HIV 1, 2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
Study of specific antibodies and p24 antigen of the human immunodeficiency virus.
Synonyms Russian
Antibodies to HIV 1, 2, antibodies to human immunodeficiency virus, HIV-1 p24, HIV-1 antigen, p24 antigen.
English synonyms
Anti-HIV, HIV antibodies, human immunodeficiency virus antibodies, HIV-1 p24, HIV-1 Ag, p24-antigen.
Research method
Electrochemiluminescent immunoassay (ECLIA).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Testing for HIV infection can be carried out anonymously and confidentially. During a confidential examination, it is mandatory to present a passport.
- Do not smoke for 30 minutes before the test.
General information about the study
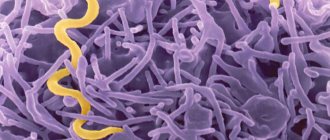
HIV (human immunodeficiency virus) is a virus of the retrovirus family that infects cells of the human immune system (CD4, T helper cells). Causes AIDS.
HIV-1 is the most common type of virus, most often found in Russia, the USA, Europe, Japan and Australia (usually subtype B).
HIV-2 is a rare type, common in West Africa.
To diagnose the human immunodeficiency virus, a fourth-generation combined test system is used, which is capable of detecting HIV infection within 2 weeks after the virus enters the blood, while first-generation test systems do this only 6-12 weeks after infection.
The advantage of this combined HIV test is the detection, thanks to the use of antibodies to HIV-1 p24 as reagents, of the specific p24 antigen (viral capsid protein), which can be detected by this test within 1-4 weeks from the moment of infection, i.e. even before seroconversion, which significantly shortens the “window period”.
In addition, this HIV test detects antibodies to HIV-1 and HIV-2 in the blood (using the antigen-antibody reaction), which are produced in sufficient quantities to be detected by the test system 2-8 weeks after infection.
After seroconversion, antibodies begin to bind to the p24 antigen, resulting in a positive HIV antibody test and a negative p24 test. However, after some time, both antibodies and antigen will be detected in the blood at the same time. At the terminal stage, an AIDS test for antibodies to HIV may give a negative result, since the mechanism of antibody production is disrupted.
Stages of HIV infection
- The incubation period, or “seronegative window period,” is the time from the moment of infection until the development of protective antibodies to the virus in the blood, when tests for antibodies to HIV are negative, but the person can already transmit the virus to other people. The duration of this period is from 2 weeks to 6 months.
- The period of acute HIV infection begins on average 2-4 weeks from the moment of infection and lasts approximately 2-3 weeks. At this stage, some people may develop nonspecific flu-like symptoms due to active replication of the virus.
- The latent stage is asymptomatic, but during it there is a gradual decrease in immunity and an increase in the amount of virus in the blood.
- AIDS (acquired immunodeficiency syndrome) is the final stage of development of HIV infection, which is characterized by severe suppression of the immune system, as well as concomitant diseases, encephalopathy or cancer.
Despite the fact that HIV infection is incurable, today there is highly active antiretroviral therapy (ART), which can significantly prolong the life of an HIV-infected person and improve its quality.
This test has a particularly high diagnostic value if HIV infection occurred shortly before the time of testing (2-4 weeks).
What is the research used for?
The analysis is used for early diagnosis of HIV, which allows preventing further transmission of the virus to other people, as well as timely initiation of antiretroviral therapy and treatment of diseases that contribute to the progression of HIV infection.
When is the study scheduled?
- With persistent symptoms (for 2-3 weeks) of unknown etiology: low-grade fever, diarrhea, night sweats, sudden weight loss, enlarged lymph nodes.
- For recurrent herpes infection, viral hepatitis, pneumonia, tuberculosis, toxoplasmosis.
- If the patient suffers from sexually transmitted diseases (syphilis, chlamydia, gonorrhea, genital herpes, bacterial vaginosis).
- If the patient has had unprotected vaginal, anal or oral sex with multiple sexual partners, a new partner, or a partner whose HIV status the patient is not sure of.
- When the patient underwent a donor blood transfusion (although cases of infection in this way are practically excluded, since the blood is carefully tested for the presence of viral particles and is subjected to special heat treatment).
- If the patient injected drugs using unsterile instruments.
- During pregnancy/planning pregnancy (taking azidothymidine during pregnancy, caesarean section to avoid transmission of the virus to the baby during passage through the birth canal, and avoiding breastfeeding reduces the risk of mother-to-child transmission of HIV from 30% to 1%).
- Accidental injection with a syringe or other object (for example, a medical instrument) containing infected blood (in such cases the likelihood of infection is extremely low).
What do the results mean?
Reference values
Result: negative.
Reasons for negative results:
- absence of HIV infection,
- the period of the seronegative window (neither the antigen nor the antibodies have yet been developed in sufficient quantities necessary for detection by the test system).
Reasons for the positive result:
- HIV infection.
Important Notes
- Diagnosis of HIV antibodies in infants born to HIV-infected mothers is difficult, since the infant receives antibodies from the mother through placental blood. As a rule, the test for HIV antibodies in such children becomes negative no later than 18 months, if the child is not infected with HIV.
