Epidemiology
To date, about 80 species of bacteria of the genus Clostridium have been described. The cause of gas gangrene in humans is only pathogenic species of clostridia: Clostridium perfringens (70 - 80% of all cases of the disease), Clostridium novi and Clostridium septicum. Other types of pathogenic bacteria of the genus Clostridium have also been described, but they are much less common. All microorganisms are obligate anaerobes - they grow and reproduce in the absence of oxygen.
Under unfavorable conditions, bacteria form spores. They can remain in this state for a significant amount of time. The spores are resistant to sunlight, drying and high temperature. The growth and development of clostridia occurs only under anaerobic conditions. Humans and all types of animals are susceptible to the disease.
Sources of infection
Clostridia are constantly present in the soil, intestines of humans and herbivores; in some cases, with poor hygiene, bacteria can be found on the skin.
Transmission routes
Gas gangrene develops when clostridia infect extensive crushed wounds (gunshot wounds, lacerations, bruises), most often the lower extremities and torso, and wounds of the large intestine. Bacteria penetrate damaged tissues with soil, dust, through scraps of clothing, shell fragments, during surgical interventions, drug injections, and out-of-hospital abortions. In mine and transport injuries, injuries often occur in the buttocks and thighs. Persons injured by cattle, pigs, sheep and goats are susceptible to the disease. The wounds become contaminated with animal dung. In some cases, the disease develops from small but contaminated cuts. The disease develops quickly. Its first signs appear from the first day of injury.
Rice. 2. 90% of all cases of gas gangrene are caused by Clostridium perfringens.
Features of diseases caused by clostridia
The main distinguishing feature of all clostridioses is the clear expression of necrotic and toxic factors that prevail over inflammatory processes. Therefore, the characteristic symptoms of diseases of this group are swelling, necrotic lesions and gas formation in the tissues.
Pseudomembranous colitis
The appearance of pseudomembranous colitis, the causative agent of which is Cl. difficile is often recorded in hospital settings or after undergoing a long course of antibiotic therapy. This is explained by the fact that clostridia are immune to most antimicrobial drugs and disinfectants that have a detrimental effect on other microorganisms. Against the background of a decrease in the amount of healthy microflora, enterocolitis caused by Clostridium difficile develops. They manifest themselves with the following symptoms:
- severe diarrhea with mucus in the stool;
- increased body temperature;
- nausea and vomiting;
- abdominal pain;
- increased fatigue;
- headache.
The mild form of the disease goes away immediately after stopping the antibiotic. When transitioning to a severe form, the following occurs:
- dehydration;
- circulatory disorders;
- the appearance of blood in the stool;
- convulsions;
- decrease in the total volume of urine excreted.
A complication of pseudomembranous colitis is intestinal rupture followed by peritonitis, leading to death.
The peculiarity of the pathology is relapses, which appear 3-27 days after recovery.
Botulism
The most dangerous infection is botulism, since botulinum toxins produced by Cl. botulinum, stronger than other clostridia. Getting into the human digestive tract with food, these poisons are quickly absorbed into the blood, causing severe damage to the nervous system, ending without treatment in paralysis of the respiratory center and death.
Tetanus
Cl. tetani produces tetanus toxin, which causes tonic muscle contractions. In addition, against the background of the underlying disease, clostridium provokes ruptures of ligaments, tendons and muscles, bone fractures, pulmonary edema and pneumonia.
A feature of tetanus clostridiosis in infants is the ability of the bacillus to secrete exotoxins in the digestive tract and provoke clinical signs of botulism. In a child’s body, after a year, the microorganism loses this property.
Gas gangrene
An infection that affects the skin. Very often develops after injuries, wounds, amputations. Gangrene is an affected, dead area of skin that gradually invades healthy areas.
Clostridia of gas gangrene include Clostridium perfringens, Cl. novyi, Cl. septicum and some other strains of bacteria. The disease is characterized by a high rate of development, with clinical signs appearing already 6 hours after infection. These include:
- fever;
- blue discoloration of the skin in the area of penetration of bacilli;
- pain and swelling of the wound edges;
- release of gas bubbles with an unpleasant putrid odor from the wound when pressure is applied;
- crepitus of the affected area upon palpation.
Doctors identify four specific symptoms of gas gangrene:
- Melnikov's symptom. A ligature applied to an infected limb, after a quarter of an hour, strongly digs into the skin due to the rapid increase in tissue volume.
- Spatula sign. When applying light blows with a metal spatula, a tympanic crunching sound is heard.
- Champagne cork symptom. Removing the tampon from the wound is accompanied by a popping sound.
- Krause's sign. Accumulations of gas bubbles between muscle fibers have a “herringbone” shape on an x-ray.
Clostridia
Clostridia are facultative anaerobes (bacteria grow and multiply in the absence of oxygen). They are saprophytes. They free nature from dead organic material through the processes of fermentation and decay. They are present in the intestines of animals and humans, where they feed on organic debris, but do not invade (penetrate) living healthy tissue.
Clostridia are rod-shaped bacteria (bacilli) that produce a number of toxins and enzymes that form spores under unfavorable conditions. Pathogenic forms of pathogens cause such serious diseases as tetanus, botulism and gas gangrene. They produce the most powerful poisons known - tetanospasmin (Clostridium tetani), botulinum toxin (Clostridium botulinum) and a-toxin (Clostridium perfringens).
The main causative agents of gas gangrene are Clostridium perfringens (70 - 80% of cases), Clostridium novyi (20 - 43%) and Clostridium septicum (5 - 18%). Much less common are types of clostridia such as Clostridium histolyticum, Clostridium sordellii, Clostridium difficile, Clostridium fallax, etc.
Gas gangrene is almost always a mixed infection. Often, during infection, aerobic microorganisms join clostridia: streptococci, staphylococci, Escherichia coli, Proteus, etc.
Taxonomy of clostridia
The causative agents of gas gangrene belong to the Bacillaceae family, genus Clostridium. The genus Clostridium includes numerous (about 80) species of clostridia.
Morphology
The causative agent of gas gangrene is a gram-positive rod. Bacteria are usually mobile and have a capsule. Some types of clostridia lack a capsule but have flagella. The largest in size of all clostridia is C. novyi. All other bacteria are much smaller.
