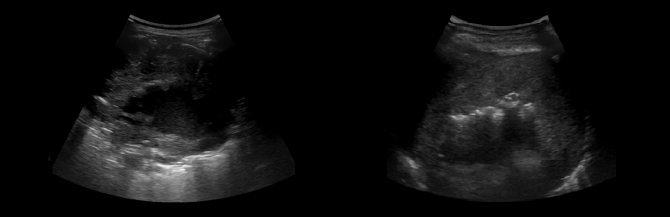
Echo pattern of alveolar consolidation
With pneumonia, there is local swelling of the lung, as well as pleural effusion of varying significance.
Due to inflammation and edema, the lung parenchyma becomes echo-dense like the liver - “hepatization”.
Against the background of pneumonia, the sliding of the pleura is usually weak due to a small excursion of the lung and adhesions.
With pleuropneumonia, sliding (-), acoustic enhancement in the form of a bright vertical C-line.
The border between the consolidation and the air tissue is often ragged and echogenic, with an energetic B(+) line behind it.
Within the foci of alveolar consolidation, hyperechoic contours of the bronchi can be observed.
Dynamic bronchogram - movement during inhalation and exhalation - air in the bronchioles during pneumonia.
Static bronchogram - immobility during inhalation and exhalation - atelectasis with bronchial obstruction.
Liquid bronchogram - anechoic tubular structures - fluid inside and along the bronchioles.
Echo pattern of pleural effusion
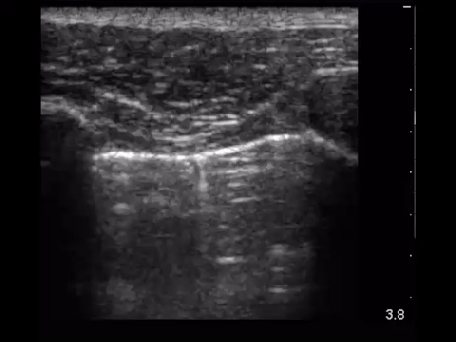
Usually the effusion is found above the diaphragm, but it can be confined anywhere in the chest cavity.
Pleural effusion is hypo- or anechoic; may include suspension, threads, clots and partitions.
Hemothorax and empyema are isoechoic in the liver and spleen, homogeneous or heterogeneous.
Calculation of pleural fluid volume: V (ml) = maximum separation (mm) of pleural sheets * 20.
B-mode - the hypo- or anechoic area between the sheets of pleura disrupts the shape of inhalation and exhalation.
The echo-dense lung responds to the pressure of the pleural fluid like a sail under a gentle wind.
M-mode - a sinusoid in solidarity with breathing, the sheets of the pleura come closer and diverge during inhalation and exhalation.
Echo picture of pulmonary edema
Pulmonary edema can be focal or diffuse; On ultrasound, many B-lines move along with breathing.
With pulmonary edema in the intercostal space there are more than 3 B-lines; the short pitch between them is less than 3 mm.
To distinguish between cardiogenic and noncardiogenic causes of edema, evaluate left heart function.
Cardiogenic causes of pulmonary edema: impaired LV contraction, abnormal MtCl and AoCl.
The B profile occurs with excessive infusion therapy due to volume overload.
Other causes of pulmonary edema: ARDS, aspiration, pneumonia, allergies, toxins, kidney disease...

Echo pattern of pneumothorax
When the pleural sheets are separated by a layer of air even 1 mm thick, there will be echo signs of pneumothorax.
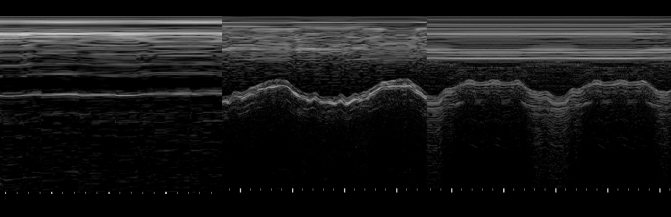
A'-profile - A-lines, sliding (-); in M-mode, when sliding (-), a “bar code” will be set.
In the presence of sliding of the pleural layers in the M-mode, the “sea shore” picture is determined.
Weakly moving lines of the chest wall (“waves”) lie above a fine-grained layer (“beach”).
The deep granular layer appears from satisfactory respiratory movements of the lung.
In the intercostal space, the sensor is moved back from the sternum to the border of the pneumothorax - the “lung point”.
At the border of pneumothorax, the sheets of pleura stick together during inhalation and are separated by air during exhalation.
Here, at the “lung point,” sliding/non-sliding and “seashore”/“barcode” are interspersed.