- This HIV test cannot determine how long ago you were infected or the stage of HIV (for example, AIDS).
- HIV is found in almost all body fluids, but only in blood, semen and vaginal secretions is the concentration of the virus sufficient for infection. In addition, the virus is unstable and can only live in liquid environments of the human body, so HIV infection is not transmitted through kissing, insect bites and household contact (for example, when using a shared toilet, through saliva, water and food).
- This HIV test, although it shortens the “window period,” is still able to determine the presence of antigen/antibodies no earlier than 1-3 weeks from the moment of possible infection.
- If an event that threatens HIV infection occurs less than 1-3 weeks before testing, it is recommended to repeat the test.
- First- and third-generation tests could give a false-positive result if antibodies to the Epstein-Barr virus, rheumatoid factor, HLA major histocompatibility complex, or antibodies after administration of an HIV vaccine were present in the patient’s blood. However, the likelihood of a false positive result with a combined test is virtually eliminated.
- In case of a positive test result, a confirmatory analysis is performed using the immunoblotting method (a test for antibodies to a number of specific proteins of the virus).
Who orders the study?
General practitioner, therapist, infectious disease specialist, dermatovenerologist.
HIV virus - possible routes of infection
The content of the article
The HIV virus (human immunodeficiency virus) is a type of lentivirus - these viruses cause disease after a long latent phase. So far, two variants of HIV have been identified - HIV-1 (present throughout the world) and HIV-2 (found mainly in West Africans, damages the host’s immune system much more slowly compared to HIV-1). You can become infected with HIV in several ways:
- through blood - for example, through blood transfusions, organ transplants, using needles contaminated with the blood of people infected with the virus,
- through sexual contact - vaginal, oral and anal
- from the carrier mother to the child - through the placenta during pregnancy, childbirth and breastfeeding.
However, household contacts (excluding sexual contacts) do not pose a danger if we follow basic hygiene rules - HIV is not transmitted by airborne droplets (sneezing, coughing), touching, using the same cutlery or dishes.
Test results
There are many reasons to test for the presence of HIV infection in the body.
An upcoming operation, planning a pregnancy, a history of casual sex and other similar reasons.
There are categories of workers (for example, medical workers, teachers and others) for whom this procedure is necessary in order to be allowed to work with people.
There are certain alarming symptoms in which an HIV test is carried out:
- with sudden weight loss
- for prolonged diarrhea (about 3 weeks)
- with fever of unknown etiology
- with the growth of lymph nodes in different places
- for lympho- and leukopenia
- in the presence of unexplained pneumonia, systemic candidiasis, tuberculosis, manifest toxoplasmosis and other serious diseases
Only the attending physician is responsible for interpreting the results of the tests performed.
Whatever the result, this is not a reason to engage in treatment on your own.
In addition, the result, due to the imperfection of the method, can be either false negative or false positive.
Sometimes similar test results in different people indicate a different clinic.
Quantitative PCR analysis for HIV infection is often done.
This test provides information about the amount of virus and is displayed as a copy/ml unit.
Decoding the results:
- There is no or very little viral RNA (about 20 copies/ml)
- a tiny amount of RNA (slightly more than 20 copies/ml)
- 20 – 106 copies/ml
- more than 106 copies/ml
The most dangerous are the third and fourth results.
How to determine HIV infection?
There are many more carriers of the infection than we think, because due to the asymptomatic course of the infection, it is difficult to diagnose it at an early stage.
Most people assume that they certainly don't care about their HIV status, so they don't take screening tests - this assumption is clearly false, because each of us can be a carrier of the virus. Not knowing about the infection poses a threat not only to our health, but also to the health of others, so it is important to detect the infection at an early stage.
HIV screening involves a laboratory test of a blood sample for the presence of p24 antigen, which is specific to the virus. The p24 antigen is detected in the carrier's blood as early as 4 weeks after infection (its concentration increases and decreases with increasing HIV levels), and antibodies after 12 weeks - immediately after this time from the moment of potential infection, it is recommended to undergo a test.
HIV screening
The test result may be negative (negative, is not a carrier) or positive (positive, is a carrier). All positive results of screening tests must be confirmed by Western blotting - only a positive result from this test allows us to conclude that the patient is truly HIV positive.
HIV carrier status can affect anyone - HIV testing should be carried out:
- in people who have ever had sexual contact with someone with an uncertain serostatus (serostatus must be confirmed by an appropriate test) or with HIV-infected people;
- all pregnant women and women planning pregnancy;
- people who inject drugs or other substances by sharing syringes and needles, or who have received tattoos or piercings with non-sterile equipment.
How to prepare?
You need to prepare for an HIV/AIDS test. Blood should be donated on an empty stomach, and the last meal should take place no later than 8 hours before. Naturally, it is recommended to maintain a unique diet, a few days before donating blood, giving up alcohol and “harmful” foods - fatty, fried, smoked foods, marinades and other refined foods.