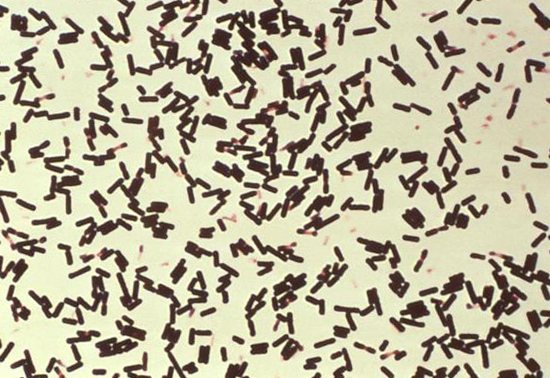
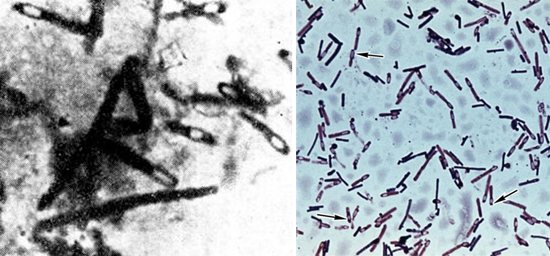
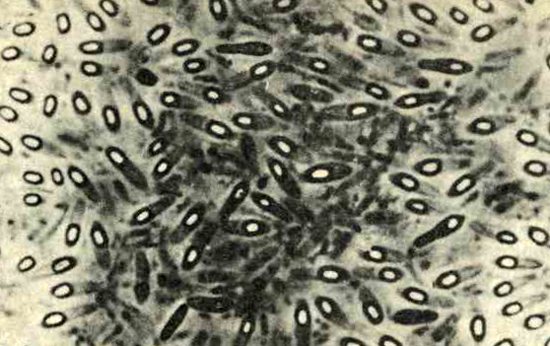
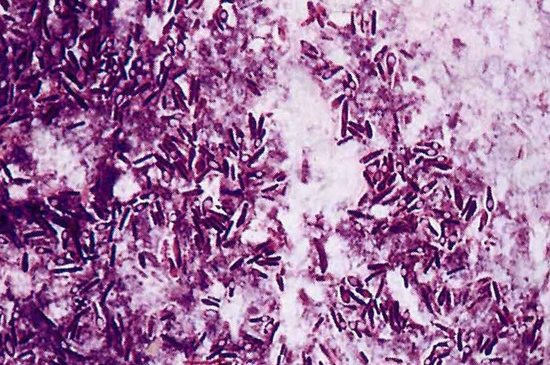
Rice. 3. The causative agent of gas gangrene Clostridium perfringens (pure culture smear) under a microscope.
Clostridia sporulation
Clostridia under unfavorable conditions form spores located centrally or subterminally. When the spores are centrally located, the rod becomes like a spindle (closter - spindle).
Clostridia spores are resistant to drying, high temperature and sunlight. They are able to survive in saline solutions, tolerate prolonged boiling, freezing, ultraviolet irradiation, radiation and vacuum. The spores exhibit resistance to a range of toxic and disinfectants.
Bacteria can remain in a spore-like state for hundreds of years. Under favorable environmental conditions, spores germinate. The germination process lasts 4 - 5 hours.
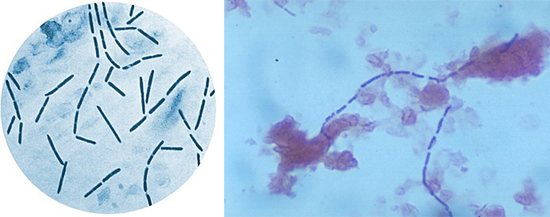
Rice. 4. Clostridium perfringens spores.

Rice. 5. The photo shows a clostridia spore. At its core there is a resting vegetative cell.
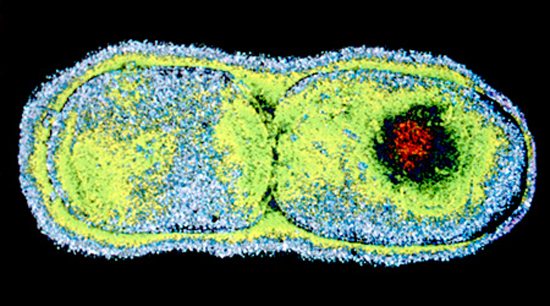
Rice. 6. Division of the vegetative cell after spore germination.
Biochemical properties and toxins of clostridia
The causative agents of gas gangrene ferment carbohydrates with the formation of gas and acid, form complex exotoxins - 12 enzymes (toxins) and enterotoxin, which causes intestinal inflammation. Bacteria are divided into six serovars (A, B, C, D, E, F), each of which has its own necrotic characteristics. Serovar A is the main causative agent of gas gangrene. It forms up to 90% of all cases of the disease. The main targets for toxins are cell membranes. Enzymes promote their breakdown, followed by swelling and autolysis (self-dissolution).
Bacteria types A and C produce enterotoxins, which cause foodborne illnesses and necrotic enteritis.
Laboratory diagnostics
Diagnosis of clostridiosis is based on anamnestic data and clinical symptoms. It is also determined in detail what food the patient has consumed recently, whether he has undergone a course of antibiotic therapy, or whether he has been injured. The final diagnosis is made only after laboratory tests:
- Bacterioscopy of scrapings and smears of primary material.
- Identification of the pathogen by inoculating pathological material on nutrient media.
- Detection of pathogenicity of microbes using a bioassay.
- Instrumental diagnostics.

A small amount of bacteria is found in the stool, and this is normal.
The detection of clostridia in a child’s stool does not confirm the diagnosis, since they are part of the normal intestinal microflora. But their number should not exceed:
- 103 – 104 CFU/g – in children of the first year of life;
- 105 CFU/g - from 1 year to 16 years;
- 106 CFU/g – over 16 years of age.
The diagnosis is confirmed if stool analysis reveals:
- increased content of clostridia combined with a decrease in the amount of beneficial microflora;
- the presence of Clostridium difficile toxins A and B in feces;
- presence of Cl.perfringeus;
- presence of Cl. botulinum (only in infants of the first year of life).
But some pathogenic clostridia in feces do not have diagnostic value, since, while in the intestines, they cannot produce toxins that cause the disease. These microbes include Cl.tetani, the rods of which may accidentally end up in the stool.
To identify clostridia, cultures on nutrient media are used. After the colonies begin to grow, their color, shape, evenness of edges, ability to hemolysis and gas formation are taken into account.

Biomaterial from sick or dead farm animals is examined in accordance with GOST 26503-85 standards.
In food products, the quantity and species of sulfite-reducing clostridia are determined according to the methods specified in GOST 29185-91. The greatest danger to humans is posed by canned meat, fish and vegetables, in which anaerobic conditions are created.
According to the requirements of existing GOSTs, the presence of sulfite-reducing clostridia and their toxins in food is unacceptable, as it leads to severe poisoning and, in many cases, death.
Clostridium perfringens is the main causative agent of gas gangrene
Gas gangrene, food poisoning and necrotic enteritis in humans and animals are caused by Clostridium perfringens types A, C and D. Similar diseases, but only in animals are caused by Clostridium perfringens types B, C, D and E.
The pathogen was first discovered by Welch and Nettal in 1892.