“Lung point” occurs with partial pneumothorax; it is absent with complete collapse of the lung.
With a small anterior pneumothorax, the “lung point” is anterior to the anterior axillary line.
With average anterolateral pneumothorax, the “lung point” is above the mid-axillary line.
With massive pneumothorax, the “lung point” is determined posterior to the mid-axillary line.
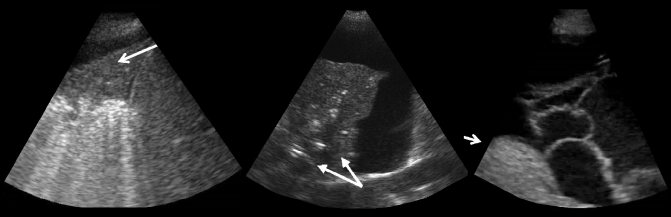
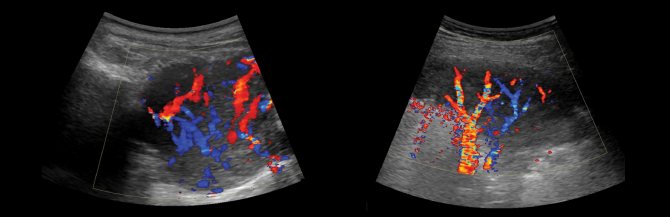
Echo picture of pulmonary embolism
In a patient with sudden shortness of breath and a normal echo picture of the lungs, it is necessary to exclude PE.
A targeted ultrasound of the deep veins of the non-cancerous veins is indicated: only the femoral and popliteal veins are examined.
The sensor is determined longitudinally immediately under the c/3 inguinal ligament, then to the center of the popliteal fossa.
The vein stuck together due to the pressure of the sensor - there is no thrombus; the vein does not compress completely - there is a thrombus in the lumen.
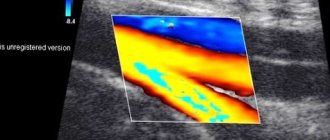
The thrombus can be “blind” isoechoic; pay attention to the defective color flow signal and spectrum.
Massive pulmonary embolism causes acute cor pulmonale—a “loose” right heart.
A patient with pulmonary embolism sometimes has triangular-shaped foci on the subpleural base.
Rarely does the lesion have a round and polygonal shape; Small pleural effusion often collects.
Echo picture during exacerbation of COPD or asthma
Echo picture of a normal lung, venous thrombosis n/c (-), effusion (-), exacerbation of COPD is likely here.
With anterior emphysematous bullae and at the peak of an asthma attack, the pleural slip is tiny.
The echo pattern is similar to pneumothorax, but the absence of a “lung point” indicates COPD or Asthma.
Echo pattern during intubation
Endotracheal intubation - sliding (+) on 2 sides;
Esophageal intubation - sliding (-) on 2 sides;
Endobronchial intubation - sliding (-) on the 1st side.
Lung cancer on ultrasound
Air tissue reflects 99% of ultrasound waves, only tumors are visible immediately under the visceral pleura.
Central lung cancer is often associated with atelectasis or recurrent pneumonitis.
When there is atelectasis, consolidation, pleural effusion, the ultrasound beam penetrates into deeper zones.
In patients with lung cancer, the presence of pleural effusion suggests stage T4 disease.
In rare cases, the causes of effusion are different - impaired lymphatic drainage, atelectasis, hypoproteinemia.
Aspiration of fluid, cytological and biochemical analysis will help make an accurate diagnosis.
Rupture of the pleural line and lack of sliding may indicate invasion of the chest wall.
The bulk of the tumor receives nutrition through neoangiogenesis from the bronchial artery.
Neoangiogenesis involves an ugly vascular architecture - chaotically disordered, tortuous.
The spectrum is monophasic with small fluctuations in systole/diastole, variable flow direction.
Large cancerous tumors, larger than 5 cm, often have an area of necrosis in the central zone.
When the area of necrosis is associated with the bronchial tree, hyperechoic gas bubbles appear.
Which is better - X-ray or ultrasound of the chest?

To differentiate oncological pathologies from benign tumors or to clarify a questionable diagnosis, information from ultrasound will not be enough. Ultrasound diagnostics is based on obtaining data from the contact of a sound wave with dense organ tissue. The lungs are filled with air, so their visualization will not be highly accurate. In this regard, such examination is rarely performed in adults, only if there are direct contraindications to radiography.
But in childhood, during pregnancy, ultrasound of the pleural cavity and lungs will be a safe alternative to the use of x-rays.
