Chronic apical periodontitis
Chronic apical periodontitis is most often an asymptomatic inflammation in the tissues of the apical periodontium, which is manifested by radiological changes at the apex of the tooth roots.
Many dentists use the clinically convenient classification of I. G. Lukomsky. It simplifies the diagnosis.
Chronic fibrous periodontitis
Occurs as an outcome of acute periodontitis or treatment of granulating and granulomatous periodontitis. Traumatic etiology is also important due to overload, which occurs with the loss of a large number of teeth or non-physiological articulation.
Chronic fibrous periodontitis is detected on an x-ray as an expansion of the periodontal fissure in the apex area and is almost never accompanied by destruction of the adjacent bone.
Chronic granulating periodontitis
It is the most active form among all chronic periodontitis and is the outcome of an acute process.
The patient complains of unpleasant, slightly painful sensations when biting on the causative tooth.
Externally, the patient looks as usual, sometimes there is an increase in the submandibular lymph nodes. In the oral cavity we see hyperemic mucosa in the tooth area, painful on palpation. A distinctive feature of this type of periodontitis is the presence of a fistula in the projection of the root apex. It may ooze pus or bulge granulations. Young granulation tissue grows through damaged cement or even dentin into the bone marrow spaces, often growing along the walls of the fistula tract. The tooth is destroyed or intact. Percussion is weakly positive.
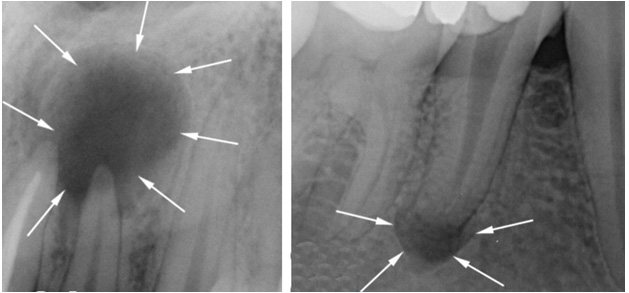
On the x-ray we see a clearing area due to bone destruction in the area of the root apex. The lesion has unclear contours and comes in different sizes.
Chronic granulomatous periodontitis
This type of periodontitis is asymptomatic and manifests itself clinically only during exacerbations. These manifestations can be of the type of granulating periodontitis in the form of fistulas and hyperemia of the mucous membrane.
The difference between granulomatous periodontitis and granulating periodontitis is the presence on the radiograph of a clearing focus at the apexes of the roots with a clear round shape (apical granuloma).
Currently, doctors are moving away from grading the size of the lesion (0.5 cm - granuloma, 0.6-0.8 cm - cystogranuloma, more than 0.8 cm - radicular cyst.
Prevention
Simple preventive measures will help to avoid the occurrence of fibrous periodontitis:
- regular oral hygiene - brushing your teeth after breakfast and before bed, using dental floss and rinses;
- timely replacement of the toothbrush;
- individual selection of pasta;
- exclusion of periodontal trauma (replacement of fillings, correction of orthopedic structures);
- systematic removal of tartar and plaque in the dentist’s office;
- preventive examinations for the purpose of early diagnosis of diseases.
If you follow these recommendations, there is a good chance that you will not need treatment for fibrous periodontitis.
Cyst - what is it and why?
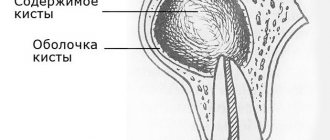
A cyst is a cavity that has an epithelial lining and cystic contents. There are two types of cysts - true and pocket.
The true one is completely covered by the epithelial lining, and the pocket one communicates with the root canal, it seems to grow from it.
Cyst formation occurs in 3 stages.
At the first stage, the epithelial cells of the islets of Malasse most likely proliferate under the influence of growth factors.
During the second stage, an epithelial cavity is formed.
These epithelial cells are directed away from their source of nutrition, die, and neutrophils drag their remains into the area of necrosis. Microcavities are formed, which then merge into one and become limited by stratified squamous epithelium.
There is another theory - the theory that the epithelium covers all open connective tissue areas, resulting in necrosis.
At the third stage of cyst formation after the death of neutrophils, there are reserves of prostaglandins, as well as cytokines produced by macrophages and T lymphocytes. Together they activate osteoclasts and trigger bone resorption.
Pocket cysts have a different mechanism of development. There is a large accumulation of neutrophils near the apical foramen in response to root canal infection. The cells die, as before, and this microabscess is closed by proliferating epithelium. A so-called epithelial ring is formed. Neutrophils that remain outside the channel die and form a microcavity. The presence of infection outside the canal further attracts neutrophils, expanding the microcavity to larger sizes. A pocket cyst is called such because the enlargement of the root canal resembles an enlargement of the periodontal pocket.