Morphology of Clostridium perfringens
Bacteria look like rods with rounded ends. They are large, measuring 3-9 × 0.9-1.2 microns. Fixed. They are located singly. Clostridia isolated from pure cultures have a capsule. Gram stained purple. Old cultures are losing this ability. They form spores that persist in the environment for many decades.
Rice. 7. Smear from a pure culture of Clostridium perfringens (photo on the left). Bacterial spore (photo on the right).
Rice. 8. The photo shows the bacteria Clostridium perfingens and spores.
Cultivation of Clostridium perfringens
Clostridium perfringens are strict obligate anaerobes, chemoorganoheterotrophs. They grow on simple nutrient media - blood sugar agar and Kitta-Tarozzi medium. The growth of bacteria is accompanied by gas formation and a decrease in pH towards the acidic side.
- On sugar-blood agar, bacteria form smooth, shiny, round shapes (S-colonies), or grayish colonies, flat, rough with jagged edges (R-colonies). A hemolysis zone forms around the colonies. When exposed to air, colonies acquire a greenish color. Colonies in the thickness of the agar acquire a lenticular shape.
- When growing in liquid media (Kitta-Tarozzi medium), turbidity is formed with intense gas formation. Subsequently, the medium clears and a whitish plate-like sediment falls to the bottom.
- When growing on bile agar, precipitation zones form.
- When growing on milk, after 4 hours intensive coagulation is noted, and the curd, due to gas formation, acquires a holey structure and often bounces up. A similar reaction is used in laboratories for rapid diagnostics.
- When growing in meat broth, bacteria produce acetic and butyric acids, as well as large amounts of gases such as H2S, NH3 and CO.
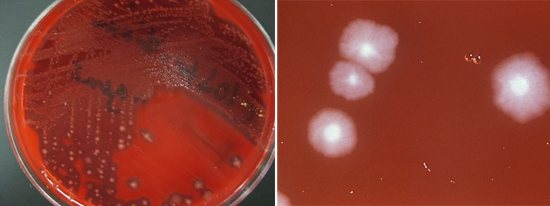
Rice. 9. Clostridium perfringens colonies on blood agar.
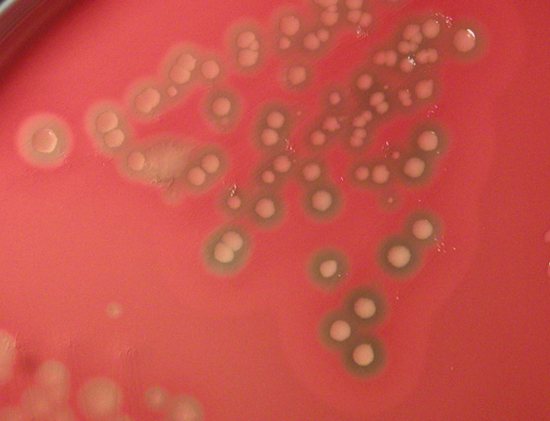
Rice. 10. C. perfringens is identified by its characteristic “double zone” of hemolysis.
Biochemical properties of clostridia
The powerful enzymatic activity of bacteria gave them the epithet perfringens, which means breaking, breaking through. Due to intense gas formation, swelling of damaged tissues and ruptures of nutrient media occur. Clostridium perfringens produce a huge number of saccharolytic enzymes that ferment glucose, lactose, maltose and sucrose with the subsequent formation of acid and gas. They intensively curdle milk, followed by the formation of a spongy, coarse-celled clot (“storm reaction”).
Bacteria decompose gelatin, egg whites, coagulated whey and collagen. Does not decompose casein.
During acetobutyrate fermentation, Clostridium perfringens synthesize butyric acid, reduce nitrates to nitrites, and form lecithinase.
Rice. 11. Determination of lecithinase activity. Around the colonies, zones of a turbid halo consisting of precipitated lipids are clearly visible.
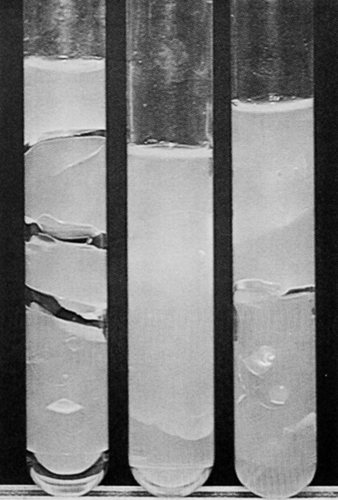
Rice. 12. In the left test tube is a culture of Clostridium perfringens on sugar agar. As a result of intense gas formation in the helium-like medium, rupture zones formed.
Toxin formation
The bacteria Clostridium perfringens, according to the spectrum of toxins (enzymes) they produce, are divided into types A, B, C, and E. Gas gangrene and foodborne toxic infections are more often associated with type A, necrotizing enterocolitis - with type C. The concept of “toxin” unites about 12 identified today toxins (enzymes) and enterotoxin. The release of enzymes in the area of damaged tissue leads to the breakdown of complex substances and disruption of cellular permeability, as a result of which cells swell and melt.
Main exotoxins of clostridia
- α-toxin (phospholipase C). It is produced more intensively by clostridia type A. It is the main and most powerful toxin. The enzyme hydrolyzes (breaks down) phospholipids of cell membranes, which leads to destruction (lysis) of cells. It has a dermatonecrotic and lethal effect, and is the main factor in interstitial invasion and intravascular hemolysis - a symbol of fatal clostridial toxinemia. Has lecithinase activity.
- b-toxin (cytotoxin). Mainly produced by clostridia types B and C. It has a dermatonecrotic and lethal effect and does not cause hemolysis. It causes the development of necrotic enteritis.
- Theta toxin. It has hemolytic and dermatonecrotic effects. Sensitive to oxygen. It is similar to O-streptolysin of streptococci.
- v-toxin (proteinases). They disrupt protein synthesis reactions by splitting nucleic acids.
- p-toxin (collagenase and gelatinase). Produced by clostridia types A, C and E, as well as some strains of bacteria type D. Enzymes break down gelatin and collagen fibers of connective tissue. They have a necrotizing and lethal effect.
- Mu-toxin (hyaluronidase). It is a factor in the penetration of clostridia. Enzymes break down acidic mucopolysaccharides and hyaluronic acid.
- Nu-toxin (DNA-za). Destroys cellular DNA.
- q-hemolysin. With the participation of complement, it destroys red blood cell membranes.
- Fibrinolysin. Dissolves fibrin fibers.
- Hemagglutinin. With its participation, the agglutination reaction of erythrocytes occurs.
- y-toxin (proteinase). Its action resembles fibrinolysin. Does not break down native (natural) collagen, but destroys azocoll (denatured collagen), casein and gelatin.
- Delta toxin (elastase). It is a proteolytic enzyme. Breaks down proteins and peptides.
- Sigma toxin. They produce clostridia types B and C. It has a lethal effect and exhibits hemolytic activity.
- Omega toxin. Produced mainly by clostridia type C. It has a dermatonecrotic and lethal effect.