Despite the fact that with an ultrasound examination of the lungs the information will not be as accurate as with radiography, the technique still has an advantage. Thus, ultrasound has the ability to search for pleural effusion (fluid accumulation) even with its minimum volume (from 5 ml), as well as to identify the type of exudate.
Ultrasound is indispensable if it is necessary to perform a pleural puncture - it is under ultrasound control that this invasive manipulation is performed.
Experience the son of difficult mistakes
Task. Child with high fever and cough. Ultrasound shows pleural effusion in the posterolateral regions with many avascular septa; C-profile of the lower lobe - alveolar consolidation with a dynamic bronchogram, B (+) line at the border with the air tissue. Conclusion: Echo picture of alveolar consolidation (pneumonia) in the lower lobe of the lung, pleural empyema.

Task. A patient after a kidney transplant complains of shortness of breath and a wet cough. On the left in the lower parts of the lung there is no breathing; there is a dull sound to percussion. Ultrasound shows anechoic fluid above the spleen; in the lower lobe of the left lung there is a C-profile with a static bronchogram. Conclusion: Echo picture of atelectasis of the lower lobe of the left lung, pleural effusion. Therapeutic and diagnostic puncture: sterile transudate.

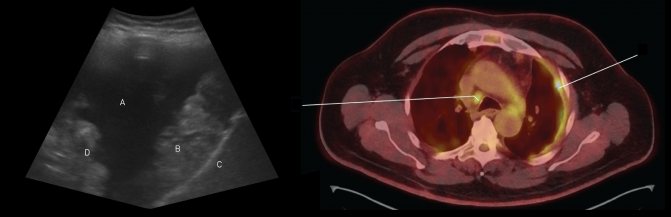
Task. Task. Ultrasound shows a flat diaphragm (C), an anechoic pleural effusion (A), and a thick diaphragmatic (B) and visceral (D) pleura with an uneven lobular contour. Conclusion: The echo pattern may be consistent with pleural mesothelioma. Positron emission tomography shows a focus of mesothelioma in the third intercostal space on the left, metastases in the paratracheal lymph node on the right.
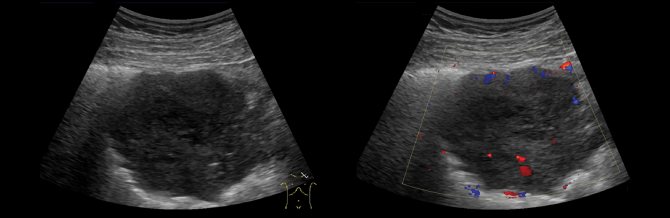
Task. Ultrasound shows abundant pleural effusion; a hypoechoic node with active vascularization grows from the diaphragmatic surface of the parietal pleura. Conclusion based on biopsy data: Metastases of cholangiocarcinoma.
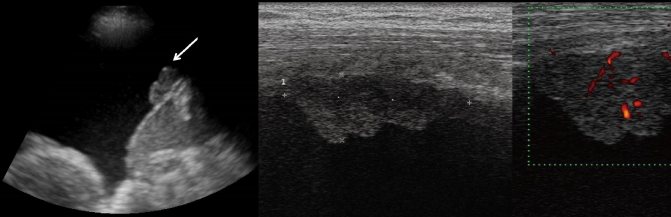
Task. Ultrasound shows a defective pleural line, subpleural formation of reduced echogenicity with an uneven lobular contour, heterogeneous echostructure; abnormal chaotic (non-radial) intranodular vessels.
Task. Ultrasound shows a defective pleural line, subpleural formation of reduced echogenicity, uneven contour, heterogeneous echostructure; invasive growth into the soft tissue of the chest wall (1), three ribs are also affected (2).
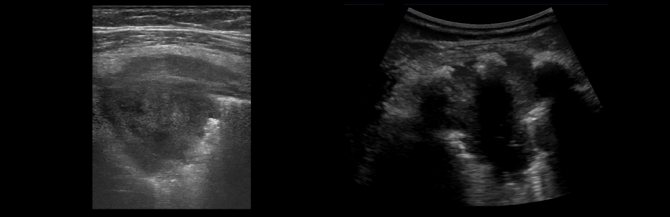
Task. On ultrasound, squamous cell lung cancer: a rounded formation, in the center there is a zone of reduced echogenicity - necrosis (1); in the necrotic core you can see hyperechoic inclusions with a “comet tail” - gas bubbles (2).
Task. Ultrasound shows lung cancer: a focus of low echogenicity, disordered vessels with variable flow direction (1). On ultrasound, adenocarcinoma is creeping: the pseudonormal vascular architecture mimics a benign tumor (2).
Take care of yourself, Your Diagnosticer!
Tags: COVID-19 easy lectures pleura ultrasound