Thrombocrit in general blood test
The most accessible method of laboratory diagnosis of thrombocrit and other blood parameters is a general analysis. CCA (general clinical analysis) of blood allows us to identify disturbances in microprocesses in the body, indicating certain possible diseases. Blood, as a biological fluid, consists of plasma and a cellular part containing groups of formed elements: platelets, leukocytes, erythrocytes, etc.
Each group of blood cells is responsible for certain biochemical processes and has its own content norm in quantitative equivalent and percentage of the total blood volume. Basic parameters are assessed according to the reference values accepted in clinical hematology.
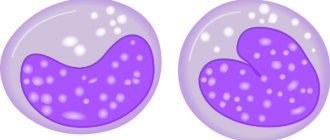
All indicators are correlated, so a comparative interpretation (an increase in some values against the background of a decrease or increase in others) gives the doctor an idea of which system of the body the failure occurred. Platelets are plate-shaped cells without a nucleus or color that are formed in the bone marrow.
The functional responsibility of platelets is to protect blood vessels from damage and ensure normal blood clotting. If a vessel is damaged (serious rupture or microtrauma), flat shaped elements move to the site of the “accident”, form a clot and stop pathological bleeding.
The complexity of the analysis lies in the organic property of blood platelets to stick together (aggregation). To prevent cells from sticking together, the laboratory uses a special automatic analyzer that continuously rotates the blood placed in it. Thrombocrit (platelet mass as a percentage) is studied in combination with other platelet indices:
- platelet count (PLT);
- distribution range (PDW);
- average volume (MPV).
Such a comprehensive study makes it possible to obtain more complete results about the behavior of platelets in the blood composition. As cells increase in size, their distribution range increases, and an increased average value may be associated with hematological diseases, intestinal inflammation, and other pathological processes. An altered platelet count indicates problems with blood clotting and a risk of blood clots. The percentage is calculated using the formula PCT = MPV* PLT.
The PCT blood test deserves increased attention in case of suspected disorders:
- infections of bacterial etiology (origin);
- secondary infectious blood disease (sepsis);
- postoperative pathological processes;
- complicated pregnancy;
- hematological pathologies.
Blood elements to be assessed (briefly)
In relation to other indicators of general analysis, thrombocrit is assessed when monitoring the treatment of meningitis, pneumonia and other diseases of inflammatory origin.
Additionally
To determine platelet indices, venous blood is taken. To obtain objective results, clinical analysis is performed on an empty stomach. Three days before the procedure, the patient is recommended to eliminate heavy fatty foods and alcoholic beverages from the diet. On the eve of the analysis, you should avoid sports training and limit general physical activity. Avoid taking medications that affect blood clotting (antiplatelet agents, coagulants and anticoagulants).
Indications for testing
Platelets (the norm for women by age - the table is attached) are detected using an analysis - this is a standard procedure that is prescribed to all patients. As a result of the study, deviations from acceptable values can be detected and pathology can be identified.
A general or biochemical blood test is prescribed. Based on the data obtained, it is possible to understand how the body functions and what disorders exist. A general blood test measures hemoglobin, leukocytes, red blood cells, and ESR. The platelet level is also assessed.
A general platelet test is prescribed:
- to identify inflammatory processes in the body;
- for blood diseases;
- for allergies;
- in case of a failure in the immune system;
- during pregnancy;
- with varicose veins;
- for problems with blood clotting.
Platelet counts should be checked in the following cases:
- functional liver disorders;
- suffered a heart attack or stroke;
- before treatment with anticoagulants;
- during menopause.
The study is carried out to identify violations in the work of:
- of cardio-vascular system;
- Gastrointestinal tract;
- respiratory organs;
- urinary system.
A blood test for platelets is carried out if there is a suspicion of a malignant tumor, disruption of the endocrine system, or immunological disorders. The analysis can also be done for prevention in order to detect pathological processes in the body.
PCT reference values
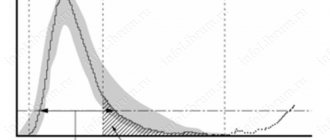
Standard thrombocrit values are not differentiated by the patient’s gender (the indicators are identical for women and men). They also do not have a gradation by age (for adults and children). For all age categories, the norm is from 0.22 to 0.24%.
Reference! Interval values may fluctuate. In the absence of deviations from other analysis indicators, the lower limit is allowed in the range of 0.11% - 0.15%, the upper - 0.28% - 0.4%.
A distinctive feature of platelet indices is the influence of physiological factors on their values, which is not abnormal. In women, in the first seven days of the follicular phase of the menstrual cycle (the period of bleeding), PCT may fall by half. A similar deviation is observed in the perinatal period. In this way, the body tries to reduce the risk of blood clots in the expectant mother.