- Epsilon is a toxin. Produced by clostridia types B and D, l-toxin - by clostridia type E. They exhibit a lethal and dermatonecrotizing effect.
- y- and n-toxins. The biochemical nature of these toxins remains unknown.
- p-toxin. It is a tissue permeability factor.
Enterotoxin of the causative agent of gas gangrene
Enterotoxin is produced by clostridia types A and C.
- Clostridium perfringens enterotoxin strain A is a heat-labile protein released in the small intestine during spore formation. When exposed to it, capillaries expand, their permeability increases, the secretion of water, sodium and chloride ions increases, and the membranes of enterocytes are damaged.
- The enteropathogenicity of Clostridium perfringens type C is associated with b-toxin. The disease occurs as necrotizing enteritis.
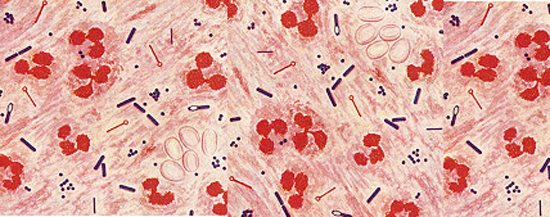
Rice. 13. Under unfavorable conditions, some bacteria form spores. They help the microorganism survive in unfavorable conditions for many decades. The photo shows spores of bacteria of the genus Clostridium.
Lecture No. 11. Clostridia
Lecture No. 11.
Clostridia.
General characteristics of pathogenic anaerobic bacteria.
Obligate anaerobes are microorganisms that live only in conditions of extremely low oxygen content - in soil, silt of water bodies, and the intestines of vertebrates and humans. In warm-blooded animals, anaerobes make up the bulk of the normal intestinal microflora and determine a number of the most important functions of the body.
A heterogeneous group of anaerobic gram-positive bacteria is differentiated primarily by its ability to form spores and morphological characteristics. In human pathology, anaerobic spore-forming bacteria of the genus Clostridium are of greatest importance. Among non-spore-forming gram-positive anaerobes, the family of lactobacilli (Lactobacillaceae) and the genus of bifidobacteria (Bifidibacterium) are of medical importance, and in pathology - non-spore-forming gram-negative anaerobes of the genera Bacteroides (bacteroides) and Fusobacterium (fusobacteria).
Genus Clostridium.
These are mobile large rods (most species), form oval or round endospores, giving clostridia (Greek kloster - spindle) a wind-like shape. The diameter of the spore is greater than the diameter (diameter) of the vegetative cell. Gram-positive, chemoorganotrophs. Strict anaerobes.
Based on their environmental and pathogenic properties, three groups of clostridia can be distinguished: - saprophytes that cause fermentation (saccharolytic) processes;
— saprophytes that cause decay processes (proteolysis);
- pathogenic species - due to their biochemical properties they can cause processes of rotting and fermentation. Pathogenic species of clostridia are conditionally divided into three groups - causative agents of traumatic (wound) clostridiosis
- gas gangrene, tetanus, pathogens
of enteral clostridiosis
(toxic infections) - botulism, pseudomembranous colitis and species that
cause pathological processes only in associations
with each other or with other microorganisms.
Modern taxonomy distinguishes five groups of clostridia based on the location of the spores, the ability to hydrolyze gelatin, and the presence of special conditions for growth. All species pathogenic for humans ferment gelatin, differing in the location of the spores - terminal (in the form of tennis rackets) in the fourth group (C.tetani - the causative agent of tetanus), subterminal (spindle) in the second group (other pathogens: C.botulinum - the causative agent of botulism, C .perfringens and other causative agents of gas gangrene, C.difficile - the causative agent of pseudomembranous colitis).
Microbiology of gas gangrene.
Gas gangrene is an anaerobic polyclostridial (i.e. caused by various types of clostridia) wound (traumatic) infection. The main importance is C.perfringens, less often - C.novyi, as well as other types of clostridia in persistent associations with each other, aerobic pyogenic cocci and putrefactive anaerobic bacteria.
C.perfringens is a normal inhabitant of the intestines of humans and animals and enters the soil with feces. It is a causative agent of wound infection - it causes disease when the pathogen enters wounds under anaerobic conditions. It is highly invasive and toxicogenic. Invasiveness is associated with the production of hyaluronidase and other enzymes that have a destructive effect on muscle and connective tissue. The main pathogenicity factor is exotoxin
, which has hemo-, necro-, neuro-, leukotoxic and lethal effects.
In accordance with the antigenic specificity of exotoxins, serotypes
of the pathogen are distinguished. Along with gas gangrene, C. perfringens causes foodborne toxic infections (they are based on the action of enterotoxins and necrotoxins).
Features of pathogenesis. Unlike purulent diseases caused by aerobes, with anaerobic infection it is not inflammation that predominates, but necrosis, swelling, gas formation in tissues, poisoning by toxins and tissue breakdown products.
Clostridia are necroparasites that actively create anaerobic conditions and cause tissue necrosis, i.e. conditions for its reproduction. Necrosis of muscle and connective tissue is a consequence of the necrotoxic action of toxins and enzymes, gas formation in tissues is the result of the enzymatic activity of clostridia. The general effect of toxins (general intoxication) manifests itself mainly in neurotoxic effects.
Immunity is predominantly antitoxic.
Laboratory diagnostics include bacterioscopy of wound discharge, isolation and identification of the pathogen, detection and identification of the toxin in biological samples using a neutralization reaction with specific antitoxic antibodies.
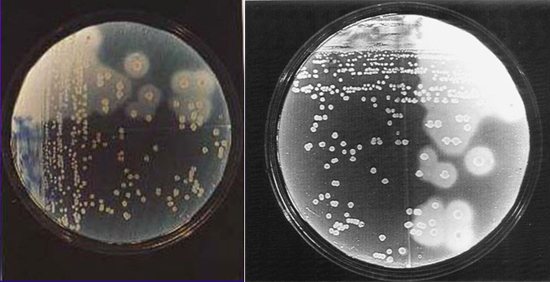
A feature of all spore-forming bacteria is resistance to heat, which is taken into account in laboratory diagnostics - heated and unheated samples are examined. When testing for clostridia, one (unheated) sample is inoculated on liquid media (casein or meat) and solid differential diagnostic media (Wilson-Blair, Willis-Hobbs). Other parts of the source material are heated at +80 and +100°C for up to 20 minutes and inoculated into liquid storage media. Grown cultures of gram-positive rods are subcultured onto solid differential diagnostic media.
Willis-Hobbs medium contains, in addition to nutrient agar, lactose, indicator, egg yolk and skim milk. Differentiation of clostridia species is carried out by the change in the color of the indicator to red (lactose fermentation) and the presence of a zone (halo) of opalescence around the colonies (lecithinase activity). C. perfringens colonies are indicator-colored and have an opalescent halo.