It is worth considering that if you are unwell, even with any viral or infectious disease, it is better not to donate blood or come back for testing again 35-40 days after recovery. Otherwise, there is a risk of getting a false positive result.
The HIV/AIDS test goes through several stages of testing. Therefore, it takes 2-10 days to prepare.
HIV infection - treatment and prevention
Confirmation of HIV infection is critical because it allows the use of appropriate antiretroviral drugs - they do not completely eliminate HIV from the body, but they do prevent it from reproducing and thus significantly prolong the lives of infected people, ensuring good health for many years (studies show that people who take antiretroviral therapy for about 30 years do not develop symptoms of infection).
Since there is still no cure to completely eliminate HIV, proper infection prevention is of utmost importance. Preventive measures include: appropriate education, avoidance of sexual contact with people of unknown serostatus or HIV-infected people, use of condoms, avoidance of intoxicants, good personal hygiene (do not share, for example, razors, toothbrushes with others), tattoos / piercing, etc. in safe recommended salons and regular HIV screening.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
HIV infection and sexual intercourse
Sexual contact is the most common cause of HIV infection worldwide. The risk of infection depends on where you are infected and the viremia (amount of virus) in your body. The higher the viral load, the higher the risk of transmitting the virus to a sexual partner. It is estimated that the risk of contracting the virus is 10 times higher during acute HIV infection (soon after infection) compared to the asymptomatic carrier stage.
HIV is much more easily transmitted from man to woman than from woman to man - this is due to the different anatomy of the female and male genital organs, as well as the higher concentration of HIV in semen compared to its concentration in the female genital organs.
HIV infection and sexual intercourse
The risk of transmitting the virus also depends on the frequency of sexual intercourse with an infected person and the use of safety measures - more frequent sexual contact means a greater risk of infection, and protection in the form of a condom significantly reduces it (but does not eliminate it completely).
The likelihood of contracting HIV is also affected by the type of sexual activity - the most dangerous is anal intercourse (both homosexual and heterosexual). Oral contact has a low risk of transmitting the virus, but there have been reports of transmission through this route, so this type of sexual activity cannot be considered safe.
Vaginal contact means that a woman is more likely to become infected than a man, and this risk increases with contact during menstruation (for both sexes). Research also shows that postmenopausal women are at higher risk of contracting HIV.
Additionally, it should be emphasized that a small portion of the population is nearly immune to AISD. The CCR5 gene is responsible for one of the coreceptors that allow the virus to enter the cell. One of the variants of this gene does not allow the synthesis of a coreceptor, so the body is resistant to HIV infection (in whole or in part).
Positive HIV test - what does it mean and how is it reported?
Often, negligent behavior of medical workers can cause infection: improper disinfection of equipment, reuse of needles, and other things can lead to infection of both the worker and hospital patients. In order to take timely measures to prevent the disease, a blood test is taken from any inpatient patient at the beginning and at the end of the treatment period. In this case, the analysis is carried out anonymously (the person does not know about it). The patient will be informed of the results only if a positive test has been received.
Advice! Since the period of treatment in the hospital does not exceed the incubation period of HIV, and the amount of antibodies to the virus in the body is not enough to detect them, it is recommended to be tested after each period of hospital treatment. Especially if surgery was performed.
At the end of the treatment period, the test is carried out not to determine the infection in the hospital, but to check whether the disease has become active during this treatment period.
If the ELISA test is positive
When a person receives a positive ELISA test for HIV, they should immediately contact their doctor. Only a specialist doctor can make a final verdict on the presence or absence of HIV infection based on an accurate study. In all cases where the ELISA is positive, a repeat PCR test is prescribed to determine the amount of virus. Based on a set of data, the doctor makes a conclusion about the speed of the disease and the characteristics of the development of the virus.
Advice! You cannot abandon further examination at the first positive result. Sometimes this result is caused by improper preparation and execution of the test.
What to do if the ELISA is positive
If the analysis shows the presence of a virus, it is recommended to do a second analysis
ELISA results are considered reliable only after repeated analysis and confirmation of the result.
If you receive a positive test, you should consult your doctor. If only one of a number of tests turns out to be positive, the analysis should be repeated after a few weeks to obtain reliable data.
The cause of an erroneous result may be traces of blood from a previous test.
Complications during tests
Many diseases can contribute to obtaining inaccurate data:
- Thyroid diseases;
- Chronic colds;
- Presence of parasites.
Such deviations in health do not allow detection of the viral trace by ELISA. Patients are prescribed other types of diagnostics.
What to do if the result is negative
Do not forget that the deadline for taking the test may fall during the seronegative window, when the activity of the virus is reduced and it is not detected. In order to get a reliable result, it is necessary to repeat the analysis after a few weeks.
You cannot bring your own blood for analysis, since the protein that is detected by ELISA quickly denatures, which will contribute to obtaining a negative result.
One way to detect virus cells during the window period is PCR. Before this analysis, a polymerase chain reaction is performed, which increases the number of RNA segments, which will make the drug more accessible for analysis.