After intense sports or other physical activity, PLT and PCT levels double. Due to the peculiarities of the body’s biological processes, thrombocrit is usually lower in the spring and at night. The difference between the indicators and the reference values is 10%.
The reason for the low level of indices is the patient’s depressive state and distress (constant neuropsychological tension). All components of the platelet unit (volume, quantity, percentage, range) are interconnected, their values change proportionally to each other.
Platelets in the body
Platelets are platelets of blood 2-5 micrometers in size, formed from megakaryocytes (bone marrow cells). The bodies consist of granules, do not have a nucleus, and the cytoplasm is basophilic. When in normal condition, they have the shape of an oval or circle. Upon contact with the surface of a structure other than the usual environment (endothelium), the plate is activated and forms up to 10 processes, increasing in size. If necessary, the corpuscles cover vascular damage and the bleeding stops.
Both a decrease and an increase in indicators are dangerous for the body.
Symptomatic manifestations of deviations from the norm
An increase or decrease in the percentage in the analysis results are clinical signs of disorders that may be accompanied by the following somatic symptoms:
- CFS (chronic fatigue syndrome);
- pallor (often blueness) of the skin of the fingers;
- bleeding from the nasal cavity (more often observed in children and the elderly).
- tingling sensations, itching in the extremities;
- cephalgic syndrome (headache);
- formation of hematomas on the body of non-traumatic origin;
- decreased visual perception.
Small amounts of blood may be found in urine and feces. You should not self-diagnose. Only a doctor can correctly assess the patient’s condition by comparing test results, medical history and symptoms.
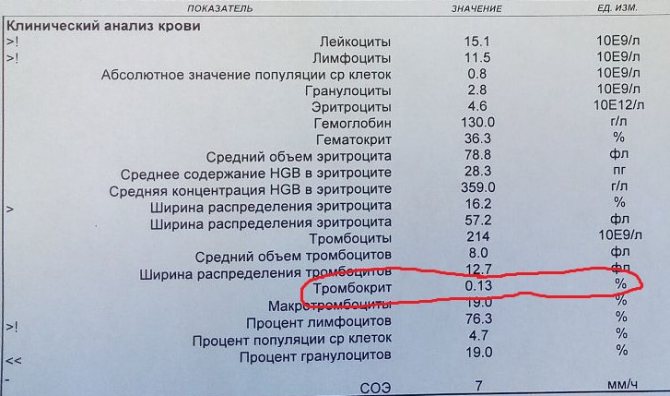
Blood test form with results
Increased level
A high platelet count means increased platelet production, hence thickening of the blood. With this condition of the blood, the risk of heart attack, blood clot formation and vascular blockage (thromboembolism) increases. Elevated levels of all platelet indices accompany the following chronic diseases and acute conditions:
PLT in blood test - what is it?
- chronic myeloproliferative diseases CMPD (transformation of bone marrow cells)
- hematological diseases, including oncological ones (polycythemia, leukemia, Werlhof’s disease, etc.);
- iron deficiency anemia (anemia);
- hyperfunction of the thyroid gland (hyperthyroidism);
- diabetes mellitus and related disease complications - angiopathy;
- infection of the body with bacteria, viruses, fungi;
- atherosclerosis of blood vessels of the lower extremities and brain;
- acute or chronic inflammation of the pancreas;
- infection of the pulmonary system with Koch's bacillus (tuberculosis);
- protein metabolism disorder (amyloidosis);
- pre-stroke and pre-infarction condition;
- systemic inflammation of the connective tissue of the heart and musculoskeletal system (rheumatism).
In women, thrombocrit may be increased due to incorrectly selected hormonal contraception. In children, an increase in PCT levels is often associated with previous viral and colds, or improper nutrition and drinking habits.
As a risk factor for heart attack, high platelet levels are more indicative of men aged 60+. An increase in platelet indices is recorded after surgical interventions, in particular splenectomy (removal of the spleen), as well as after bone fractures. Deviations of PCT results from the norm are provoked by nicotine addiction.
Elevated platelet count: what does it mean?
There are many reasons for the platelet count to go beyond the normal limits established for a woman.