Prevention and treatment. The basis for preventing gas gangrene is timely and correct surgical treatment of wounds. In case of severe wounds, antitoxic serums are administered against the main types of clostridia in a dose of 10 thousand IU, for medicinal purposes - in a dose of 50 thousand IU.
Clostridium difficile.
This is a representative of the normal intestinal microflora, rarely causes gas gangrene, and is the causative agent of pseudomembranous enterocolitis -
the result of irrational antibiotic therapy and the development of dysbiosis due to the dominance of this pathogen. When using antibiotics (especially clindomycin, ampicillin and cephalosporins) and cytostatics, a deep imbalance of the intestinal microflora and colonization with C. difficile occurs. The toxic component of the pathogenicity of this type of clostridia consists of an enterotoxin and a cytotoxin. The pathogen exhibits high resistance to broad-spectrum antibiotics, which contributes to massive colonization of the intestine and the secretion of large amounts of toxins that cause changes in the intestinal wall. Pseudomembranous colitis is a hospital infection that dominates among intestinal lesions, but is difficult to detect bacteriologically (difficulties in isolating and studying anaerobes).
Microbiology of tetanus.
Tetanus is an acute wound infection characterized by damage from a neurotoxin
motor cells of the spinal cord and brain, which manifests itself in the form of convulsions of the transversely striated muscles. People and farm animals get sick. Soil, especially contaminated with human and animal excrement, is a constant source of tetanus infection.
The causative agent is C.tetani, a large spore-forming gram-positive rod. The spores are located terminally (type of drumstick), and are mobile due to flagella - peritrichs. Obligatory anaerobe. The spores are very resistant.
Antigenic properties. The pathogen has O- and H-antigens.
Pathogenicity factors. The main factor is the strongest exotoxin. There are two main fractions of it: tetanospasmin (neurotoxin) and tetanolysin (hemolysin). The neurotoxin enters the central nervous system into the areas of myoneural synapses, is transmitted from neuron to neuron in the area of synapses, accumulates in the motor areas of the spinal cord and brain, and blocks synaptic transmission. Death occurs from paralysis of the respiratory center, asphyxia (damage to the muscles of the larynx, diaphragm, intercostal muscles) or paralysis of the heart.
Laboratory diagnostics. Microbiological diagnostics includes bacterioscopy of starting materials, culture to isolate the pathogen and its identification, and detection of tetanus toxin.
The material to be examined is from a patient (especially in places where the pathogen enters the body - from wounds), a corpse (blood, pieces of liver and spleen), dressing and suture surgical material, soil, dust and air samples.
Isolation of the pathogen is carried out according to the standard scheme for anaerobes, using various solid and liquid (Kitt-Tarozzi medium) media, identification is based on morphological, cultural, biochemical and toxigenic properties.
The simplest and most effective method of microbiological diagnostics is a bioassay on white mice. One group is infected with the test material, the second (control) is infected after mixing the samples with antitoxic tetanus serum. In the presence of tetanus toxin, the experimental group of mice died, while the control group remained alive.
Treatment and emergency prevention. Donor tetanus immunoglobulin (antitoxin), antitoxic serum (350 IU/kg), antibiotics (penicillins, cephalosporins) are used. To create vaccine immunity, tetanus toxoid is used, most often as part of DTP vaccines (tetanus toxoids, diphtheria and killed pertussis bacilli).
Microbiology of botulism.
Botulism is a severe foodborne illness associated with the consumption of products contaminated with C.botulinum and characterized by specific damage to the central nervous system. It got its name from Lat. botulus - sausage.
Properties of the pathogen. Large polymorphic gram-positive rods, motile, have peritrichous flagella. The spores are oval and located subterminally (tennis racket). They produce eight types of toxins, differing in antigenic specificity, and accordingly, 8 types of pathogens are distinguished. Among the most important characteristics is the presence or absence of proteolytic properties (hydrolysis of casein, production of hydrogen sulfide).
The toxin has a neurotoxic effect. The toxin enters the body with food, although it can probably accumulate when the pathogen multiplies in the tissues of the body. The toxin is heat labile, although boiling for up to 20 minutes is necessary for complete inactivation. The toxin is quickly absorbed in the gastrointestinal tract, penetrates the blood, and selectively acts on the nuclei of the medulla oblongata and ganglion cells of the spinal cord. Nervous and paralytic phenomena develop - swallowing disorders, aphonia, dysphagia, ophthalmo-plegic syndrome (strabismus, double vision, drooping eyelids), paralysis and paresis of the pharyngeal and laryngeal muscles, cessation of breathing and cardiac activity.
Laboratory diagnostics. The principles are common to clostridia. The pathogen is isolated and identified, but of greatest practical importance is the detection of botulinum toxin and determination of its serotype.
To isolate the pathogen, samples are sown on dense media and Kitt-Tarozzi accumulative medium (part of the material is preheated at +85o C).
To study the toxin, bioassays are carried out on white mice (one experimental group and four control groups with a mixture of the material and the corresponding antiserum - types A, B, C and E). All batches die, except one (with an antiserum homologous to the type of toxin). It is also possible to determine the toxin in RNGA with an antibody diagnosticum.
Treatment and prevention. It is based on the early use of antitoxic serums (polyvalent or, when the type is established, homologous). Prevention is based on a sanitary and hygienic regime when processing food products. Homemade canned mushrooms and other products stored under anaerobic conditions are especially dangerous.
Streptococci.
The family Streptococcaceae includes seven genera, of which the most important for humans are streptococci (genus Streptococcus) and enterococci (genus Enterococcus). The most significant species are S.pyogenes (group A streptococci), S.agalactiae (group B streptococci), S.pneumoniae (pneumococcus), S.viridans (viridans streptococci, mutans biogroup), Enterococcus faecalis.
Morphology. Streptococci (from the Greek streptos - chain and coccus - grain) are gram-positive cytochrome-negative bacteria of spherical or ovoid shape, growing more often in the form of chains, mostly immobile, do not have spores. Pathogenic species form a capsule (in pneumococcus it has diagnostic value). Facultative (most) or strict anaerobes.
Cultural properties. Streptococci do not grow well on simple nutrient media. Typically media containing blood or serum are used. Sugar broth and blood agar containing 5% defibrinated blood are more often used. In the broth, growth occurs near the bottom - near the wall in the form of a crumbly sediment; the broth is often transparent. On dense media they often form very small colonies. Optimum temperature +37o C, pH - 7.2-7.6. On solid media, group A streptococci form three types of colonies:
- mucoid (resemble a drop of water) - characteristic of virulent strains that have a capsule;
- rough - flat, with an uneven surface and scalloped edges - characteristic of virulent strains that have M antigens;
- smooth - characteristic of low-virulent strains.
They prefer a gas mixture with 5% CO2. Capable of forming L-forms.