Traumatic periodontitis
Periodontal trauma is one of the initiating factors in the occurrence of hemorrhage and the development of ischemia, which directly leads to the formation of pulp necrosis. The focus of necrosis attracts bacteria, colonizes them and infects the periodontium. With an increase in the number of microorganisms, acute inflammation begins. Traumatic periodontitis develops.
With chronic long-term trauma, periodontal restructuring occurs gradually, first due to its adaptation, then as chronic inflammation with lacunar resorption of the compact lamina.
The main reason for the development of pathology is the inflammatory response. As a result of occlusal trauma, inflammatory mediators are produced in the pulp; they are considered a protective reaction to mechanical aggression. They disrupt microcirculation and increase vascular permeability. The pulp dies.
When pulp necrosis reaches the apical periodontium, due to its cytotoxic effect, interleukins activate osteoclasts and bone resorption.
Causes
In a vital tooth (in which the nerve has not been removed), periodontitis appears most often due to microorganisms penetrating the periodontium through the pulp, that is, it is usually a consequence of untreated pulpitis or caries. But it should be noted that periodontitis can also occur due to, for example, a crack in the root of a tooth or in case of injury in the oral cavity - due to falls or blows; and even a minor minor injury can lead to a severe form of chronic periodontitis. In rare cases, periodontitis occurs because the doctor misdiagnosed the patient and prescribed the wrong treatment. Thus, the periodontium becomes inflamed under the influence of irritating drugs: arsenic, formalin, phenol. Sometimes periodontitis occurs due to an allergic reaction, which causes a local immunological reaction. And finally, it has been noted that the risk of periodontitis increases sharply in people who smoke - cigarette smoke contains various pathogenic substances that promote periodontal inflammation. The development of periodontitis is also possible when infection penetrates from the lateral surface of the root through a bone “pocket” formed due to gum disease, exposed roots and the presence of dental plaque.
In a non-vital tooth (in which the nerve has already been removed and the canals are filled), periodontitis most often develops due to the complexity of the anatomical structure of the root system, many isthmuses and undercuts that cannot be completely processed and disinfected. This is the most common cause of the development of granulomas or cysts. Unfortunately, not all doctors use high-precision research methods before starting dental treatment, such as computed tomography, which allows you to accurately determine the number of roots and canals, their shape and structure. If such an assessment is not possible, the risk of missing an additional channel increases, in which microorganisms will remain and continue to cause chronic inflammation.
Medicinal periodontitis
Drug-induced periodontitis develops when aggressive liquids or drugs, such as arsenic paste, formalin, tri-cresol formalin, and phenol, enter the periodontium. Penetration into the periodontium occurs through the root canal.
This also includes periodontitis, which develops in response to the removal of phosphate cement, resorcinol-formalin paste, pins and other filling materials into the periodontium during the treatment of pulpitis. Drug-induced periodontitis also includes periodontitis due to allergies as a result of the use of drugs that can cause a local immune response (antibiotics, eugenol, etc.).

Foreign bodies
Gutta-percha, paper pins, calcium residues and a wide variety of other things can be found in the periapical tissues.
The apical periodontium always reacts to foreign bodies. They can enter through the root canal, through an injured mucous membrane or periodontal pocket.
In the case of paper pin penetration, it should be remembered that the human body does not know how to process cellulose, so the foreign body is surrounded by a bacterial plaque, which maintains inflammation.
Gutta-percha is a biocompatible material. However, at the same time it can give a reaction from the apical periodontium. Studies in guinea pigs have shown that large particles of gutta-percha are encapsulated and surrounded by collagen fibers, while small particles support a local tissue reaction. And magnesium and silicon, which are contained in excess gutta-percha, can cause resorption.

Treat or remove?
The most difficult question that faces the doctor and the patient. What does the decision depend on? From many factors:
- Experience, knowledge and skills of the doctor, equipment of the clinic. There is no need to explain anything here
- The desire and capabilities of the patient. Treatment of periodontitis, especially in exacerbation, will require certain financial costs from the patient and several visits to the clinic
- Size and location of inflammation. There are lesions on one tooth, or they spread to several neighboring teeth and even cause inflammation in the maxillary sinus
- The significance of the tooth. It is clear that the “wisdom tooth” will most likely be removed, and they will try to save the front one
- Possibility of subsequent restoration. It happens that such teeth are destroyed below the gum level and it is no longer possible to restore them with a filling or crown
And in order not to make such difficult decisions, to save your teeth and money, visit the dentist once every six months for a check-up.

The article material was approved by the doctor: Feshchenko (Kashirova) Evgenia Aleksandrovna Dentist-therapist
16 years
Diagnosis of chronic apical periodontitis
Diagnosis of chronic apical periodontitis is similar to that in the case of acute apical periodontitis. This means we use basic and additional diagnostic methods.
The main ones include clarifying the patient’s complaints, medical history, probing, percussion, palpation and determining tooth mobility.
The patient’s complaints are most often absent, but they may complain of discomfort while eating when biting.
Probing is painless, palpation of the mucous membrane in the apical area is also painless. Percussion is weakly positive.
Additional special methods include determining the electrical excitability of the pulp (reduced to 200 μA), determining occlusion (the presence or absence of a traumatic factor), fistula tract, and temperature tests.
NB! We definitely do an X-ray examination.