A condition characterized by an increase in the number of blood platelets is called thrombocytosis. This may be a temporary phenomenon (physiological thrombocytosis), not associated with the disease, or permanent, due to the development of the pathological process. An increase in concentration can be caused by:
- myeloproliferative diseases - when the bone marrow produces an increased number of blood cells;
- primary thrombocythemia;
- chronic inflammation - tuberculous, granulomatous, connective (rheumatoid arthritis) or bone tissue (osteomyelitis), small intestine or colon mucosa;
- sarcoidosis;
- diseases of infectious nature;
- hemorrhagic syndrome;
- acute hemolysis - pathological breakdown of red blood cells;
- malignant neoplasms;
- anemia;
- consequence of removal of the spleen (splenectomy);
- excessive dehydration.
Reduced thrombocrit values
The main reasons for a low thrombocrit level are thrombocytopenia (active destruction of platelets and their accelerated removal from the body) and the inability of the bone marrow to synthesize blood cells in the quantity required by the body. Thrombocytopenia provokes anemia of various types:
- Hemolytic. Most often occurs due to incorrect blood transfusion or heavy metal poisoning;
- Pernicious, otherwise Addison-Birmer's disease. Associated with a deficiency of cyanocobalamin (vitamin B12) in the body.
Aplastic anemia is caused by dysfunction of the bone marrow. Low platelet indices are characteristic of:
- a group of diseases with characteristic damage to connective tissue (collagenosis);
- oncohematological diseases;
- state of chronic intoxication of the body;
- cirrhosis;
- renal failure in the decompensated stage;
- pathologies of an autoimmune nature;
- infection with viruses.
A decrease in thrombocrit is a clinical sign of weight deficiency in a newborn baby. In such cases, the baby is prescribed special anti-anemic therapy. An external sign of thrombocrit deficiency is bruising. If hematomas of non-traumatic origin and subcutaneous hemorrhages (hemorrhages) appear on the body, it means that the capillaries in this area are damaged.
To fix the problem, platelets need to block the damaged area. The frequent occurrence of such bruises indicates that blood cells are not coping with the task due to their small number.

Chemotherapy and a course of antibacterial medications can lower PCT levels
Violation of the reference values of platelet indices does not diagnose a specific disease. In case of deviations from the norm, it is necessary to compare the data of all blood test parameters. In case of pronounced changes, the patient needs additional examination, including laboratory microscopy and hardware diagnostic procedures (ultrasound, MRI, CT, etc.).
Significance in diagnosis
First of all, by determining thrombocrit indicators, the following aspects are established:
- Determination of the risk of bleeding, increased thrombosis (thrombocytosis condition).
- Assessment of the benefit/risk ratio when prescribing certain medications.
The most well-known reasons for determining this indicator in the blood are:
- The patient has a high temperature of unknown origin.
- Evaluation of treatment with immunosuppressive drugs.
- Severe viral, bacterial, fungal infection of the body.
- The patient is on artificial ventilation.
- Complications after organ transplantation.
Important. It is necessary to take into account that any change in the number of platelet germ cells - an increase (thrombocytosis), a decrease (thrombocytopenia), a change in shape, aggregation - immediately affects the thrombocrit numbers. To assess the indicators of platelet distribution in peripheral blood, it is necessary to know its normal values
To assess platelet distribution in peripheral blood, it is necessary to know its normal values.
Results
The PCT indicator in the blood test form indicates thrombocrit - the percentage of platelets in the total mass of biological fluid (blood). Platelets are plate-shaped blood cells produced by the bone marrow. Their main function is to prevent bleeding when blood vessels are damaged. In addition to the percentage index, laboratory blood microscopy evaluates the platelet count (PLT), platelet distribution range (PDW) and mean volume (MPV).
The thrombocrit rate for adults and children ranges from 0.15 to 0.4%. A non-pathological decrease in values is the perinatal period and menstruation in women, as well as at night and in the spring season. An increase in the percentage, first of all, characterizes the danger of developing thrombosis, strokes and heart attacks. High PCT values accompany a number of chronic diseases.
A low platelet index indicates thrombocytopenia and insufficient platelet production, which is a clinical sign of anemia, blood cancer, autoimmune and other chronic pathologies. If the study results deviate from the norm, determining the cause of the violation and prescribing appropriate therapy is the responsibility of the attending physician.
Symptoms of a low platelet count
The color indicator of the blood and the reasons for its deviations in tests.
A decrease in the number of platelets in the blood also does not go unnoticed and is expressed in the following symptoms:
- bleeding from the nose;
- the presence of hematomas and their rapid appearance;
- the appearance of blood on the gums when brushing your teeth;
- difficulties in long-term bleeding control in minor injuries;
- pale skin;
- manifestation of hypotension;
- increased heart rate with weak pulse.
If these symptoms were not a consequence of previous blood loss, then this is a likelihood of a disease that requires examination and diagnosis
It is vitally important to establish the reason for this behavior of the body.