To differentiate streptococci, various characteristics are used: growth at +10o and 45o C, growth on a medium with 6.5% NaCl, growth on a medium with a pH of 9.6, growth on a medium with 40% bile, growth in milk with 0.1% methylene blue, growth after heating for 30 minutes. at 60o C. The most common S.pyogenes belongs to group 1 (all signs are negative), enterococci (group 3) - all signs are positive.
There are a number of classifications of streptococci. The simplest classification is based on the growth characteristics of these microorganisms on sheep blood agar (in relation to red blood cells).
Beta-hemolytic streptococci
when growing on blood agar, they form a clear zone of hemolysis around the colony,
alpha - hemolytic -
partial hemolysis and greening of the medium (conversion of oxy- to methemoglobin),
gamma - hemolytic -
hemolysis is invisible on blood agar. Alpha-hemolytic streptococci are called S.viridans (greening) due to the green color of the medium.
Antigenic structure. Serological classification is of practical importance for differentiating streptococci with a complex antigenic structure. The classification is based on group-specific polysaccharide cell wall antigens
. There are 20 serogroups, designated by capital letters. The most important are streptococci of serogroups A, B and D.
Streptococci of serogroup A have type-specific antigens - proteins M, T and R. Based on the M antigen, hemolytic streptococci of serogroup A are divided into serovars (about 100).
Streptococci have cross-reacting antigens with antigens of the cells of the basal layer of the skin epithelium, epithelial cells of the cortical and medullary zones of the thymus. An antigen (receptor II) was also found in the cell wall of streptococci that can interact with the Fc fragment of IgG.
Factors of pathogenicity of streptococci.
1. Protein M is the main factor. Determines adhesive properties, inhibits phagocytosis, determines type specificity, and has superantigen properties. Antibodies to M protein have protective properties.
2. Capsule - masks streptococci due to hyaluronic acid, similar to hyaluronic acid in host tissues.
3. C5a - peptidase - breaks down C5a - a complement component, which reduces the chemoattractive activity of phagocytes.
4. Streptococci cause a pronounced inflammatory reaction, largely due to the secretion of more than 20 soluble factors - enzymes (streptolysins S and O, hyaluronidase, DNase, streptokinase, protease) and erythrogenic toxins.
Erythrogenin -
scarlet fever toxin, which, through immune mechanisms, causes the formation of a bright red scarlet fever rash. There are three serological types of this toxin (A, B and C). The toxin has pyrogenic, allergenic, immunosuppressive and mitogenic effects.
Genetics. Mutations and recombinations are less pronounced than in staphylococci. Capable of synthesizing bacteriocins. Phages are not used for differentiation.
Epidemiological features. The main sources are patients with acute streptococcal infections (tonsillitis, pneumonia, scarlet fever), as well as convalescents. The mechanism of infection is airborne, droplet, less often contact, very rarely alimentary.
Clinical and pathogenetic features. Streptococci are inhabitants of the mucous membranes of the upper respiratory tract, digestive and urinary genital tracts, causing various diseases of an endo- and exogenous nature. Local _
(tonsillitis, caries, tonsillitis, otitis, etc.) and
generalized
infections (rheumatism, erysipelas, scarlet fever, sepsis, pneumonia, streptoderma, etc.). The development of certain forms depends on a number of conditions, including from the entrance gate, various pathogenicity factors, the state of the immune system (antitoxins and type-specific M antibodies play a special role).
A special position in the genus Streptococcus is occupied by the species S.pneumoniae (pneumococcus) - the etiological agent of lobar pneumonia, acute and chronic inflammatory diseases of the lungs. It differs from other streptococci in morphology (usually diplococci are in the shape of a candle flame, with flat ends facing each other, have a pronounced capsule), antigenic specificity (they have 83 serovars for the capsular polysaccharide antigen), high sensitivity to bile and optochin, and cause alpha hemolysis. The main factor of pathogenicity is the polysaccharide capsule.
Scarlet fever is caused by various serotypes of beta-hemolytic streptococci that have M-antigen and produce erythrogenin (toxigenic streptococci of serogroup A). In the absence of antitoxic immunity, scarlet fever occurs, and in the presence of sore throat.
Laboratory diagnostics. The main diagnostic method is bacteriological. Material for research - blood, pus, mucus from the throat, plaque from the tonsils, wound discharge. The decisive factor in the study of isolated crops is the determination of the serogroup (species). Group-specific antigens are determined in the precipitation reaction, latex - agglutination, coagglutination, ELISA and in MFA with monoclonal antibodies (MAbs). Serological methods are more often used to diagnose rheumatism and glomerulonephritis of streptococcal etiology - antibodies to streptolysin O and streptodornase are determined.
Gram-negative aerobic and optionally anaerobic cocci.
The genus Neisseria is of greatest importance, of the species - N.gonorrhoeae - gonococcus and N.meningitidis - meningococcus, the remaining types of Neisseria are commensals.
Morphology. Neisseria are diplococci that resemble coffee beans or beans, adjacent to each other with flattened sides. They are characterized by the presence of a capsule, as well as pili and villi, which facilitate the adhesion of pathogenic neisseria to the epithelium.
Cultural characteristics. For cultivation, pathogenic neisseria require a medium containing blood, blood serum, or human ascitic fluid. Each species selectively ferments carbohydrates. Optimum temperature +37o C, pH - 7.2-7.4. Blood and chocolate agar with the addition of starch are suitable for cultivation; an increased concentration of CO2 and selective components that suppress the growth of accompanying microflora are required.
N.gonorrheae (gonococcus).
Gonococcus is the causative agent of gonorrhea, a sexually transmitted disease with inflammatory manifestations in the genitourinary tract. The substrate for colonization is the epithelium of the urethra, rectum, conjunctiva of the eye, pharynx, cervix, fallopian tubes and ovary.
Diplococci, easily stained with methylene blue and other aniline dyes, are pleomorphic (polymorphism). They are very picky about cultivation conditions and nutrient media. Of the carbohydrates, only glucose is fermented.
The antigenic structure is very variable - phase variations (disappearance of antigenic determinants) and antigenic variations (changes in antigenic determinants) are characteristic. The main antigenic load is carried by determinants of pili and surface proteins. High antigenic variability is associated with a lack of immune protection against re-infection. The greatest antigenic relationship is with meningococci.
Pathogenicity factors. The main factors are pili
, with the help of which gonococci carry out adhesion and colonization of epithelial cells of the mucous membrane of the genitourinary tract, and
lipopolysaccharide
(endotoxin released when gonococci are destroyed). Gonococci synthesize IgAI protease, which breaks down IgA.
Genetics. Genetic variability is characteristic, even throughout the life of one microbial population. The transfer of information is carried out mainly by conjugation. F- and R-plasmids were identified, incl. plasmids carrying the beta-lactamase gene.
Laboratory diagnostics. Bacterioscopic diagnosis includes Gram and methylene blue staining. Typical signs of gonococcus are gram-negative staining, bean-shaped diplococci, and intracellular localization. With antibiotic therapy, chronic gonorrhea and some other cases, both morphological signs and the relationship to Gram staining may change. Luminescent diagnostics using direct and indirect immunofluorescent analysis are more reliable.
Inoculation is carried out on special media (KDS-MPA from rabbit meat or bovine heart with serum, ascites-agar, blood agar). Characteristic signs of gonococcus in bacteriological diagnosis are gram-negative diplococci, colonies of which on solid media have oxidase activity. They ferment glucose, but not maltose or sucrose.
N.meningitidis (meningococci).
Meningococcus is the causative agent of meningococcal infection - a strict anthroponosis with airborne droplet transmission of the pathogen. The main source is media. The natural reservoir is the human nasopharynx. Morphological, cultural and biochemical properties are similar to gonococcus. Differences - they ferment not only glucose, but also maltose, and produce hemolysin. They have a capsule that is larger in size and has a different structure than that of gonococcus.
Antigenic composition. They have four main antigenic systems.
1. Capsular group-specific polysaccharide antigens. Serogroup A strains most often cause epidemic outbreaks.
2. Protein antigens of the outer membrane. Based on these antigens, meningococci of serogroups B and C are divided into classes and serotypes.
3. Genus- and species-specific antigens.
4. Lipopolysaccharide antigens (8 types). They have high toxicity and cause pyrogenic effects.
Pathogenicity factors. Adhesion factors and colonization - pili and outer membrane proteins. Invasiveness factors are hyaluronidase and other produced enzymes (neuraminidase, proteases, fibrinolysin). Capsular polysaccharide antigens that protect microorganisms from phagocytosis are of great importance.
Immunity is persistent, antimicrobial.
Laboratory diagnostics are based on bacterioscopy, culture isolation and its biochemical identification, and serological diagnostic methods. The material is inoculated on solid and semi-liquid nutrient media containing blood, ascitic fluid, and blood serum.
Oxidase-positive cultures are considered to belong to the genus Neisseria. Meningococcus is characterized by fermentation of glucose and maltose. Belonging to a serogroup is determined by an agglutination test (RA). To detect antigens, coagglutination reaction, latex agglutination, ELISA can also be used, for serodiagnosis - RNGA with group-specific polysaccharide antigens
Clostridium novyi
Clostridium novyi is one of the main causative agents of gas gangrene. During the Great Patriotic War, gas gangrene was caused by bacteria of this type in 42% of cases. The pathogen was first isolated and given the name Clostridium oedematiens by E. Segen and M.V. Weinberg in 1891. Later, this type of clostridia was more fully described by the American bacteriologist F. Novi, whose name later began to be called this type of bacteria.
Morphology of Clostridium novyi
Clostridia are rods, large, sometimes slightly curved, measuring 4 - 22 x 1.4 - 2 microns, mobile, have up to 25 flagella, often arranged in chains. The pathogen, like all clostridia, are obligate anaerobes. A capsule is not formed. Gram-stained violet (Gram-positive). Old cultures are losing this ability. They form oval spores located centrally and subterminally.
Rice. 14. Clostridium novyi. Large sticks, arranged singly or in chains.
Cultivation
Clostridium novyi are strict anaerobes. Highly sensitive to oxygen. They grow on simple media: carbohydrate, casein and meat peptone.
- When growing on solid media, translucent, juicy grayish colonies are formed after 48 hours. The edges are uneven. The surface is grainy. Clostridia types A, B and C sometimes form daughter colonies. The colonies are surrounded by a zone of hemolysis. Clostridia type D does not destroy red blood cells.
In the depths of the agar, colonies resemble lumps of cotton wool or snow flakes, often colored brown or yellow.
- When growing in liquid media, gas is formed and the nutrient medium becomes cloudy, and sediment falls to the bottom. The pH shifts to the acidic side due to the formation of H2S and organic acids.
Antigenic structure
Clostridium novyi is identified by the detection of somatic antigens. There are 4 serovars, different in antigenic characteristics and synthesized toxins - serovars A, B, C and D.
Biochemical properties
Serovars types A, B and C ferment fructose, glucose and maltose; serovars type D ferment only glucose. Serovars types A, C and D degrade glycerol. All strains curdle milk and break down gelatin. Type D clostridia produce hydrogen sulfide and indole, other types of bacteria do not.
Clostridium novyi toxins
Clostridium novyi produces a pathogenic enzyme such as phospholipase (a-toxin), as well as b, y, sigma, e and n - toxins that have necrotic, hemolytic and lethal effects. By disrupting the permeability of blood vessels, they lead to the development of jelly-like edema.

Rice. 15. The photo shows gas gangrene.
General information
Clostridiosis (clostridium spp) is an infectious disease with an acute course. It is caused by clostridia - gram-positive anaerobic bacteria that can produce endospores. Thanks to this, they are well preserved in the external environment. It is the varieties of these bacteria that produce the most toxic poisons: botulinum toxin, tetanospasmin, ε-toxin. They cause very serious diseases: tetanus , botulism , gas gangrene , etc. But most often they are affected by the bacterium Clostridium difficile. Normally, these bacteria are part of the microflora of the gastrointestinal tract and genital tract in women. Clostridium difficile is a representative of normal microflora; it causes colitis and enterocolitis if it multiplies too actively. The toxin produced by the bacterium clostridium perfringens can cause foodborne illness, and the toxin produced by clostridium botulinum causes botulism.
Clostridium septicum
Clostridium septicum was first described in 1877 by L. Pasteur. These bacteria are opportunistic. Under normal conditions, they reside in the human intestine and do not cause disease. In the case of intestinal defects, such as colorectal cancer, the infection damages the intestines and spreads through the blood (hematogenously) throughout the body. Unlike Clostridium perfringens, gas gangrene can occur without prior injury or damage. The infection is more common in people with injuries and burns of the skin, after surgery and septic abortions, peripheral vascular diseases, diabetes, and colon cancer.
The disease develops quickly. Up to 80% of adults die within the first 2 days. Survival rates increase in individuals without concomitant diseases of the lower extremities.
Clostridium septicum affects both humans and domestic animals: large and small livestock.
Morphology
Clostridium septicum is a rod-shaped bacterium. with dimensions 3 - 4 x 1.1 - 1.6 microns. In cultures, filamentous forms of bacteria are sometimes formed, up to 50 microns in length. Motile (have flagella). A capsule is not formed. Gram positive. Over time, clostridia lose this feature. They are strict anaerobes.
Clostridium septicum produces spores. The spores are most often located subterminally, less often - centrally.
Rice. 16. Clostridium septicum under a microscope.
Cultural properties
Clostridium septicum grows well on casein and meat media supplemented with glucose.
- On the surface of glucose-blood agar, bacteria form translucent colonies, shiny, consisting of intertwined threads with a zone of hemolysis along the periphery.
- When growing on 2% agar, the colonies have the appearance of disks.
- When growing on Zeissler agar, after 48 hours, a continuous, delicate coating forms with a zone of hemolysis along the periphery.
- When grown in 1% sugar agar, colonies form in depth. They have a dense center, with intertwining threads extending from the periphery.
- When growing in meat peptone broth, a uniform cloudiness is formed. Further, loose sediment and gas formation are observed.
- When growing on Kitta-Tarozzi medium, bacteria grow with intense gas formation.

Rice. 17. When growing in 1% sugar agar, colonies form in depth. They have a dense center, with intertwining threads extending from the periphery.
Antigenic structure
Clostridium septicum has H and O antigens. The H antigens identify 6 serovars: A, B, C, D, E and F.
Biochemical properties
Clostridium septicum synthesizes a number of enzymes. They live on various organic substrates, including those containing sugars and amino acids, releasing carbon dioxide and molecular hydrogen.
Bacteria ferment some carbohydrates: glucose, maltose and lactose, producing gas and acid. Nitrates are converted to nitrites. They break down proteins releasing ammonia and hydrogen sulfide. Milk curdles slowly under the influence of bacteria. They do not decompose sucrose, glycerin and mannitol. They do not form indole.
3.1. Sanitation / disinfection / sterilization
Sanitation
Sanitation refers to the reduction of the number of microbes through preventive or disinfection measures. Unlike disinfection and sterilization, a prerequisite for sanitation is not a certain or complete reduction in the number of microbes.
Disinfection
Disinfection refers to the destruction or deactivation (irreversible damage) of all disease-causing (pathogenic) microbes, as a result of which there is no longer a risk of infection from the treated objects.
Surface disinfection is carried out in hygiene-sensitive areas such as
- hospitals,
- clinics,
- medical and dental surgery offices,
- microbiological laboratories, etc.
The task and purpose of surface disinfection is to interrupt the path of infection. Microorganisms are destroyed or inactivated by the components of disinfectants.
Treatment
After the analysis reveals clostridia levels above normal, the doctor, taking into account the patient’s age, concomitant diseases, and the presence of allergies, prescribes appropriate therapy. This may include:
- Taking certain antibacterial drugs. Most often this is Metronidazole and its analogues, since it is to this type of drug that bacteria of the Clostridium species are highly sensitive;
- It is advisable to prescribe various types of probiotics (Latculose, Linex, etc.), since they populate the intestines with beneficial bacteria;
- Enzymes (Creon) that promote digestion, as well as bacteriophages, may be prescribed;
- It is possible to prescribe sorbents to remove toxins from the body.
Only a specialist should decipher test results, as well as prescribe medications and determine dosage. Clostridial intestinal infection is a serious problem in which self-medication and resort to folk remedies are unacceptable.
List of references: https://kdl.ru/analizy-i-tseny/issledovanie-kala-na-toksini-klostridiy-clostridium-difficile-aiv https://www.zp.ru/posev-clostridium-difficile.htm https ://www.invitro.ru/analizes/for-doctors/594/2411/ https://propionix.ru/analiz-na-disbakterioz https://citilab.ru/labs/119/services/49/49- 84-104/38131.aspx This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/08/2020
Cause
It is impossible to name a specific reason for the increase in the number of bacteria in the intestines. Most often this is caused by a decrease in human immunity, which causes the uncontrolled reproduction of one or another type of bacteria, including clostridia. Doctors name only a few factors influencing the appearance of clostridiosis:
- The reason may be poor nutrition, namely a high protein content in the human diet. As is known, clostridia perform the function of protein breakdown. Accordingly, in its excess, the number of bacteria also increases;
- Bacteria can enter the human body from the outside. This is due to poor personal hygiene. Therefore, doctors advise teaching children to wash their hands from childhood. It is also necessary to thoroughly wash vegetables and fruits before eating;
- Uncontrolled use of antibiotics, hormonal drugs, and antidepressants can also lead to an increase in the number of pathogenic bacteria. In the modern world, with the development of the Internet and a large number of advertised drugs, many people began to prescribe medications to themselves and take them without consulting a doctor. It is this fact that can affect the intestinal microflora;
- In children, the cause of the proliferation of clostridia, which poses a great danger to the small organism, can be prematurity. In this case, the child’s body is extremely vulnerable;
- Various types of diseases and previous operations can cause a decrease in immunity and provoke the proliferation of bacteria;
- Poor ecology and poor diet have a particularly bad effect on intestinal function.
Stool culture for dysbacteriosis is most often recommended for people who are susceptible to frequent allergies and viral diseases, as well as newborns.
To avoid many diseases, including dysbiosis, it is necessary to monitor your diet, observe hygiene rules and, in case of any changes in the functioning of the intestines, consult a doctor for qualified help.
Classification
To date, more than one hundred species of clostridia have been identified. In medicine, their classification is based on several principles. Based on morphology, the following groups are distinguished:
- rods with a round, terminal spore (C. tetani);
- rods with an oval subterminal spore (C. botulinum);
- with a subterminal or centrally located oval spore (causative agents of gas gangrene).
By type of pathological processes:
- enteral clostridioses (C. botulinum, C. perfringens, C. difficile);
- traumatic and post-traumatic (C. tetani, C. perfringens, C. novyi, C. histolyticum, C. septicum);
- generalized infections: septicemia , sepsis .
Tests and diagnostics
To make a diagnosis, a specialist must study the patient’s medical history, paying attention to whether antibiotic therapy was carried out.
A laboratory test of stool is required to check for the presence of Clostridium difficile and their toxins. If necessary, an endoscopic examination of the large intestine is performed, which reveals characteristic signs - yellowish plaques on the mucosa, a thick layer of overlays, ulcerated areas, which can be important in the process of differential diagnosis. Radiography may be performed.
A blood test is also performed, in which nonspecific changes are noted in the manifest forms of infection.
Clostridia: what is it?
The human body is endowed with many species and a certain number of different bacteria. Their role in the smooth functioning of the whole organism is invaluable. The intestines are equipped with many types of intestinal bacteria, so-called aerobic and anaerobic, that is, those that need oxygen to live, and, accordingly, those that are able to live without oxygen.
In medicine, there are three families of bacteria that live in the intestines:
- So-called “good” bacteria (bifidobacteria, lactobacilli and Escherichia);
- Conditionally pathogenic, which under normal conditions and a certain concentration do not pose any danger (enterococci, staphylococci, clostridia, candida);
- Pathogenic bacteria (Shigella, Salmonella).
Clostridia is one of the opportunistic intestinal bacteria. Normally, clostridia perform the function of processing protein, which enters the intestines along with food. During the processing of protein by clostridia, substances are released - skatole and indole. Their moderate amount does not cause any harm to the body, but rather improves intestinal motility.